Introduction
The brain is the nervous system's central organ, responsible for coordinating and controlling various bodily functions. Briefly, the brain's main regions include the cerebral cortex, thalamus, hypothalamus, limbic system, midbrain, cerebellum, medulla oblongata, and pons. The cranial nerves emanate at different brain levels. The ventricles are the spaces inside the brain filled with cerebrospinal fluid (CSF).
Anterior and posterior arterial networks of the central nervous system form the circle of Willis. The venous sinuses drain the superficial veins, which follow the same course as their corresponding arteries. Deep brain structures also drain to the venous sinuses via deep veins.
The cranium or skull serves as the brain's protective enclosure. The frontal, parietal, temporal, occipital, sphenoid, and ethmoid bones comprise the cranium. The skull bones' thickness varies in different regions, with some areas being more vulnerable to penetrating injuries than others.
The meninges are the brain's protective coverings divided into the dura, arachnoid, and pia mater. The dura mater is the outermost layer, lying just beneath the skull. The arachnoid mater is the middle layer, separated from the dura by the subdural space. Arachnoid granulations are small outward projections of the arachnoid mater that allow CSF to re-enter the bloodstream. The subarachnoid space contains CSF. The pia mater is the innermost layer, adhering closely to the brain.
Penetrating head trauma (PHT) constitutes a foreign-body head injury breaching the skull and invariably involving the dura mater and brain.[1] PHT is the most lethal form of traumatic head injury. Almost 70-90% of the victims die before reaching the hospital, and 50% of those reaching the hospital eventually expire in the ED during resuscitation.[2][3][4][5] Recovery and rehabilitative strategies among survivors are often protracted and complicated.
The 2001 severe head injury management guidelines published by the Brain Trauma Foundation (BTF) and American Association of Neurological Surgeons (AANS) do not include PHT management algorithms. The current guidelines for managing PHT are based on military protocols during the Iraq and Afghanistan conflicts over 2 decades ago. However, a widely accepted evaluation protocol includes the primary survey, stabilization, secondary survey with detailed neurological examination, and pertinent imaging studies. The cornerstone of surgical management of PHT involves early decompression, safe debridement, and watertight dural closure.[6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
PHT can result from high-velocity penetrations, for example, from missiles and blast fragments. PHT may also arise from low-velocity injuries, as happens after a knife-stabbing incident.[7] The force magnitude and damage extent and direction determine the presentation of the condition.
Epidemiology
In the United States, approximately 20,000 headshot injuries occur annually. Most PHT deaths are due to firearm injuries. US military data from 2000 to 2015 estimate the incidence of this condition to be 1.47%. Almost 32,000 to 35,000 annual civilian deaths result from PHT.[8][9]
Pathophysiology
The projectile (a foreign object) penetrates the skull forcefully, damaging the meninges and brain. The complexity of the brain injury is determined by the projectile's ballistic characteristics, bullet design, muzzle velocity, travel distance, and yaw or tumbling.[6]
The projectile creates a permanent cavitation along its path. The sonic and pressure waves from the projectile's motion produce temporary cavitations. Expansion and retraction of these cavities result in distant punctate hemorrhages and hematoma progression, which may cause herniation syndrome. Released tissue thromboplastin from the injured brain parenchyma can lead to coagulopathy.
The mechanisms by which blast injuries arise are the following:
- Primary blast injury - due to the overpressure wave moving through the body
- Secondary blast injury - due to blast fragments penetrating the tissues
- Tertiary blast injury - due to the blast wind propelling the victims
- Quaternary blast injury - due to explosive forces, causing burns and crush injuries
The patterns of blast injuries include the following:
- Involvement of organs under the body armor
- Soft tissue cranio-orbital injuries
- Neurovascular injuries
Penetrating injuries may introduce contaminants or foreign materials into the brain, increasing infection risk. Secondary injury mechanisms, including ischemia, oxidative stress, excitotoxicity, and metabolic derangements, can occur in the hours to days following the initial trauma. These processes can exacerbate tissue damage and neurological deficits.
History and Physical
As in any other medical emergency, evaluating patients with PHT begins with the primary survey. Assess the patient's airway, breathing, circulation, disability, and exposure (ABCDE). Resuscitation must be started immediately for unconscious patients with no respiration or pulse, regardless of cause. Once stable, the secondary survey must be completed.
The history must be obtained as much as possible from the patient. However, individuals with PHT often present with altered sensorium, making it necessary for clinicians to elicit information from the emergency medical services (EMS) team, witnesses, or other rescuers. The history should include the following details:
- Date and time of injury
- Weapon type and caliber
- Location of the injury
- Events surrounding the injury
- The occurrence of neurologic symptoms like loss of consciousness (LOC) and seizures and their quality and duration
- Any medical comorbidity
- Whether the patient is currently on any anticoagulants or antiplatelet agents
Evaluating for signs suggesting raised intracranial pressure (ICP) is critical. The initial manifestations of PHT, such as headache, nausea, vomiting, and papilledema, may be nonspecific.
During physical examination, the superficial wound should be inspected. The entrance wound and, if present, the exit wound must be identified. Blood-matted hair may cover these wounds. When a patient presents with a gunshot wound to the head, other body parts, including the neck, chest, and abdomen, should be scrutinized for other gunshot wounds. Damage to the heart or great vessels may even be more life-threatening.
A subgaleal hematoma can become extensive because blood quickly dissects through the loose areolar tissue. This kind of hematoma can cause hemodynamic compromise. Assess whether there is any oozing of cerebrospinal fluid (CSF), blood, or brain parenchyma from the injury site. Evaluate for hemotympanum, which may indicate a basilar skull fracture. Examine all orifices for retention of foreign bodies, the weapon, teeth, and bone fragments.
A detailed neurological assessment should be performed, starting with the Glasgow Coma Scale (GCS) score. Motor, sensory, and cranial nerve function and deep tendon reflexes may be examined in patients with altered sensorium. A mental status examination (MSE) and coordination testing may be added in cooperative patients. Assume multiple injuries in cases of PHT. The neck, chest, abdomen, pelvis, and extremities must also be carefully examined.
PHT's presentation depends on the trauma mechanism, lesion sites, and associated injuries. Lateralizing signs can help clinicians localize the brain injury and determine its extent at baseline. Note that the neurologic damage may be distant from the impact site.
Evaluation
The initial laboratory exams for patients who suffered traumatic injuries must include a complete blood count, blood typing, coagulation studies, and a basic metabolic panel. If an emergency surgery is likely, information from these blood tests will guide the surgical team in evaluating the patient's health before performing the procedure. Abnormalities must be addressed before or during surgery.
Imaging studies must include plain radiographs, computed tomography (CT), and magnetic resonance imaging (MRI). The roles of these tests are explained below.[6]
Plain Radiographs
Plain radiographs aid in determining the shape of the penetrating objects and the presence of intracranial missile or bone fragments and concurrent pneumocephalus. However, the missile trajectory may not be easily determined owing to ricocheting or fragmentations. Plain x-rays are also appropriate for documenting injuries in other body parts in polytrauma cases.
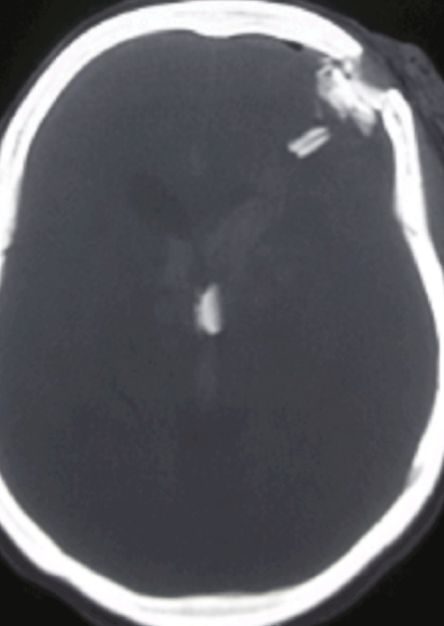
CT Scan
CT is the neuroradiologic modality of choice (see Image. Computed Tomography Of Non-Missile Penetrating Head Injury). CT scans may show in-driven bone or missile fragments, providing essential clues on missile trajectory, intracranial injury patterns, and associated herniation effects. However, the CT scan may miss radiolucent objects like wood fragments.
Certain factors are essential in critical decision-making and have prognostic implications. These may include the following:
- Sites of entry and exit wounds
- Presence of intracranial fragments
- Missile track and its relationship to both blood vessels and air-containing skull-base structures
- Presence of intracranial air
- Patterns of intracranial injuries
- Presence of cerebral herniation
Both acute and chronic lesions may appear on a CT scan, as in patients who had a stroke before the penetrating injury. Differentiating acute from chronic lesions helps determine baseline neurologic function in individuals with prior brain injuries.
MRI
MRI helps to localize wooden objects if present. This modality also provides valuable information on associated soft tissue injuries. However, an MRI should not be performed if intracranial metallic fragments could be present.
Treatment / Management
The patient must be stabilized without removing the penetrating object in the prehospital setting or a nontrauma facility. Early evaluation of high-risk mechanisms at a level 1 trauma center may improve outcomes.[10][11] Patients with PHT require meticulous medical and surgical management. In the emergency department (ED), resuscitation and stabilization should be provided, managing the ABCDEs using Advanced Trauma Life Support (ATLS) guidelines. Early activation of a trauma team may help promptly recognize polytrauma. The systolic blood pressure must be maintained above 90 mm Hg.[12][13][14](A1)
The prime dictum in the new military model of management of PHT includes the following:
- Saving the patient's life - by performing ATLS, Advanced Cardiac Life Support (ACLS), and the "far-forward" approach in resuscitation and decompression
- Preventing infection - by ensuring a watertight dural closure
- Preserving function - by aggressively sorting and mitigating secondary insults, such as meningitis, seizures, and stroke
- Restoring anatomic function - by cranioplasty
Details of the strategies in each stage of care are provided below.
Prehospital Care
The goals of this stage are initial resuscitation, secondary injury prevention or mitigation, on-scene wound management, and cervical spine immobilization. Avoiding intracranial hypertension (ICP ≥ 20 mm Hg), brain tissue hypoxemia (PbtO2 < 15 mm Hg), or hyperemia (PbtO2 > 35 mm Hg) is critical to minimizing neuronal damage. The combat experiences in Iraq and Afghanistan have shown the significance of early hypotension, hypoxia, hypocarbia, and hypercarbia management.
Rapid transport to a definitive care unit is crucial in the prehospital setting. The far-forward approach incorporates rapid evacuation from the “kill box” to a safer area. Critical care air transport transfers the patient to a combat support hospital (CSH) while responders provide prompt medical evaluation and resuscitation.[15]
ED Care
The priority ED care goals are aggressive resuscitation, stabilization, clinical assessments, and radiological workup. Many patients with PHT will likely require operative intervention. Clinicians must have a low threshold for obtaining surgical consultation.
Penetrating objects must not be removed from the skull until trauma and neurosurgical evaluation are obtained. Instead, the protruding object should be stabilized and protected from motion during patient transportation to prevent further injury. Sterile dressings must be applied to both the entrance and exit wounds.
Surgical Management
Effective hemostasis and infection control strategies were not available until 1889. Acute decompression and hemorrhage control were the initial goals of surgical intervention. A radical debridement strategy removing all foreign bodies evolved from the principles of Dr. Harvey Cushing and was utilized earlier during World Wars I and II and the Korean, Vietnam, and Iran–Iraq Wars. The concept was to limit secondary injury and promote eventual reconstruction.
During World War II, Dr. Donald Matson outlined the tenets of far-forward neurosurgery: immediate life-saving decompression, neural function preservation, anatomic restoration, and infection prevention. Rapid evacuation of casualties, blood availability in the forward area, and antibiotic use have dramatically improved PHT outcomes since then.
A shift to conservative debridement started during the 1980s Israeli-Lebanon conflict. Early radical decompression by hemicraniectomy with conservative debridement and duraplasty was advocated starting the time of Operation Iraqi Freedom (OIF). However, a new PHT management strategy has recently evolved whereby rapid, far-forward cranial decompression with watertight dural closure is performed before rapid evacuation to a major trauma center.
Surgical treatment should ideally be performed within 12 hours of injury to prevent infection and other complications. Nonviable scalp, bone fragments, and necrosed brain tissue are extensively debrided. Hematomas causing mass effects are promptly evacuated. Only the superficial bone and missile fragments and easily accessed non-eloquent brain regions are removed. Indications for removing intraventricular foreign bodies are migration, occlusive hydrocephalus, porous material (rock, wood) contact with the ventricles, and infection.[16]
Water-tight dural closure is the dictum. However, deeply embedded fragments are not pursued unless delayed movement or vascular compromise has been documented. This strategy minimizes damage from missile tract exploration.
Homeostasis around the venous sinuses can be achieved using techniques such as muscle and dural elevation, sinus ligation, and oversewing, which preserve the sinuses when possible. Additional hemostatic agents Surgicel, Gelfoam, and cottonoid patties may be used. The sinuses must be exposed, secured, and repaired while avoiding inadvertent air emboli.
Bilateral exposures such as coronal incisions provide adequate exposure and vascular control. Such techniques also facilitate wound closure by partial-thickness scalp-releasing incisions. Proximal control of the cervical carotid is critical while exploring the lateral skull base.
Temporary or permanent CSF diversion helps to decompress the hemicraniectomy flap and seal the associated CSF leaks. Scalp flap vascularity must be preserved. "Knockout removal" by making mallet strikes parallel to the weapon tract is recommended.[17]
The modern military paradigm focuses on early cranial decompression, CSF leak prevention, and aggressive secondary insult mitigation. The BTF, military and civilian TBI experts, and the American Department of Defense (DoD) are collaborating to generate updated, evidence- and consensus-based PHT clinical practice guidelines and new care algorithms.
Multidisciplinary Postoperative Management
The patient must be transferred to a neurointensive care unit and closely monitored by interprofessional team members (see Enhancing Healthcare Team Outcomes below). The ICP must be maintained below 20 to 25mmHg and cerebral perfusion pressure (CPP) above 60 mm Hg. Nutrition and medical management must focus on deep vein thrombosis (DVT), seizure, and stroke prevention.
Differential Diagnosis
The differentials of PHT include the following:
- Alzheimer disease
- Stroke
- Cancer metastasis to the brain
- Cerebral aneurysm
- Frontal lobe syndrome
- Epilepsy
- Hydrocephalus
- Prion-related diseases
However, physical examination and imaging tests will differentiate PHT from these conditions. Meanwhile, PHT has a highly variable presentation due to the differences in the intracranial projectile movements, which include the following:
- Penetrating injuries wherein the projectile penetrates the skull and dura but remains within the skull, characteristically lacking an exit wound
- Perforating injuries with a ‘‘through and through’’ mechanism, characterized by having both entry and exit wounds
- Tangential injuries wherein the missiles or fragments glance off the skull but may drive skull fragments inside the brain
- Ricochet that creates multiple intracranial trajectories
- Careening when the projectile penetrates the skull but moves along the cortical periphery without penetrating the brain parenchyma
A detailed evaluation will help differentiate between these patterns.
Prognosis
The clinical outcomes of PHT are mostly abysmal. Low post-resuscitation GCS, older age, hypoxia, hypotension, and the use of ballistic weapons confer a bad prognosis. Lateral perforating wounds have the worst prognosis. Penetrating wounds involving the zona fatalis—a suprasellar area comprising the third ventricle, hypothalamus, and thalamus—and showing a "tram-track" sign on imaging have almost 100% mortality.
Self-inflicted fatal PHT is observed in 35% of cohorts.[18] Additionally, a systematic review and meta-analysis with a pooled sample size of 1738 patients revealed that 34.2% of cohorts with PHT had a poor outcome, and the overall mortality for these patients was 18%. A GCS score greater than 8 at presentation is a significant predictor of decreased mortality.[19]
However, far-forward strategies in the military setting are associated with a four-fold increase in patients living independently at 2 years compared to their civilian counterparts with PHT. ICP monitoring also improves survival.[20][21]
Complications
The complications after surviving PHT can be categorized as follows:
Early
- Hypoxia
- Hypotension
- Hematoma
- Ischemia
- Raised ICP
- Anatomic defects
- Neurogenic pulmonary edema
- Stunned myocardium syndrome
- Dyselectrolytemia from diabetes insipidus, cerebral salt-wasting syndrome, syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Neuroendocrine dysfunction
- Traumatic optic neuropathy
- Cranial nerve injuries.
Intermediate
- Refractory cerebral edema
- Acute hydrocephalus
- Seizures
- Vasospasm
- CSF leak
- Pseudoaneurysm (traumatic intracranial aneurysm)
- Deep venous thrombosis
Late
- Infection
- Late hydrocephalus
- CSF fistula
- Venous sinus occlusions
- Arteriovenous fistulas
- Trephination syndrome (shrunken skin flap syndrome)
- Temporalis atrophy
- Hygroma
- Scalp necrosis
- Complications relating to cranioplasty
- Lead or copper toxicity from retained bullet fragments.
Grossly contaminated wounds, CSF leaks, perforating wounds, penetrating wounds with air sinus violation, transventricular injury patterns, or those crossing the midline have an increased infection risk. The incidence of infection was 58.8% in the pre-antibiotic era. Presently, the incidence of infection in patients with PHT is 4 to 11% in the military compared to 1 to 5% among civilians. The infection risk is also higher for patients with lower GCS scores and higher Organ Failure Assessment scores.[22]
Cephalosporin administration for at least 7 to 14 days is usually recommended for antibiotic prophylaxis. Staphylococcus epidermidis, Staphylococcus aureus, gram-negative bacilli, and anaerobes are the most common causes of secondary infection in patients with PHT. Metronidazole can be added to cephalosporins to broaden the antibacterial coverage.[23] Synthetic grafts should be avoided in contaminated wounds. CSF leaks occurring remotely from the point of entry or exit wounds may require CSF diversion.
Vascular complications in PHT range from 5 to 40%. Orbitofacial or pterional region involvement, extensive dural penetration, intracranial hematomas, and the occurrence of subarachnoid hemorrhage are associated with a higher vascular complication risk in patients with PHT. Blast exposures also elevate the risk of neurovascular injuries and vasospasms.
The incidence of posttraumatic epilepsy ranges from 30 to 50%, with 10% occurring in the first week and 80% occurring within the first 2 years of injury. The prophylactic antiepileptic use beyond the first 7 days of injury is not recommended.[24]
The most common complications associated with non-missile penetrating head trauma (NMPHT) include vascular damage (19%) and infection (14%). Stab injuries with transorbital penetration, hematoma larger than the tract, and a depth exceeding 40 mm have a high risk of developing vascular injuries. Stab-to-referral time greater than 24 hours, the lack of prophylactic antibiotics, and the presence of a weapon in situ increase the risk of infection. One study revealed that the overall mortality of NMPHT was 10%, with vascular injuries accounting for 42% of them. Low GCS on admission, concurrent vascular injuries, and eloquent brain involvement had poor outcomes. A weapon in situ had a favorable outcome.
In another study, the pooled central nervous system infection rate was 13.8%, the seizure rate was 13.2%, and the cerebrospinal fluid leak or fistula rate was 5.4%. The overall mortality reported was 18.0%. Higher clinical and imaging severity scores correlated with neurological impairment and mortality risk.[25]
Deterrence and Patient Education
The key preventive measures for PHT include the following:
- Use of protective headgear
- Firearm safety
- Following workplace safety regulations
- Fall prevention
- Vehicle safety
- Violence prevention
- Improving infrastructure
- Fall risk assessment
- Regular health check-ups in patients with high fall or accident risk
These measures will not prevent all PHT incidents but will minimize the risk of the condition's occurrence. Preventing PHT involves a multifaceted approach that includes education, implementing public policies, instituting engineering solutions, and promoting safe behaviors in various settings.
Pearls and Other Issues
The most important points in PHT management include the following:
- Immediate assessment and stabilization of vital signs are crucial. The ABCDEs should be quickly evaluated and managed, as the condition can be life-threatening.
- Patients with penetrating head injuries benefit from immediate transfer to a trauma center equipped with specialized resources, neurosurgical expertise, and comprehensive trauma care capabilities.
- Rapid neuroimaging, particularly CT scanning, is essential for evaluating the extent and location of injuries, identifying foreign bodies, assessing bleeding, and guiding immediate management.
- Cervical immobilization must be performed if a cervical spine injury cannot be ruled out.
- Prophylactic antibiotics reduce the risk of infection, especially in soil or organic material contamination cases.
- Neurosurgical consultation and intervention are often necessary in cases where there are indications for removing foreign bodies, repairing blood vessels, controlling bleeding, or relieving intracranial pressure.
- Patients with severe penetrating head trauma may require ICU admission for close monitoring of vital parameters like neurological status and ICP.
- Continuous neurological assessments are important in detecting changes in the patient's condition, monitoring for signs of increased ICP, and evaluating neurological deficits.
- Measures to prevent secondary brain injury, such as maintaining adequate oxygenation, controlling intracranial pressure, and avoiding hypotension, are critical to minimize further damage.
- Rehabilitation is often necessary for individuals with penetrating head trauma to optimize recovery and regain functional abilities.
- Long-term follow-up and monitoring are essential to managing potential complications, addressing cognitive or physical impairments, and supporting the patient's recovery over time.
Rapid assessment and multidisciplinary management help optimize patient outcomes.
Enhancing Healthcare Team Outcomes
Individuals with PHT require a collaborative care approach among various healthcare professionals. The goal is to optimize outcomes and support the patient's recovery throughout the different stages of treatment. The multidisciplinary team members involved in PHT management are the following:[26][27]
- EMS personnel - EMS professionals play a critical role in the initial assessment, stabilization, and rapid transportation of patients with PHT to specialized trauma facilities.
- Emergency medicine physicians and trauma surgeons - These healthcare professionals often provide the first line of care for individuals with PHT. These specialists provide immediate evaluation, resuscitation, and decision-making regarding the need for emergency surgical intervention.
- Neurosurgeons - Neurosurgeons perform procedures such as removing foreign objects, repairing damaged blood vessels, managing hemorrhages, and relieving ICP elevation to minimize neurologic damage after PHT.
- Neurologists - Neurologists assess and manage the neurological status of patients, provide expertise in diagnosing and treating neurologic conditions, and contribute to the long-term neurological care and rehabilitation of individuals with brain injuries.
- Intensivists or neurointensivists - These specialists focus on monitoring and stabilizing patients with severe head trauma, ensuring optimal ventilation, hemodynamic stability, and management of intracranial pressure.
- Neuroradiologists - These medical professionals interpret imaging studies to assist in diagnosing the nature, extent, and location of brain injuries. Neuroradiologists provide crucial information for surgical planning and postoperative monitoring.
- Physical and occupational therapists - Rehabilitation specialists help patients regain motor skills, cognitive abilities, and functional independence. These providers develop tailored rehabilitation programs to optimize recovery and improve quality of life for patients recovering from PHT.
- Speech-language pathologists - These professionals assist patients in regaining speech and swallowing function that may have been affected by the head trauma.
- Psychologists and psychiatrists - Mental health professionals provide support to patients and their families, addressing emotional, cognitive, and behavioral challenges that may arise after head trauma. These providers offer counseling, cognitive therapy, and emotional support.
- Social workers and case managers - These professionals assist patients and families in navigating the healthcare system, accessing resources, coordinating care, and addressing social, financial, and practical needs during the recovery process.
Effective coordination among these multidisciplinary team members minimizes complications and improves outcomes for patients with PHT.
Media
(Click Image to Enlarge)
References
Fahde Y, Laghmari M, Skoumi M. Penetrating head trauma: 03 rare cases and literature review. The Pan African medical journal. 2017:28():305. doi: 10.11604/pamj.2017.28.305.10376. Epub 2017 Dec 11 [PubMed PMID: 29721135]
Level 3 (low-level) evidencevan Rein EAJ, van der Sluijs R, Voskens FJ, Lansink KWW, Houwert RM, Lichtveld RA, de Jongh MA, Dijkgraaf MGW, Champion HR, Beeres FJP, Leenen LPH, van Heijl M. Development and Validation of a Prediction Model for Prehospital Triage of Trauma Patients. JAMA surgery. 2019 May 1:154(5):421-429. doi: 10.1001/jamasurg.2018.4752. Epub [PubMed PMID: 30725101]
Level 1 (high-level) evidenceKommaraju K, Haynes JH, Ritter AM. Evaluating the Role of a Neurosurgery Consultation in Management of Pediatric Isolated Linear Skull Fractures. Pediatric neurosurgery. 2019:54(1):21-27. doi: 10.1159/000495792. Epub 2019 Jan 23 [PubMed PMID: 30673671]
Vlček M, Jaganjac E, Niedoba M, Landor I, Neumann J. Current treatment procedures for civilian gunshot wounds. Rozhledy v chirurgii : mesicnik Ceskoslovenske chirurgicke spolecnosti. 2018 Winter:97(12):558-562 [PubMed PMID: 30646735]
Cengiz O, Atalar AÇ, Tekin B, Bebek N, Baykan B, Gürses C. Impact of seizure-related injuries on quality of life. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2019 Mar:40(3):577-583. doi: 10.1007/s10072-018-3697-3. Epub 2019 Jan 5 [PubMed PMID: 30612277]
Level 2 (mid-level) evidenceKazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. Journal of emergencies, trauma, and shock. 2011 Jul:4(3):395-402. doi: 10.4103/0974-2700.83871. Epub [PubMed PMID: 21887033]
Hawryluk GWJ, Selph S, Lumba-Brown A, Totten AM, Ghajar J, Aarabi B, Ecklund J, Shackelford S, Adams B, Adelson D, Armonda RA, Benjamin J, Boone D, Brody D, Dengler B, Figaji A, Grant G, Harris O, Hoffer A, Kitigawa R, Latham K, Neal C, Okonkwo DO, Pannell D, Rosenfeld JV, Rosenthal G, Rubiano A, Stein DM, Stippler M, Talbot M, Valadka A, Wright DW, Davis S, Bell R. Rationale and Methods for Updated Guidelines for the Management of Penetrating Traumatic Brain Injury. Neurotrauma reports. 2022:3(1):240-247. doi: 10.1089/neur.2022.0008. Epub 2022 Jun 21 [PubMed PMID: 35919507]
Fathalla H, Ashry A, El-Fiki A. Managing military penetrating brain injuries in the war zone: lessons learned. Neurosurgical focus. 2018 Dec 1:45(6):E6. doi: 10.3171/2018.8.FOCUS18371. Epub [PubMed PMID: 30544315]
Romero Pareja R, Castro Delgado R, Turégano Fuentes F, Jhon Thissard-Vasallo I, Sanz Rosa D, Arcos González P. Prehospital triage for mass casualty incidents using the META method for early surgical assessment: retrospective validation of a hospital trauma registry. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2020 Apr:46(2):425-433. doi: 10.1007/s00068-018-1040-6. Epub 2018 Nov 7 [PubMed PMID: 30406394]
Level 2 (mid-level) evidencePuffenbarger MS, Ahmad FA, Argent M, Gu H, Samson C, Quayle KS, Saito JM. Reduction of Computed Tomography Use for Pediatric Closed Head Injury Evaluation at a Nonpediatric Community Emergency Department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2019 Jul:26(7):784-795. doi: 10.1111/acem.13666. Epub 2019 Feb 1 [PubMed PMID: 30428150]
Voss JO, Thieme N, Doll C, Hartwig S, Adolphs N, Heiland M, Raguse JD. Penetrating Foreign Bodies in Head and Neck Trauma: A Surgical Challenge. Craniomaxillofacial trauma & reconstruction. 2018 Sep:11(3):172-182. doi: 10.1055/s-0038-1642035. Epub 2018 Apr 24 [PubMed PMID: 30087746]
Maragkos GA, Papavassiliou E, Stippler M, Filippidis AS. Civilian Gunshot Wounds to the Head: Prognostic Factors Affecting Mortality: Meta-Analysis of 1774 Patients. Journal of neurotrauma. 2018 Nov 15:35(22):2605-2614. doi: 10.1089/neu.2018.5682. Epub 2018 Jul 23 [PubMed PMID: 29877141]
Level 1 (high-level) evidenceMcGrew PR, Chestovich PJ, Fisher JD, Kuhls DA, Fraser DR, Patel PP, Katona CW, Saquib S, Fildes JJ. Implementation of a CT scan practice guideline for pediatric trauma patients reduces unnecessary scans without impacting outcomes. The journal of trauma and acute care surgery. 2018 Sep:85(3):451-458. doi: 10.1097/TA.0000000000001974. Epub [PubMed PMID: 29787555]
Level 1 (high-level) evidenceMilton J, Rugino A, Narayan K, Karas C, Awuor V. A Case-Based Review of the Management of Penetrating Brain Trauma. Cureus. 2017 Jun 12:9(6):e1342. doi: 10.7759/cureus.1342. Epub 2017 Jun 12 [PubMed PMID: 28706766]
Level 3 (low-level) evidenceLang SS, Kumar N, Zhao C, Rahman R, Flanders TM, Heuer GG, Huh JW. Intracranial Pressure and Brain Tissue Oxygen Multimodality Neuromonitoring in Gunshot Wounds to the Head in Children. World neurosurgery. 2023 Oct:178():101-113. doi: 10.1016/j.wneu.2023.07.059. Epub 2023 Jul 20 [PubMed PMID: 37479026]
Stanishevsky AV, Aliev ZS, Gizatullin SK, Rafaelyan AA, Svistov DV, Gavrilov GV, Onnitsev IE. Metallic foreign bodies of brain ventricles. Zhurnal voprosy neirokhirurgii imeni N. N. Burdenko. 2022:86(6):25-35. doi: 10.17116/neiro20228606125. Epub [PubMed PMID: 36534621]
Harrington BM, Gretschel A, Lombard C, Lonser RR, Vlok AJ. Complications, outcomes, and management strategies of non-missile penetrating head injuries. Journal of neurosurgery. 2020 Jun 19:134(5):1658-1666. doi: 10.3171/2020.4.JNS20122. Epub 2020 Jun 19 [PubMed PMID: 32559744]
Hakkenbrak NAG, Bakkum ER, Zuidema WP, Halm JA, Dorn T, Reijnders UJL, Giannakopoulos GF. Characteristics of fatal penetrating injury; data from a retrospective cohort study in three urban regions in the Netherlands. Injury. 2023 Jan:54(1):256-260. doi: 10.1016/j.injury.2022.08.025. Epub 2022 Aug 19 [PubMed PMID: 36068101]
Level 2 (mid-level) evidenceKarras CL, Texakalidis P, Nie JZ, Tran HM, Dahdaleh NS, Bovis GK, Cybulski GR, Magill ST. Outcomes Following Penetrating Brain Injuries in Military Settings: A Systematic Review and Meta-Analysis. World neurosurgery. 2022 Oct:166():39-48. doi: 10.1016/j.wneu.2022.07.062. Epub 2022 Jul 21 [PubMed PMID: 35870782]
Level 1 (high-level) evidencePan J, Bonow RH. Intracranial Pressure Monitors in Patients With Penetrating Brain Injury. JAMA network open. 2023 Mar 1:6(3):e236754. doi: 10.1001/jamanetworkopen.2023.6754. Epub 2023 Mar 1 [PubMed PMID: 36961469]
Mansour A, Rowell S, Powla PP, Horowitz P, Goldenberg FD, Lazaridis C. Comparative Effectiveness of Intracranial Pressure Monitoring vs No Monitoring in Severe Penetrating Brain Injury Management. JAMA network open. 2023 Mar 1:6(3):e231077. doi: 10.1001/jamanetworkopen.2023.1077. Epub 2023 Mar 1 [PubMed PMID: 36961466]
Level 2 (mid-level) evidenceMeister MR, Boulter JH, Yabes JM, Sercy E, Shaikh F, Yokoi H, Stewart L, Scanlon MM, Shields MM, Kim A, Tribble DR, Bartanusz V, Dengler BA. Epidemiology of cranial infections in battlefield-related penetrating and open cranial injuries. The journal of trauma and acute care surgery. 2023 Aug 1:95(2S Suppl 1):S72-S78. doi: 10.1097/TA.0000000000004018. Epub 2023 May 29 [PubMed PMID: 37246289]
Bayston R, de Louvois J, Brown EM, Johnston RA, Lees P, Pople IK. Use of antibiotics in penetrating craniocerebral injuries. "Infection in Neurosurgery" Working Party of British Society for Antimicrobial Chemotherapy. Lancet (London, England). 2000 May 20:355(9217):1813-7 [PubMed PMID: 10832851]
Level 1 (high-level) evidence. Antiseizure prophylaxis for penetrating brain injury. The Journal of trauma. 2001 Aug:51(2 Suppl):S41-3 [PubMed PMID: 11505199]
Hanafi I, Munder E, Ahmad S, Arabhamo I, Alziab S, Badin N, Omarain A, Jawish MK, Saleh M, Nickl V, Wipplinger T, Wipplinger C, Nickl R. War-related traumatic brain injuries during the Syrian armed conflict in Damascus 2014-2017: a cohort study and a literature review. BMC emergency medicine. 2023 Mar 29:23(1):35. doi: 10.1186/s12873-023-00799-6. Epub 2023 Mar 29 [PubMed PMID: 36977988]
Chatfield-Ball C, Boyle P, Autier P, van Wees SH, Sullivan R. Lessons learned from the casualties of war: battlefield medicine and its implication for global trauma care. Journal of the Royal Society of Medicine. 2015 Mar:108(3):93-100. doi: 10.1177/0141076815570923. Epub [PubMed PMID: 25792616]
Cristofori I, Pal S, Zhong W, Gordon B, Krueger F, Grafman J. The lonely brain: evidence from studying patients with penetrating brain injury. Social neuroscience. 2019 Dec:14(6):663-675. doi: 10.1080/17470919.2018.1553798. Epub 2018 Dec 12 [PubMed PMID: 30501456]