Introduction
Hangman’s fracture is the spondylolisthesis at the C2-3 level following bilateral fractures of the pars interarticularis of the axis. Traumatic spondylolisthesis of the axis, though first described in 1866, the term “Hangman's fracture” was coined in 1965.[1] It is the second most common fracture type involving C2 vertebrae after odontoid fractures and represents approximately 4-20% of all cervical fractures.[2][3][4]Steele’s rule of thirds states that the cross-sectional area at the atlas level may be divided into three equally represented parts: the dens, space, and the spinal cord. This increased area for the spinal cord at this level allows for the relative lack of neurologic injury associated with a hangman’s fracture.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Schneider et al. coined the term hangman’s fracture in 1965. Despite the term implying a hyperextension and distraction injury, such as in the case of a judicial hanging, the more common mechanism of action is hyperextension and axial loading.[6] These injuries are most commonly seen in motor vehicle accidents, diving injuries, or contact sports.
Epidemiology
Fractures of the cervical spine are present in 1% to 3% of all trauma cases, of which 9% to 18% are of the C2 vertebrae. The incidence of C2 fractures has doubled from 3 per 100,000 to 6 per 100,000 from 1997 to 2014 in data reported from the Swedish National Patient Registry. Fractures of the odontoid process are much more common, representing 35% to 78% of all C2 fractures in the general population and 89% of patients older than 70 years old. Meanwhile, hangman’s fractures represent 11% to 25% of all C2 vertebrae fractures.[7] In a study comprising 58 patients, the mean age of the cohorts was 62.7 ± 25 years, with male to female ratio of 1:1.2. Motor vehicle accidents accounted for the most common cause of the same.[2]
Pathophysiology
It is vitally important to keep in mind the unique anatomy of the atlas-axis complex when treating their associated injuries. Unlike the subaxial cervical spine, the C1 to C2 complex does not contain an intervertebral disc; there are unique ligaments that allow for support of the cranium and provide the majority of cervical rotation. There is also a close relationship between the transverse foramen, which carries the vertebral artery through the cervical spine, with the C2 pedicle/pars interarticularis, which may slightly weaken this area allowing for a fracture to occur.
Two hypotheses have been presented for the pathogenesis of Hangman’s fracture:
- Internal gear hypothesis: The presence of a trabeculae void and acute transition from the bi-columnar to tri-columnar unit places the isthmus of the Axis at increased risk of injury
- Leaf spring hypothesis: C2 pedicle is like the shackle in the assembly and therefore the weak link within the same.[3]
The extension compression subtype of Hangman's fracture results from pincer-like compression of the C2 pedicle between adjoining articular processes of C1 and C3. The flexion subtype of Hangman's fracture results following the bending failure of the pedicle over the fulcrum formed by the superior facet of C3.[3] The flexion type of injury harbingers the risk of injury to the C2–C3 disc anteriorly and C1–C2 posterior ligament complex (PLC) posteriorly.[3]
Multiple grading systems for hangman’s fractures exist; however, the Levine and Edwards classifications are the most widely used.
Levine and Edwards Classification
Specifics
Angulation in this system is measured as the angle between the inferior endplate of C2 and C3. Anterior subluxation of C2 on C3 greater than 3 mm is a marker for C2 to C3 intervertebral disc disruption. It is important to recognize that this grading system does not apply to the pediatric population.[8]
Grading
- Type 1: Less than 3 mm subluxation of C2 on C3, due to axial loading, stable, rigid cervical collar treatment
- Type 2: Disruption of the C2 to C3 disc, posterior longitudinal ligament, greater than 4 mm subluxation, greater than 11 degrees angulation, less than 5 mm requires a reduction in axial traction and halo fixation for 6 to 12 weeks while that greater than 5 mm can require surgery
- Type 2a: Less displacement more angular deformity, flexion injury, unstable, not suitable for axial traction, treatment in halo
- Type 3: C2 to C3 facet capsule disrupted, anterior longitudinal ligament disruption, unstable, may have a deficit, surgical candidates
Francis Grading System
Specifics
Two factors are considered for the Francis Grading system: angulation and displacement. Angulation is measured by the degree of anterior angulation off the posterior vertebral line drawn straight from the C3 vertebral body. The magnitude of anterolisthesis that measures displacement is graded as either greater than or less than 3.5 mm.[9]
Grading
- Type 1: Less than 11 degrees of angulation and less than 3.5 mm of displacement
- Type 2: Greater than 11 degrees of angulation and less than 3.5 mm of displacement
- Type 3: Less than 11 degrees of angulation and greater than 3.5 mm displacement
- Type 4: Greater than 11 degrees of angulation and greater than 3.5 mm of displacement
- Type 5: Complete disc disruption
Typical versus Atypical Fractures
It is important to recognize that not all C2, hangman’s type fractures can be described using these classification systems. A typical hangman’s fracture allows for the separation of the anterior elements from the posterior elements of the C2 vertebrae, therefore increasing the available space for the spinal cord. However, in the case of an atypical hangman’s fracture, the posterior aspect of the C2 vertebral body, not the bilateral pars, is involved. This leads to a higher risk of neurologic injury as the space remaining for the spinal cord does not increase secondary to the fracture.
Typical "Hangman's fractures" lead to the separation of the neural arch from C2 bilaterally.[10]
Atypical Hangman's fractures include:
History and Physical
It is important to recognize that outside of the obvious motor vehicle collisions and high-impact falls, low-energy and blunt trauma, especially in the elderly population, can induce significant unstable injury. History should also entertain fracture risk factors such as osteoporosis, metastatic burden, or vitamin D deficiencies. Physical exam findings include pain with palpation in the posterior portion of the neck, radiculopathy, myelopathy, and possible posterior fossa findings secondary to vertebral artery injury. A strict neurologic exam including cranial nerves, sensory, motor, and rectal tone is mandatory.
Evaluation
Laboratory tests should be ordered as an adjunct to overall medical status. Normalized hemoglobin, hematocrit, PT/PTT, INR, and platelet counts will be needed for operative intervention.
X-ray
Evaluation with X-rays will provide limited but important information. Care must be taken to ensure proper radiographic imaging creates a picture from the occiput to the C7 through the T1 disc space. This is essential in reviewing cervical spine trauma. Lateral, anteroposterior (AP), and open-mouth odontoid views are necessary. Approximately 93% of cervical spine injuries appear with combined, lateral, AP, and odontoid view radiographs. X-rays are an excellent modality for determining alignment during the immediate injury, post-operative period, as well as long-term follow-up.
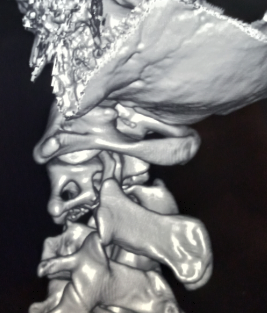
CT Scan
Computed tomography is the mainstay of radio imaging.[10] CT scan is the most important modality for determining fracture etiology and ruling out an injury regarding a C2 fracture. A CT scan is warranted even if plain films are negative and clinical suspicion is high. CT scan does not directly evaluate the spinal cord, soft tissue, or ligamentous construct. It is important to recognize the importance that complete imaging will require dedicated thin-cut CT reconstructions. Non-contrast CT scan is adequate for evaluating the bony anatomy for fracture. This can be coupled with a CT angiogram (see below) for evaluation of the vascular anatomy.
MRI
Evaluation with MRI is essential for analyzing the ligamentous construct, disc space, spinal cord, nerve roots, and other soft tissue injuries. MRI is also useful for determining the acute nature of the fracture when this is otherwise unknown. This is done via non-contrasted imaging. T2 signal hyperintensities and STIR changes within the dens, ligaments, or soft tissue can illustrate a critical component. MRI is less dangerous than flexion-extension cervical injury.
The Effendi, Levine, and Francis classifications are solely based on static radiographs.[1] The management algorithm however is also dependent upon the integrity of the C2/3 disc, the anterior and the posterior longitudinal ligaments.[10] The MRI is an important armamentarium to connote concurrent instability which is determined by:
- C2-3 angulation of ≥11°.
- C2-3 translation of ≥3.5 mm.
- Teardrop fracture involving C2 or C3.
- Associated C disco-ligamentous injury.[1][15]
Vascular Imaging
Vascular imaging may be indicated. The vertebral artery’s second segment (V2) runs through the transverse foramen of C2 to C6, while V3 runs extradurally, exiting the C2 foramen across the sulcus arteriosus. This can place it at risk for injury. Indeed, in one series, 15% of patients with C1 to C2 fractures had vertebral artery injuries. Of which, type-III odontoid fractures posed the greatest risk. It is important to note that an untreated vertebral artery injury has a 24% stroke rate. CT angiography can be coupled to CT imaging upon fracture evaluation with consideration of kidney function. Level-III evidence suggests that patients with C1 to C3 fractures can be screened with multi-slice multi-detector CT angiography. At this time, MR angiography cannot be listed as the sole imaging modality for the evaluation of vertebral artery injury. The first-line investigation with percutaneous angiography is overly aggressive.[16][17]
Treatment / Management
Treatment options include conservative management, cervical orthosis, halo-vest orthosis, and surgical procedures.
External Fixation
A rigid cervical collar represents the immediate first treatment. Nonunion may occur as frequently as 50% of odontoid fractures, but nonunion is rare in hangman’s fractures, with approximately 90% healing with immobilization alone. Level III evidence shows that a hangman’s fracture may be initially managed with immobilization with a halo-vest or collar alone. This produces a reduction rate of 97% to 100% and a fusion rate of 93% to 100%. External orthosis should be maintained for 8 to 14 weeks. It is important to remember that halo-vest orthosis is not very well tolerated in the elderly population, and therefore collar is recommended as first-line management.[18][19][20](B3)
Non-operative treatment is advocated for extension type Levine-Edwards type I and type II hangman's fracture whereas flexion type Levine type IIa and type III fractures invariably require surgical intervention.[2][4][10][21](B2)
A systematic review has shown that conservative treatment failed sequentially for Levine-Edward's type I (fusion rate of almost 100%) to III fractures (fusion rate of only 30%).[1] This approach is also time-consuming and harbingers high-risk risks of nonunion. In one study comprising 625 patients who were managed with halo-vest immobilization (HVI), cohorts aged>80 had higher risks of complications, mortality, and readmissions. [22] Another similar study comprising 189 patients with 71.1% sustaining C2 fractures and managed with halos showed a mortality of 8.3%, a failure rate of 10.7%, and a complication rate of 46.3%.[23]
Internal Fixation
Surgical fixation may be considered in the following scenarios:
- Severe angulation of C2 on C3 (Francis II and IV, Levine II).
- Disruption of the C2 to C3 disc space (Francis V, Levine II).
- Anterior displacement of C2 greater than 50% on C3.
- Inability to establish or maintain alignment with external immobilization.
- Nonunion after the use of external immobilization.
The main mandate of surgical intervention is to achieve early anatomical stability while preserving the maximum range of neck movements.[24]
Abnormal angulations and incomplete reduction impair biomechanical loading thereby leading to a heightened risk for persistent neck pain, nonunion, and implant failure.[1]
The different patterns of surgical strategies include:
- Halo traction.
- Anterior stand-alone fusion.
- Posterior stand-alone fusion, and
- Global (anterior-posterior) fusion.[1]
Internal fixation can be achieved via anterior fixation or by a variety of posterior constructs.
Anterior
C2 to C3 anterior cervical discectomy and fusion may be used with anterior plating to stabilize the C2 to C3 vertebral bodies. The main benefit of the anterior approach is preserving the C1 motion, which drastically decreases the morbidity compared to posterior fixation.[9]
Posterior
- C1 to C2 transarticular screws
- C1 lateral mass and C2 pedicle screws
- C1 lateral mass and C2 pars interarticularis screws
- C1 to C2 wiring (also as an adjunct technique)
- Extension to C3 lateral mass if there is a disruption of the C2 to C3 intervertebral disc or facet joint capsules.[25] (A1)
Posterior fixation technique selection requires significant review by a neurosurgeon or orthopedic spine surgeon. It considers a variety of factors, including surgeon experience, fracture location, vertebral artery location, biomechanical suitability, and anatomical variations. Vascular imaging is mandatory to illustrate the location of the vertebral artery in the V2 and V3 segments. The patient’s overall functional status, medical optimization, and bone health must be evaluated in the operative decision-making.
Flexion injury damaging the posterior ligamentous complex requires C1–2 posterior fixation per the tension band law. The extension injury needs either anterior or posterior C2–3 fixations.[3] Levine-Edwards type II fractures are mostly managed by anterior C2/3 fusion.[10] Levine-Edwards type III fractures, if reducible following traction, can be managed by anterior C2/3 fusion. If irreducible, they most often have to undergo posterior fusion.[10] They may necessitate global fixation.[1] An anterior stand-alone approach with a longer cantilever beam technique to include C4 has also been shown to achieve good reduction and stability for Levine Edward's Type III Hangman's fractures.[1] The prerequisites for posterior pars screw fixation include reduction of fracture translation to <3 mm, and intact anterior longitudinal ligament.[1] However, pars screws should have concurrent C3 lateral mass fixation for type II fractures. This also hampers C1-2 motion and cannot address the anterior disc.[1] Anterior fixation is advocated in C2-3 disc disruption. C3 corpectomy may be required to decompress the cord.[1][26] The accuracy of screw placements can be enhanced by newer adjuncts such as Robot-assisted methods and intra-operative navigation systems.[24][27][28][29] The course and the integrity of the vertebral artery can be ascertained by preoperative angiography.[10] The intraoperative risk of arterial injury can be nullified by the use of color-coded duplex ultrasound.[30][31] C2 spinous muscle complex graft, compared to iliac bone, minimize donor site morbidities and complications.[32] A zero profile minimizes dysphagia and spares the motion at the atlantoaxial joint.[33] C2 pedicle reformation (osteosynthesis with Herbert's compression and lag screws) preserves neck movements.[34][35] A longer construct encompassing C4 might be required to prevent kyphosis.[36][37] The posterior approach has a better recovery of cervical sagittal balance compared to the anterior approach.[38] Minimally invasive approaches have also been described through tubular retractor systems aided with neuronavigation.[39][40](B3)
Hangman's fractures most often show excellent clinical outcomes.[4] Management of Hangman's fracture has low risks of mortality and procuring neurological complications.[21](B2)
Differential Diagnosis
Differential diagnoses include pseudosubluxation (generally C2 on C3) and the Mach effect.
Prognosis
Successful repair of the fractured bone(s) can lead to excellent recoveries with a good long-term prognosis. Some cases require fusion of the C2 and C3 vertebrae. Researchers studied fusion surgery performed via the posterior approach; this method demonstrated excellent results in 3-part fractures of the axis.[41]
In another study of over 30 people with a hangman’s fracture, researchers found that 85 percent of patients with a hangman's fracture experienced a full recovery within a year.[42]
Complications
Complications of the Hangman's fracture include:
- Vertebral artery arteriovenous fistula (AVF).[43][44]
- Occlusion and dissection of the vertebral artery.[45][46]
- Brown-Sequard syndrome (BSS).[47]
- Concurrent spinal cord injury especially in atypical, Type IIa, and III fractures.[2]
Complications of different management strategies include:
- Post-operative dysphagia has a reported incidence of 22.6% in 1st week and 9.7% at 3 months. The risk is higher with anterior plating and minimized with zero profile implants.
- Post-operative dysphonia has a reported incidence of 24.5% in 1st week and 3.8% at 3 months.[48]
- Intraoperative vertebral artery injury.[30]
- Halos complications include pin site infections, loosening of the pins, and restricted neck movements.
Deterrence and Patient Education
Patients need to understand that most cases will not require surgery. They may need to wear a neck collar to limit movement to promote healing and prevent further injury. More commonly, they will require halo immobilization.
Less commonly, the patient will require surgery. All aspects of the procedure need to be explained to the patient, and they should receive reassurance regarding the high degree of successful recovery following surgery, as cited above. They should also be given realistic expectations regarding recovery time, lasting as long as a year.
Pearls and Other Issues
- A rigid cervical collar should be immediately placed in the emergency room setting.
- The majority of Hangman’s fractures may be successfully treated with external orthosis alone.
- Vascular imaging should be performed in all C1 to C3 fractures.
Enhancing Healthcare Team Outcomes
Fractures of the spine are best managed by an interprofessional team that includes clinicians (including PAs and NPs), specialists (orthopedists, neurologists), orthopedic and neurology nurses, and therapists. Physical therapy may play a role in rehabilitative recovery in surgical and non-surgical cases. This interprofessional approach will result in improved patient outcomes. [Level 5]
Clinicians should be aware that imaging is critical for the diagnosis of a hangman's fracture. CT scan is the most important modality for determining fracture etiology and ruling out an injury regarding a C2 fracture. Even if plain films are negative and clinical suspicion is high, a CT scan is warranted. CT scan does not directly evaluate the spinal cord, soft tissue, or ligamentous construct. It is important to recognize the importance that complete imaging will require dedicated thin-cut CT reconstructions. Non-contrast CT scan is adequate for evaluating the bony anatomy for fracture. This can be coupled with a CT angiogram for evaluation of the vascular anatomy. A missed injury can prove fatal.
Most patients can be managed with external support, and full recovery is possible with time.[49]
Media
(Click Image to Enlarge)
References
Mudumba VS,Pavan S,Alugolu R, Saradhi's single stage, anterior sequential reduction utilizing C3 for type III hangman's fracture: A novel technique. Journal of craniovertebral junction & spine. 2022 Jan-Mar [PubMed PMID: 35386244]
Cai Y,Khanpara S,Timaran D,Spence S,McCarty J,Aein A,Nunez L,Arevalo O,Riascos R, Traumatic spondylolisthesis of axis: clinical and imaging experience at a level one trauma center. Emergency radiology. 2022 Aug [PubMed PMID: 35543854]
Menon VK, Mechanically Relevant Anatomy of the Axis Vertebra and Its Relation to Hangman's Fracture: An Illustrated Essay. Neurospine. 2019 Jun [PubMed PMID: 31261461]
Turtle J,Kantor A,Spina NT,France JC,Lawrence BD, Hangman's Fracture. Clinical spine surgery. 2020 Nov [PubMed PMID: 33044269]
Spence KF Jr,Decker S,Sell KW, Bursting atlantal fracture associated with rupture of the transverse ligament. The Journal of bone and joint surgery. American volume. 1970 Apr [PubMed PMID: 5425648]
SCHNEIDER RC,LIVINGSTON KE,CAVE AJ,HAMILTON G, [PubMed PMID: 14288425]
Robinson AL,Olerud C,Robinson Y, Epidemiology of C2 Fractures in the 21st Century: A National Registry Cohort Study of 6,370 Patients from 1997 to 2014. Advances in orthopedics. 2017 [PubMed PMID: 29181200]
Level 3 (low-level) evidenceLevine AM,Edwards CC, The management of traumatic spondylolisthesis of the axis. The Journal of bone and joint surgery. American volume. 1985 Feb [PubMed PMID: 3968113]
Francis WR,Fielding JW,Hawkins RJ,Pepin J,Hensinger R, Traumatic spondylolisthesis of the axis. The Journal of bone and joint surgery. British volume. 1981 [PubMed PMID: 7263740]
Scholz M,Kandziora F,Kobbe P,Matschke S,Schleicher P,Josten C,Spine Section of the German Society for Orthopaedics and Trauma, Treatment of Axis Ring Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global spine journal. 2018 Sep [PubMed PMID: 30210957]
Pinter ZW,Lawson BK,Freedman BA,Sebastian AS, Atypical hangman's fracture with concomitant subaxial fracture-dislocation treated with circumferential fusion of C2-C5-a case report. Spinal cord series and cases. 2020 Dec 2 [PubMed PMID: 33268764]
Level 3 (low-level) evidencePrasad GL, Traumatic irreducible non-Hangman's type bilateral C2-C3 high-grade facet dislocation: technical nuance. British journal of neurosurgery. 2020 Dec 2 [PubMed PMID: 33263442]
Jain S,Mishra K,Gandhi A,Garg D, Curious Case of Atypical Hangman's Fracture: C2-C3 Listhesis without Pars Fracture. Journal of neurosciences in rural practice. 2020 Oct [PubMed PMID: 33144811]
Level 3 (low-level) evidenceAljuboori Z,Hoz S,Boakye M, Failure of C2-3 anterior arthrodesis for the treatment of atypical Hangman's fractures: A three case series. Surgical neurology international. 2020 [PubMed PMID: 32257578]
Level 2 (mid-level) evidenceKim SK,Rhee JM,Park ET,Seo HY, Surgical Outcomes for C(2) Tear Drop Fractures: Clinical Relevance to Hangman's Fracture and C(2-3) Discoligamentous Injury. Orthopaedic surgery. 2021 Dec [PubMed PMID: 34791834]
Gupta P,Kumar A,Gamangatti S, Mechanism and patterns of cervical spine fractures-dislocations in vertebral artery injury. Journal of craniovertebral junction [PubMed PMID: 23741123]
Pratt H,Davies E,King L, Traumatic injuries of the c1/c2 complex: computed tomographic imaging appearances. Current problems in diagnostic radiology. 2008 Jan-Feb [PubMed PMID: 18054664]
Tuite GF,Papadopoulos SM,Sonntag VK, Caspar plate fixation for the treatment of complex hangman's fractures. Neurosurgery. 1992 May [PubMed PMID: 1584391]
Coric D,Wilson JA,Kelly DL Jr, Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. Journal of neurosurgery. 1996 Oct [PubMed PMID: 8814154]
Level 3 (low-level) evidenceSonntag VK,Hadley MN, Nonoperative management of cervical spine injuries. Clinical neurosurgery. 1988 [PubMed PMID: 3288418]
Prost S,Barrey C,Blondel B,Fuentes S,Barresi L,Nicot B,Challier V,Lleu M,Godard J,Kouyoumdjian P,Lonjon N,Marinho P,Freitas E,Schuller S,Allia J,Berthiller J,Charles YP,French Society for Spine Surgery (SFCR), Hangman's fracture: Management strategy and healing rate in a prospective multi-centre observational study of 34 patients. Orthopaedics & traumatology, surgery & research : OTSR. 2019 Jun [PubMed PMID: 31005699]
Level 2 (mid-level) evidenceKurucan E,Sulovari A,Thirukumaran C,Greenstein A,Molinari R,Mesfin A, Volume-outcome relationship in halo vest utilization for C2 fractures. The spine journal : official journal of the North American Spine Society. 2020 Oct; [PubMed PMID: 32474222]
Isidro S,Molinari R,Ikpeze T,Hernandez C,Mahmoudi MS,Mesfin A, Outcomes of Halo Immobilization for Cervical Spine Fractures. Global spine journal. 2019 Aug [PubMed PMID: 31431875]
Verma S,Singh PK,Agrawal M,Sawarkar D,Borkar SA,Kumar A,Garg K,Agrawal D,Gupta D,Satyarthee G,Chandra SP,Kale SS, Use of Intraoperative Imaging to Preserve C1-C2 Mobility in Complex Atlas-Hangman Fractures. Neurology India. 2022 Jan-Feb [PubMed PMID: 35263885]
Menger RP,Storey CM,Nixon MK,Haydel J,Nanda A,Sin A, Placement of C1 Pedicle Screws Using Minimal Exposure: Radiographic, Clinical, and Literature Validation. International journal of spine surgery. 2015 [PubMed PMID: 26484006]
Level 1 (high-level) evidencePatel JYK,Kundnani VG,Kuriya S,Raut S,Meena M, Unstable Hangman's fracture: Anterior or posterior surgery? Journal of craniovertebral junction & spine. 2019 Oct-Dec [PubMed PMID: 32089613]
Jun XH,Yi L, Percutaneous Fixation of Levine-Edwards Type II Hangman's Fractures Under the Guidance of an Orthopedic Robot. Orthopedics. 2023 Jan-Feb [PubMed PMID: 36343643]
Sacino AN,Materi J,Davidar AD,Judy B,Liu A,Hwang B,Theodore N, Robot-assisted atlantoaxial fixation: illustrative cases. Journal of neurosurgery. Case lessons. 2022 Jun 20 [PubMed PMID: 35733845]
Level 3 (low-level) evidenceAsuzu DT,Buchholz AL, MAZOR-X robotic-navigated percutaneous C2 screw placement for hangman's fracture: a case report. Journal of spine surgery (Hong Kong). 2021 Sep [PubMed PMID: 34734148]
Level 3 (low-level) evidenceDaves GD Jr, The occurrence of natural stable analogues. Implications for the design of therapeutic agents. Acta pharmaceutica Suecica. 1987 [PubMed PMID: 3330895]
Level 3 (low-level) evidenceOswald KAC,Deml MC,Heldner MR,Seiffge D,Bigdon SF,Albers CE, Intraoperative color-coded duplex ultrasound for safe surgical reduction of displaced hangman fractures in patients with atypical course of the vertebral artery: A case report of two patients. Trauma case reports. 2022 Feb [PubMed PMID: 34917739]
Level 3 (low-level) evidenceXu D,Gan K,Wang Y,Wang Y,Ma W, Comparison of C2-3 Pedicle Screw Fixation With C2 Spinous Muscle Complex and Iliac Bone Graft for Instable Hangman Fracture. Frontiers in surgery. 2021 [PubMed PMID: 34901137]
Ashraf AM,Houten JK, A Potentially Advantageous Use of a Zero-Profile, Stand-Alone Anterior Interbody Spacer at C2-3 for the Treatment of Hangman's Fracture: A Technical Case Report. Cureus. 2021 Jun [PubMed PMID: 34354875]
Level 3 (low-level) evidenceBasankin IV,Giulzatyan АА,Nesterenko PB,Bagaudinov АB,Tayurski DА,Mukhanov МL, Experience of Using Transpedicular Osteosynthesis in Traumatic Spondylolisthesis of the Axis. Sovremennye tekhnologii v meditsine. 2021 [PubMed PMID: 35265349]
Liu Y,Zhu Y,Li X,Chen J,Yang S,Yang H,Jiang W, A new transpedicular lag screw fixation for treatment of unstable Hangman's fracture: a minimum 2-year follow-up study. Journal of orthopaedic surgery and research. 2020 Sep 1 [PubMed PMID: 32873313]
Agrawal M,Sawarkar D,Singh PK,Mishra S,Meena R,Gupta DK,Chandra PS,Kale SS, Posterior fixation for paediatric and adolescent unstable hangman's fracture: evolution to C1 sparing techniques. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2021 Jul [PubMed PMID: 33783618]
Sawarkar D,Agrawal M,Singh PK,Mishra S,Agrawal D,Kumar A,Verma S,Doddamani R,Meena R,Garg K,Gurjar H,Chandra PS,Kale SS, Evolution to Pedicle Reformation Technique in Surgical Management of Hangman's Fracture. World neurosurgery. 2021 May [PubMed PMID: 33567364]
Jin C,Xie N,Ren Y,Liu X,Tang F,Guo Q,Jia L,Cheng L, How Does Cervical Sagittal Balance Change After Hangman Fracture Treated with Anterior or Posterior Approach Surgery? World neurosurgery. 2020 Jun [PubMed PMID: 32201290]
Man Kyu C,Youngseok K,Ki Hong K,Dae-Hyun K, Direct trans-pedicular screw fixation for atypical hangman's fracture: A minimally invasive technique using the tubular retractor system. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Dec [PubMed PMID: 31431401]
Soliman MAR,Kwan BYM,Jhawar BS, Minimally Invasive Unilateral Percutaneous Transfracture Fixation of a Hangman's Fracture Using Neuronavigation and Intraoperative Fluoroscopy. World neurosurgery. 2019 Feb [PubMed PMID: 30391610]
Yuan S,Wei B,Tian Y,Yan J,Xu W,Wang L,Liu X, Posterior temporary C1-2 fixation for 3-part fractures of the axis (odontoid dens and Hangman fractures). Medicine. 2018 Nov; [PubMed PMID: 30508884]
Ryken TC, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Theodore N, Walters BC. Management of isolated fractures of the axis in adults. Neurosurgery. 2013 Mar:72 Suppl 2():132-50. doi: 10.1227/NEU.0b013e318276ee40. Epub [PubMed PMID: 23417186]
Karakoyun DO,Yılmaz A,Uzlu O,Dağlıoğlu E,Işık HS, Vertebral arteriovenous fistula due to blunt neck trauma: A case report. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2022 Jun [PubMed PMID: 35652878]
Level 3 (low-level) evidenceSarath Chander V,Govindasamy R,Rudrappa S,Gopal S, Unstable Hangman Fracture Complicated by Vertebral-Venous Fistula: Surgical Considerations and Review of Literature. World neurosurgery. 2021 Jan [PubMed PMID: 32987171]
Kaiser R,Saur K,Smolanka A,Ullas G,Beneš V, Type-III Hangman's fracture combined with serious cerebrovascular injury after near-hanging: a first case report and review of the literature. British journal of neurosurgery. 2019 Sep 28 [PubMed PMID: 31566025]
Level 3 (low-level) evidenceLáinez Ramos-Bossini AJ,Gálvez López R,Pastor Rull J, Vertebral artery dissection secondary to hangman's fracture. Medicina clinica. 2020 Mar 13 [PubMed PMID: 30954291]
Foster MA,Gridley DG,Lettieri SC,Feiz-Erfan I, Brown-Sequard syndrome associated with hangman fracture after blunt trauma: A case report. Surgical neurology international. 2022 [PubMed PMID: 35509566]
Level 3 (low-level) evidenceYang Y,Dai L,Ma L,Gao X,Liu H, Incidence of dysphagia and dysphonia after Hangman's fractures: Evidence from 93 patients. Medicine. 2018 Dec [PubMed PMID: 30544470]
Pehler S,Jones R,Staggers JR,Antonetti J,McGwin G,Theiss SM, Clinical Outcomes of Cervical Facet Fractures Treated Nonoperatively With Hard Collar or Halo Immobilization. Global spine journal. 2019 Feb; [PubMed PMID: 30775208]
Level 2 (mid-level) evidence