Introduction
Elbow fractures are more common in the pediatric population than in the adult population. Children often utilize an outstretched arm as a protective mechanism when falling, creating a high incidence of fractures about the elbow. Supracondylar fractures of the humerus account for up to 18% of pediatric fractures and 60% of elbow fractures.[1] In 1959 Dr. Gartland described that even expert trauma surgeons are anxious and apprehensive while managing supracondylar humerus fractures. Despite evolutions in the evaluation and treatment over the years, these fractures still pose considerable challenges to orthopedic surgeons.
The modified Gartland classification is often used to describe fracture patterns and guide treatment.[2] These injuries can be significant due to the risks of neurological damage, vascular injury, and compartment syndrome.[3] Inadequate reduction and fixation can also lead to malunion and deformity.[4] On the other hand, some patients who develop a malunion may have a satisfactory function in the long term.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The distal humerus is composed of medial and lateral columns. The medial and lateral columns are composed of the trochlea and medial epicondyle medially and the capitellum and lateral epicondyle laterally. The distal humerus narrows proximally from metaphysis to diaphysis. The humerus also thins in its anteroposterior width as the medial and lateral columns merge at the proximal aspect of the olecranon fossa. This creates a point of relative weakness in the supracondylar region of the distal humerus.[6]
Epidemiology
The supracondylar region of the distal humerus is the most commonly fractured area around the elbow in children.[7] They most frequently occur in children aged 5 to 7 years. The median age is approximately six years, and the incidence gradually decreases with age.[8] Some studies describe an increased prevalence among males than females, while others describe a higher prevalence in females.[8][9][10] However, a recent epidemiological study found no significant difference between the genders.[11] Extension-type fractures are much more common than flexion-type fractures and occur as a result of a fall on an outstretched hand.[12]
Ligamentous laxity in the pediatric age group causes hyper-extension of the elbow and contributes to causing extension-type fractures.[11][13] Also, it has been reported that these fractures are more common on weekends and during summer.[8][11] Flexion-type fractures are more prevalent in older children. These injuries often occur in the non-dominant upper extremity.[14] The incidence of open supracondylar fractures is around 1%.[11]
Pathophysiology
The shape of the distal humerus is roughly triangular in the coronal plane, with the base composed of the lateral epicondyle, capitellum, trochlea, and medial epicondyle. In the axial plane, it is dumbbell shaped owing to the thin plate of the bone in the middle, at the site of the olecranon fossa and coronoid fossa. Most fractures occur when the child falls on an outstretched arm causing hyperextension of the elbow. The olecranon process engages the olecranon fossa producing an extensive force on the distal humerus.[15][16] The bone fractures at the weakest point, and the anterior humeral cortex fails in tension. The posterior cortex and periosteum may be intact. This is the mechanism of injury for extension-type fractures, which account for up to 95% of supracondylar fractures. Flexion-type fractures occur with a fall on a flexed elbow but are much less common.[12]
The mechanism of injury and the resultant displacement of the fracture also guides the reduction maneuver performed. In posteromedial displacement of the distal fragment, the medial periosteum is intact. Due to this, the reduction is performed in pronation which tensions the medial periosteum and prevents varus malalignment. On the other hand, posterolateral displacement tends to rupture the medial periosteum, and the reduction is therefore performed in supination.[17]
History and Physical
History
There may be a history of a fall on an outstretched arm, causing an extension-type fracture or a fall on a flexed elbow. Although rare, a non-accidental injury must be excluded, accounting for <0.5% of the fractures.[18] The child or carer may give a history of pain, swelling, or deformity of the affected limb. Young children may be reluctant to use the affected limb.
Physical Examination
The affected limb must be thoroughly assessed for the integrity of the soft tissue envelope and the distal neurovascular status. Any other injuries must also be carefully evaluated and documented.
The arm may be swollen, bruised, and deformed. Any bleeding around the elbow may point towards an open fracture and needs to be assessed. The typical deformity for an "off-ended" Gartland III injury is an S-shaped deformity. There may be a "pucker sign" in the antecubital fossa, indicating that the proximal fragment may have button-holed through the brachialis muscle indenting the deep dermis.[19] This sign indicates a high-energy injury and should alert the attending clinician to the risk of the brachial artery or median nerve injury. These structures can get entrapped between the fracture fragments while performing reduction, and the surgeon should be careful.[16] These patients are also at risk of developing compartment syndrome.
Careful assessment and documentation of the functions of the median, anterior interosseous, ulnar, and radial nerves are mandatory. Best practice includes documentation of the motor and sensory functions of each nerve. Neurovascular injuries have been reported to be as high as 49%. The vascular compromise has been reported in 10-20% of the displaced supracondylar humerus fractures. Similarly, traumatic neurapraxia has been documented in around 11% of fractures, with the anterior interosseous nerve most commonly involved in extension-type fractures and the ulnar nerve most frequently involved in flexion-type injuries.[16][20]
Brachial artery injury can occur in up to 38% of displaced Gartland III fractures cases.[21] Examining the perfusion of the limb distal to the fracture is essential. Radial and ulnar pulses should be assessed. Note the temperature and color of the ipsilateral hand and measure the capillary refill time. The distinction must be made between the 'pulseless pink, perfused hand' and the 'pulseless, pale, cold hand.' There is good collateral circulation from the elbow in some children, and this accounts for the pulseless but perfused hand. Both cases require urgent management; however, the latter shows evidence of an ischaemic limb, which is a surgical emergency. The presence of neurological deficit and a pulseless hand is predictive of vascular compromise with entrapment of both artery and nerve within the fracture site.[22]
Similarly, adequate neurological evaluation is of paramount importance and should be repeated after every intervention. It is difficult to perform a thorough nerve examination in children; however, certain games like rock, paper, scissors, and ok can help in the motor assessment. The child is asked to make a fist (rock) that evaluates the median nerve, extend the fingers (paper) to assess the radial nerve, and abduct the fingers (scissors) that check the ulnar nerve motor function. Finally, asking them to make an ok sign evaluates the anterior interosseous nerve.[16]
Evaluation
Radiographic Evaluation
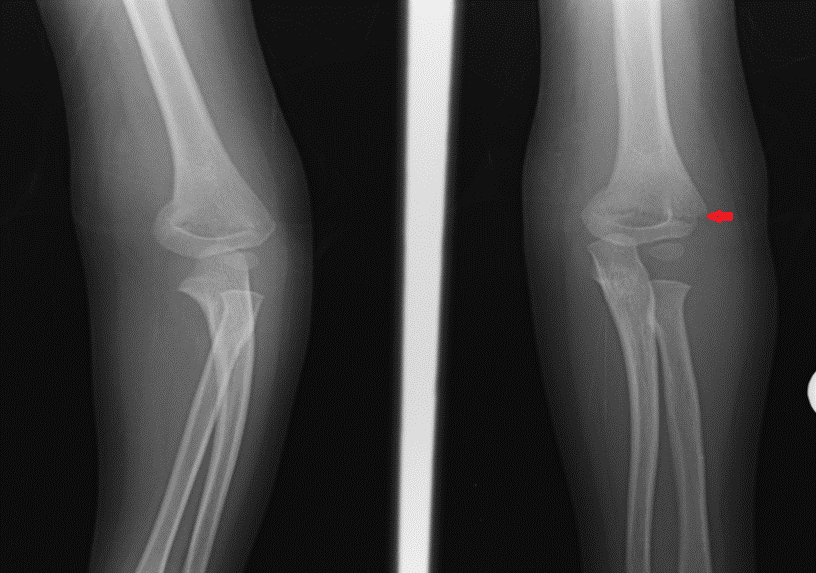
Plain radiographs of the elbow are required to make the diagnosis. Anteroposterior and lateral views are needed to confirm the type of fracture (extension vs. flexion-type), degree of displacement, malrotation, and comminution. The elbow is mostly cartilaginous in children. The first epiphyseal center to appear is that of the capitellum at one year of age.[23] Adequate knowledge of the ossification of the distal humerus with the age of appearance and fusion of the various epiphyseal centers, including the proximal radius and ulna, is needed to interpret elbow radiographs in children accurately.
Anteroposterior (AP) Radiographs
A transverse or short oblique fracture line may be seen in the supracondylar region of the distal humerus. These can be difficult to identify and may even be missed in nondisplaced fractures.
Baumann's Angle: This is also known as the humerocapitellar angle in the coronal plane. It is the angle between a line along the longitudinal axis of the humerus and a tangential line across the capitellar physis. Normal is 64-81 degrees from the longitudinal axis line. Increased Baumann's angle is suggestive of cubitus varus deformity.[24][25] Baumann's angle is a reliable measurement guide for coronal plane alignment.[26]
Radiocapitellar Line: A line drawn along the long axis of the radius should intersect the capitellum in all views. This is usually intact in supracondylar fractures unless there is an associated radial head/neck fracture.
Lateral Radiographs
Posterior Fat Pad Sign: In a flexed elbow, the posterior fat pad lies adjacent to the olecranon fossa. An intra-articular fracture from any bone within the elbow causes bleeding from the fracture site. The resultant hematoma/effusion causes the fat pad to lift away from the olecranon fossa. This creates a positive posterior fat pad sign. Several studies have reported on the utility of identifying the presence of a posterior fat pad sign in the identification of occult/nondisplaced intra-articular fractures of the elbow.[27]
Anterior Humeral Line: A longitudinal line drawn along the anterior humeral cortex on the lateral view must bisect the middle third of the capitellum. The line may intersect the anterior one-third of the capitellum in those younger than four years of age.[28] If the line is anterior to the capitellum, it indicates an extension-type fracture pattern.[29]
Angiography
Angiography is not recommended before the reduction in cases of vascular compromise.[30][31] The Pediatric Orthopedic Society of North America (POSNA) does not recommend arteriography before reduction as it delays treatment.
Gartland Classification of Supracondylar Fracture of Humerus
Supracondylar fractures in children have been classified according to Gartland.[32] Fractures are either extension or flexion-type injuries depending on the mechanism of injury and the direction of displacement of the distal fragment. Extension-type fractures are the most common, and the distal fragment is extended compared to the proximal fragment. Extension injuries were classified initially as nondisplaced, moderately displaced, and severely displaced.[32] Gartland's classification was modified by Wilkins and included a subdivision of type II injuries to include the presence or absence of a rotational deformity.[33] Leitch added the IV type of fracture to signify multiplanar instability with a completely torn periosteum. This subtype of the fracture is identified intra-operatively when complete instability of the fracture is present.[34]
The modified Gartland classification is as follows:
- Type I – Nondisplaced or minimally displaced (<2 mm) fractures
- Type IIA – Displaced fractures (>2 mm) with intact posterior hinge
- Type IIB – Displaced fracture with intact posterior hinge and malrotation
- Type III – Completely displaced fractures with disruption of the posterior periosteum
- Type IV - Completely displaced fractures with multidirectional instability[34]
Treatment / Management
All patients should be assessed according to Advanced Trauma Life Support (ATLS) principles. A non-accidental injury should be excluded from all pediatric injuries.
Non-Operative Management
Non-operative management is acceptable for nondisplaced Gartland I and minimally displaced Gartland IIA fractures. Management of Gartland II fractures has been controversial. Gartland II injuries can be managed non-operatively, provided that fracture alignment is satisfactory. Displacement and malunion can occur in the presence of medial column comminution. There is a risk of medial column collapse, leading to a cubitus varus deformity.[35] A recurvatum deformity secondary to malunion can occur if the anterior humeral line does not intersect the capitellum on lateral radiographs. These three factors: medial comminution, posterior displacement, and excess swelling, are contraindications to non-operative management of Gartland II fractures.(B2)
Non-operative management involves immobilization in a collar and cuff or an above-elbow cast with the elbow in 80 to 90 degrees of flexion for three to four weeks. Excess swelling can compromise the vascularity of the forearm and lead to compartment syndrome.[36] Above-elbow casts have been found to provide more effective pain relief than a collar and cuff for Gartland I fractures.[37] One study found that patients with Gartland II displaced fractures had satisfactory functional outcomes when managed in a cast, although some developed cubitus varus.[5] Excessive flexion should be avoided in patients with significant elbow swelling as it can cause compartment syndrome.(B2)
Traction has been used historically for displaced fractures.[38] It may be used in low-resource settings in low- and middle-income countries where there is limited access to equipment for surgical treatment.[39](A1)
Surgical Management
Surgical management is indicated for displaced Gartland II and Gartland III fractures. Urgent surgical management is indicated for patients with neurovascular compromise, compartment syndrome, and open fractures. Surgical management involves closed reduction and percutaneous pinning with K-wires for closed injuries. Open reduction may be required for failed closed reduction, irreducible fractures, and vascular exploration. Orthopedic surgeons managing these intricate fracture patterns with potential concomitant neurovascular injuries should ensure that they can handle the associated injuries and have a vascular surgeon on hand for assistance during the surgery.
Closed Reduction and Percutaneous Pinning
This is indicated for Gartland IIB and III fractures. It is also indicated for Gartland IIA fractures if an acceptable reduction is not obtained in a cast and if there are any contraindications to non-operative treatment (e.g., medial column comminution).
Closed Reduction
Closed reduction involves in-line traction with 'milking' of the soft tissues when a pucker sign is present. Traction pulls the fracture out to length, and 'milking' helps release the soft tissues. Traction should be applied with the elbow in slight flexion. This is followed by the correction of coronal plane displacement: medial/lateral translation and varus/valgus angulation of the distal fragment. Pronation with a valgus-directed force or supination with the addition of a varus force may be required, and these maneuvers also help correct rotational deformity. Pronation helps to correct posteromedial displacement (internal rotation) while tightening the medial periosteum, while supination can help correct posterolateral (external) rotation. The sagittal plane deformity is corrected by hyperflexion of the distal fragment in extension-type fractures. The extension may be required in flexion-type fractures.
The joystick technique has been described as a method to reduce multi-directionally unstable fractures.[40][34](B2)
Percutaneous Pinning Technique
Lateral pins and crossed pins (medial and lateral) bicortical constructs can be used.
Lateral pin configurations are frequently used, and they reduce the risk of iatrogenic ulnar nerve injury. Two or three lateral pins may be used. Pins must be inserted in a parallel or divergent manner with maximal separation between them. The divergent pattern is reported to be more stable than the parallel configuration.[41] For lateral pins, a capitellar starting point also provides improved construct rigidity compared to a direct lateral entry point.[42] A trans olecranon fossa four-cortex purchase has been described as a technique for lateral pinning to increase construct rigidity.[43] Pin size has been shown to affect the stability of the fixation. 2 mm pins have been found to provide improved biomechanical strength compared to 1.6mm pins.[42](B2)
The use of crossed pins increases the risk of iatrogenic ulnar nerve injury; however, they improve the torsional rigidity of the construct compared to the use of two lateral pins.[20][44] A medial incision should be made of an adequate size that will allow the protection of the ulnar nerve before inserting a medial pin.[45] The insertion of percutaneous medial pins should be avoided due to the risk of nerve injury. A further way to reduce the risk of iatrogenic ulnar nerve injury is to extend the elbow while inserting the medial pin. This maneuver displaces the nerve more posteriorly.(A1)
Open Reduction and Percutaneous Pinning
Open reduction is necessary when reduction cannot be achieved by the closed method. In particular, soft tissue/neurovascular structures can become trapped in the fracture site preventing anatomical reduction. Open reduction may also be necessary for open fractures. Exploration of the brachial artery via an open approach is required in cases where perfusion is not established peri-operatively following reduction and fixation of the fracture. Open exploration of the brachial artery in the setting of an absent radial pulse but perfused hand following reduction and fixation remains controversial.
An anterior approach has been recommended for open reduction.[46][47] Alternative approaches include medial, lateral, and posterior approaches.[48]
Vascular Exploration
Urgent vascular exploration is indicated in patients with a pulseless, pale hand. This must be performed by a surgeon experienced in repairing small vessels or in conjunction with a vascular surgeon. An attempt at closed reduction and fixation of the fracture should be performed in the first instance to see if this restores perfusion to the limb.
The management of patients with a pink, perfused, but pulseless hand following reduction and fixation remains controversial. These patients need close observation following surgery. Non-operative management has been shown to yield acceptable results.[49][50][51] Some patients with a pulseless, perfused hand may go on to develop ischemia, and this patient cohort necessitates urgent vascular exploration.[51](B2)
Differential Diagnosis
A significant proportion of the distal humerus is cartilaginous in children. Although the ossification centers appear predictably around the elbow, there may be diagnostic uncertainty in very young children. Differential diagnoses include
- Radial head fractures
- Distal humeral medial or lateral condyle fractures
- Transphyseal fractures of the distal humerus are another differential diagnosis, and non-accidental injury should be excluded in such cases.
- A pulled elbow is usually indicated from the history, and radiographs are rarely performed in these cases.
Prognosis
The prognosis depends on the remodeling potential of the bone, patient, and injury-specific factors.
Remodeling Potential
Remodeling depends on the following factors:
- The age of the patient and the amount of growth remaining
- The distance of a fracture from the physis
- Plane of deformity
- Degree of displacement
The distal humerus physis provides 20% of the longitudinal growth of the humerus. As a result, the supracondylar region of the distal humerus does not have a significant ability to remodel in cases of malunion. At the elbow, the sagittal plane deformity has better remodeling potential than the coronal plane deformity. Younger patients have more growth remaining and thus have a higher remodeling potential but only for sagittal plane deformity. Coronal plane deformity does not remodel.
Patient Factors
Children younger than five years old have better remodeling potential than those older than five.[31] After age five, children have limited residual growth of the distal humerus. Obesity is an indicator of injury severity and worse outcomes.[52][53]
Injury-Specific Factors
- Grade of injury
- Adequacy of reduction and fixation
- Neurovascular status of the limb
Appropriate treatment on time improves the long-term prognosis of these injuries. The prognosis may be worse for higher-grade injuries; however, anatomical reduction, stable fixation, and appropriate care of the soft tissues (including neurovascular injuries and compartment syndrome) improve outcomes. Nondisplaced Gartland I fractures usually heal well without complication. Gartland II fractures with medial comminution can develop cubitus varus if this is not recognized, reduced, and stabilized. Gartland III and IV injuries are more likely to be associated with neurovascular injuries; however, timely, appropriate treatment can lead to excellent outcomes.[54]
Complications
1. Neurological Injury
- 11.3% incidence of traumatic neuropraxia.[20]
- Anterior Interosseous Nerve Palsy: This is the most commonly injured nerve in extension-type supracondylar fractures.
- Median Nerve Palsy: This can be traumatic or iatrogenic in origin.
- Radial Nerve Palsy: This has been found to be more common in fractures with posteromedial displacement.[54]
- Ulnar Nerve Palsy: This is the most commonly injured nerve in flexion-type fractures.
2. Vascular Injury
- Brachial artery injury is more common in completely displaced Gartland III (and IV) injuries.[55]
3. Compartment Syndrome
- This can result in the forearm from impaired perfusion in the setting of brachial artery injury and inadequate collateral circulation.
3. Volkmann Ischaemic Contracture
- This is relatively rare.
- It can occur as a complication of forearm compartment syndrome and delayed treatment of arterial injury with resultant forearm ischemia.[55]
4. Malunion and Deformity
- Malunion can occur with resultant deformity in the sagittal, coronal and axial planes.
- Recurvatum Deformity:
- The sagittal plane deformity is more likely to remodel in younger children because this is in the plane of movement of the elbow (flexion/extension).
- This is the most common sagittal plane deformity.
- Cubitus Varus:
- Coronal and axial plane deformity have minimal remodeling potential.
- Comminution of the medial column can cause collapse, malunion, and varus deformity.
- It may also occur because of a residual internal rotation deformity.[56]
- Cubitus Valgus:
- This can occur due to inadequate reduction and malunion.
- It can lead to tardy ulnar nerve palsy.
5. Stiffness
- The range of movement rapidly improves within the first six weeks following surgery.
- The range can improve to 98% of normal within the first 12 months.[57]
- Stiffness is more commonly associated with open reduction procedures.[46]
- Long-term reduction in the range of movement is also associated with malunion.
6. Pin-site Infection
7. Pin-site Migration
Postoperative and Rehabilitation Care
Percutaneous pins can usually be removed at the 3 to 4-week point post-operatively. Children can then be allowed to commence mobilization. Children may experience some stiffness immediately following the removal of immobilization; however, this has been shown to improve rapidly in the first month after surgery. Older children regain their range of motion more slowly compared to younger children.[58] Physiotherapy has not been found to improve outcomes in a randomized controlled trial.[59]
Deterrence and Patient Education
Children and their parents/carers should be counseled about the severity and prognosis of these injuries. Nondisplaced and minimally displaced fractures have the best long-term outcomes.
Displaced fractures are more severe injuries and may result in a late deformity despite appropriate treatment. Nerve injury at the time of injury often recovers spontaneously without intervention; however, further investigation is warranted if this does not occur. Nerve injury is also a risk of surgical fixation with percutaneous pinning. Blood vessel (arterial) injury can also occur at the time of injury or surgery. Other serious complications, such as compartment syndrome, should also be highlighted. A high index of suspicion is warranted. Early, appropriate treatment improves outcomes, even in severe cases.
Pearls and Other Issues
Pearls
- The presence of a pucker sign on clinical examination indicates a more severe soft tissue injury and a high risk of neurovascular compromise.
- Refer patients with a positive posterior fat pad sign to an orthopedic surgeon for further review. This indicates the presence of an intra-articular fracture.
- In addition to standard AP and lateral views, internal oblique and external oblique views intra-operatively provide improved visualization of the medial and lateral columns for assessment of reduction.[46]
Pitfalls
- Pin placement at the fracture site needs to be maximized. Lateral pins that cross at the fracture site or crossed pins that cross in the distal fragment have little to no rotational stability.
Enhancing Healthcare Team Outcomes
Pediatric supracondylar fractures of the humerus can range from mild to severe injuries. Emergency care providers and nurses are involved in the initial assessment, triage, and management of children presenting with elbow injuries. Advanced nurse practitioners also play a crucial role in emergency care, especially in urgent care centers.[60] Nondisplaced fractures can be easily missed because much of the pediatric elbow is cartilaginous. A careful clinical and radiological examination can reveal the presence of a nondisplaced fracture. Radiographers can often provide preliminary reports of plain radiographs for emergency department patients.[61] This may benefit other healthcare providers who are less experienced at reviewing pediatric elbow radiographs. If there is any uncertainty about the diagnosis, placement of the patient in an above elbow back slab and further review by an orthopedic surgeon is recommended.
Emergency care staff play a crucial role in identifying the presence of associated neurovascular injuries and compartment syndrome following the child's arrival in the emergency department. This is very important as the neurovascular status of the limb can evolve while the child is awaiting review and treatment by an orthopedic surgeon. Besides, these patients are at risk of developing compartment syndrome, and urgent treatment is mandatory.
All members of the interprofessional team play essential roles in the management of this patient group. These fractures can be very painful. The nursing staff is often involved in assessing patients' pain status and administering analgesia.[62] All treating healthcare staff need to be aware that an increasing analgesia requirement could be a sign of compartment syndrome.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Shenoy PM,Islam A,Puri R, Current Management of Paediatric Supracondylar Fractures of the Humerus. Cureus. 2020 May 15 [PubMed PMID: 32550057]
Leung S,Paryavi E,Herman MJ,Sponseller PD,Abzug JM, Does the Modified Gartland Classification Clarify Decision Making? Journal of pediatric orthopedics. 2018 Jan; [PubMed PMID: 26974527]
Tomaszewski R,Wozowicz A,Wysocka-Wojakiewicz P, Analysis of Early Neurovascular Complications of Pediatric Supracondylar Humerus Fractures: A Long-Term Observation. BioMed research international. 2017; [PubMed PMID: 28367440]
Pannu GS,Eberson CP,Abzug J,Horn BD,Bae DS,Herman M, Common Errors in the Management of Pediatric Supracondylar Humerus Fractures and Lateral Condyle Fractures. Instructional course lectures. 2016; [PubMed PMID: 27049207]
Moraleda L,Valencia M,Barco R,González-Moran G, Natural history of unreduced Gartland type-II supracondylar fractures of the humerus in children: a two to thirteen-year follow-up study. The Journal of bone and joint surgery. American volume. 2013 Jan 2; [PubMed PMID: 23405411]
Level 2 (mid-level) evidenceHammond WA,Kay RM,Skaggs DL, Supracondylar humerus fractures in children. AORN journal. 1998 Aug; [PubMed PMID: 9706234]
Level 3 (low-level) evidenceMostafa E,Imonugo O,Varacallo M, Anatomy, Shoulder and Upper Limb, Humerus . 2020 Jan [PubMed PMID: 30521242]
Barr LV, Paediatric supracondylar humeral fractures: epidemiology, mechanisms and incidence during school holidays. Journal of children's orthopaedics. 2014 Mar; [PubMed PMID: 24643672]
Landin LA,Danielsson LG, Elbow fractures in children. An epidemiological analysis of 589 cases. Acta orthopaedica Scandinavica. 1986 Aug [PubMed PMID: 3788491]
Level 2 (mid-level) evidenceFarnsworth CL,Silva PD,Mubarak SJ, Etiology of supracondylar humerus fractures. Journal of pediatric orthopedics. 1998 Jan-Feb [PubMed PMID: 9449099]
Holt JB,Glass NA,Shah AS, Understanding the Epidemiology of Pediatric Supracondylar Humeral Fractures in the United States: Identifying Opportunities for Intervention. Journal of pediatric orthopedics. 2018 May/Jun; [PubMed PMID: 29462120]
Level 3 (low-level) evidenceSkaggs D,Pershad J, Pediatric elbow trauma. Pediatric emergency care. 1997 Dec; [PubMed PMID: 9435010]
Nork SE,Hennrikus WL,Loncarich DP,Gillingham BL,Lapinsky AS, Relationship between ligamentous laxity and the site of upper extremity fractures in children: extension supracondylar fracture versus distal forearm fracture. Journal of pediatric orthopedics. Part B. 1999 Apr [PubMed PMID: 10218167]
Anjum R,Sharma V,Jindal R,Singh TP,Rathee N, Epidemiologic pattern of paediatric supracondylar fractures of humerus in a teaching hospital of rural India: A prospective study of 263 cases. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2017 Jun; [PubMed PMID: 28511800]
Level 3 (low-level) evidenceAbraham E,Powers T,Witt P,Ray RD, Experimental hyperextension supracondylar fractures in monkeys. Clinical orthopaedics and related research. 1982 Nov-Dec [PubMed PMID: 6814805]
Level 3 (low-level) evidenceDuffy S,Flannery O,Gelfer Y,Monsell F, Overview of the contemporary management of supracondylar humeral fractures in children. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2021 Jul [PubMed PMID: 33744996]
Level 3 (low-level) evidenceSmuin D,Hatch M,Winthrop Z,Gidvani S,Hennrikus W, The Reduction Maneuver for Pediatric Extension Type 3 Supracondylar Humerus Fractures. Cureus. 2020 Jul 15 [PubMed PMID: 32821565]
Flaherty EG,Perez-Rossello JM,Levine MA,Hennrikus WL,American Academy of Pediatrics Committee on Child Abuse and Neglect,Section on Radiology, American Academy of Pediatrics,Section on Endocrinology, American Academy of Pediatrics,Section on Orthopaedics, American Academy of Pediatrics,Society for Pediatric Radiology, Evaluating children with fractures for child physical abuse. Pediatrics. 2014 Feb [PubMed PMID: 24470642]
Smuin DM,Hennrikus WL, The Effect of the Pucker Sign on Outcomes of Type III Extension Supracondylar Fractures in Children. Journal of pediatric orthopedics. 2017 Jun [PubMed PMID: 27776053]
Babal JC,Mehlman CT,Klein G, Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. Journal of pediatric orthopedics. 2010 Apr-May; [PubMed PMID: 20357592]
Level 1 (high-level) evidenceCampbell CC,Waters PM,Emans JB,Kasser JR,Millis MB, Neurovascular injury and displacement in type III supracondylar humerus fractures. Journal of pediatric orthopedics. 1995 Jan-Feb; [PubMed PMID: 7883927]
Level 2 (mid-level) evidenceMangat KS,Martin AG,Bache CE, The 'pulseless pink' hand after supracondylar fracture of the humerus in children: the predictive value of nerve palsy. The Journal of bone and joint surgery. British volume. 2009 Nov; [PubMed PMID: 19880900]
Miyazaki CS,Maranho DA,Agnollitto PM,Nogueira-Barbosa MH, STUDY OF SECONDARY OSSIFICATION CENTERS OF THE ELBOW IN THE BRAZILIAN POPULATION. Acta ortopedica brasileira. 2017 Nov-Dec; [PubMed PMID: 29375260]
Williamson DM,Coates CJ,Miller RK,Cole WG, Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. Journal of pediatric orthopedics. 1992 Sep-Oct [PubMed PMID: 1517426]
Smajic N,Smajic J,Sadic S,Jasarevic M,Ahmetovic-Djug J,Hodzic R, Correlation between Bauman's and carrying angle in children with supracondylar fracture of humerus. Medical archives (Sarajevo, Bosnia and Herzegovina). 2013 [PubMed PMID: 23848042]
Level 2 (mid-level) evidenceSilva M,Pandarinath R,Farng E,Park S,Caneda C,Fong YJ,Penman A, Inter- and intra-observer reliability of the Baumann angle of the humerus in children with supracondylar humeral fractures. International orthopaedics. 2010 Apr [PubMed PMID: 19424695]
Samelis PV,Papagrigorakis E,Ellinas S, Role of the Posterior Fat Pad Sign in Treating Displaced Extension Type Supracondylar Fractures of the Pediatric Elbow Using the Blount Method. Cureus. 2019 Oct 29 [PubMed PMID: 31824792]
Herman MJ,Boardman MJ,Hoover JR,Chafetz RS, Relationship of the anterior humeral line to the capitellar ossific nucleus: variability with age. The Journal of bone and joint surgery. American volume. 2009 Sep [PubMed PMID: 19723996]
Level 2 (mid-level) evidenceAbzug JM,Herman MJ, Management of supracondylar humerus fractures in children: current concepts. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Feb [PubMed PMID: 22302444]
Shaw BA,Kasser JR,Emans JB,Rand FF, Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. Journal of orthopaedic trauma. 1990; [PubMed PMID: 2313426]
Omid R,Choi PD,Skaggs DL, Supracondylar humeral fractures in children. The Journal of bone and joint surgery. American volume. 2008 May; [PubMed PMID: 18451407]
GARTLAND JJ, Management of supracondylar fractures of the humerus in children. Surgery, gynecology [PubMed PMID: 13675986]
Alton TB,Werner SE,Gee AO, Classifications in brief: the Gartland classification of supracondylar humerus fractures. Clinical orthopaedics and related research. 2015 Feb; [PubMed PMID: 25361847]
Leitch KK,Kay RM,Femino JD,Tolo VT,Storer SK,Skaggs DL, Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. The Journal of bone and joint surgery. American volume. 2006 May; [PubMed PMID: 16651572]
Level 2 (mid-level) evidenceLabelle H,Bunnell WP,Duhaime M,Poitras B, Cubitus varus deformity following supracondylar fractures of the humerus in children. Journal of pediatric orthopedics. 1982; [PubMed PMID: 7161389]
Level 2 (mid-level) evidenceBattaglia TC,Armstrong DG,Schwend RM, Factors affecting forearm compartment pressures in children with supracondylar fractures of the humerus. Journal of pediatric orthopedics. 2002 Jul-Aug; [PubMed PMID: 12131436]
Ballal MS,Garg NK,Bass A,Bruce CE, Comparison between collar and cuffs and above elbow back slabs in the initial treatment of Gartland type I supracondylar humerus fractures. Journal of pediatric orthopedics. Part B. 2008 Mar; [PubMed PMID: 18510158]
Jones D, Transcondylar fractures of the humerus in children: definition of an acceptable reduction. Proceedings of the Royal Society of Medicine. 1977 Sep; [PubMed PMID: 918083]
Level 3 (low-level) evidenceYeomans D,Graham SM,Mkandawire NC,Harrison WJ,Perry DC, Conservative management of displaced paediatric supracondylar fractures: a systematic review. Tropical doctor. 2018 Oct; [PubMed PMID: 30153770]
Level 1 (high-level) evidenceNovais EN,Andrade MA,Gomes DC, The use of a joystick technique facilitates closed reduction and percutaneous fixation of multidirectionally unstable supracondylar humeral fractures in children. Journal of pediatric orthopedics. 2013 Jan; [PubMed PMID: 23232373]
Level 2 (mid-level) evidenceLee SS,Mahar AT,Miesen D,Newton PO, Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. Journal of pediatric orthopedics. 2002 Jul-Aug; [PubMed PMID: 12131437]
Gottschalk HP,Sagoo D,Glaser D,Doan J,Edmonds EW,Schlechter J, Biomechanical analysis of pin placement for pediatric supracondylar humerus fractures: does starting point, pin size, and number matter? Journal of pediatric orthopedics. 2012 Jul-Aug; [PubMed PMID: 22706457]
Level 2 (mid-level) evidenceKasirajan S,Govindasamy R,Sathish BRJ,Meleppuram JJ, Trans-olecranon fossa four-cortex purchase lateral pinning in displaced supracondylar fracture of the humerus - a prospective analysis in 48 children. Revista brasileira de ortopedia. 2018 May-Jun; [PubMed PMID: 29892587]
Zionts LE,McKellop HA,Hathaway R, Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. The Journal of bone and joint surgery. American volume. 1994 Feb; [PubMed PMID: 8113261]
Green DW,Widmann RF,Frank JS,Gardner MJ, Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. Journal of orthopaedic trauma. 2005 Mar; [PubMed PMID: 15758668]
Level 2 (mid-level) evidenceVaquero-Picado A,González-Morán G,Moraleda L, Management of supracondylar fractures of the humerus in children. EFORT open reviews. 2018 Oct; [PubMed PMID: 30662761]
Koudstaal MJ,De Ridder VA,De Lange S,Ulrich C, Pediatric supracondylar humerus fractures: the anterior approach. Journal of orthopaedic trauma. 2002 Jul; [PubMed PMID: 12142829]
Ersan O,Gonen E,İlhan RD,Boysan E,Ates Y, Comparison of anterior and lateral approaches in the treatment of extension-type supracondylar humerus fractures in children. Journal of pediatric orthopedics. Part B. 2012 Mar; [PubMed PMID: 22158013]
Cambon-Binder A,Jehanno P,Tribout L,Valenti P,Simon AL,Ilharreborde B,Mazda K, Pulseless supracondylar humeral fractures in children: vascular complications in a ten year series. International orthopaedics. 2018 Apr; [PubMed PMID: 29192344]
Ramesh P,Avadhani A,Shetty AP,Dheenadhayalan J,Rajasekaran S, Management of acute 'pink pulseless' hand in pediatric supracondylar fractures of the humerus. Journal of pediatric orthopedics. Part B. 2011 May; [PubMed PMID: 21164361]
Level 2 (mid-level) evidenceWeller A,Garg S,Larson AN,Fletcher ND,Schiller JR,Kwon M,Copley LA,Browne R,Ho CA, Management of the pediatric pulseless supracondylar humeral fracture: is vascular exploration necessary? The Journal of bone and joint surgery. American volume. 2013 Nov 6; [PubMed PMID: 24196459]
Level 2 (mid-level) evidenceChang CH,Kao HK,Lee WC,Yang WE, Influence of obesity on surgical outcomes in type III paediatric supracondylar humeral fractures. Injury. 2015 Nov; [PubMed PMID: 26429104]
Seeley MA,Gagnier JJ,Srinivasan RC,Hensinger RN,VanderHave KL,Farley FA,Caird MS, Obesity and its effects on pediatric supracondylar humeral fractures. The Journal of bone and joint surgery. American volume. 2014 Feb 5; [PubMed PMID: 24500590]
Level 2 (mid-level) evidenceWang SI,Kwon TY,Hwang HP,Kim JR, Functional outcomes of Gartland III supracondylar humerus fractures with early neurovascular complications in children: A retrospective observational study. Medicine. 2017 Jun; [PubMed PMID: 28640089]
Level 2 (mid-level) evidenceBlakey CM,Biant LC,Birch R, Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow-up. The Journal of bone and joint surgery. British volume. 2009 Nov; [PubMed PMID: 19880895]
Level 3 (low-level) evidenceBender J,Busch CA, Results of treatment of supracondylar fractures of the humerus in children with special reference to the cause and prevention of cubitus varus. Archivum chirurgicum Neerlandicum. 1978; [PubMed PMID: 655730]
Zionts LE,Woodson CJ,Manjra N,Zalavras C, Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clinical orthopaedics and related research. 2009 Aug; [PubMed PMID: 19198963]
Level 2 (mid-level) evidenceSpencer HT,Wong M,Fong YJ,Penman A,Silva M, Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. The Journal of bone and joint surgery. American volume. 2010 Apr; [PubMed PMID: 20360514]
Schmale GA,Mazor S,Mercer LD,Bompadre V, Lack of Benefit of Physical Therapy on Function Following Supracondylar Humeral Fracture: A Randomized Controlled Trial. The Journal of bone and joint surgery. American volume. 2014 Jun 4; [PubMed PMID: 24897743]
Level 1 (high-level) evidenceWoo BFY,Lee JXY,Tam WWS, The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: a systematic review. Human resources for health. 2017 Sep 11; [PubMed PMID: 28893270]
Level 2 (mid-level) evidenceBrown C,Neep MJ,Pozzias E,McPhail SM, Reducing risk in the emergency department: a 12-month prospective longitudinal study of radiographer preliminary image evaluations. Journal of medical radiation sciences. 2019 Sep; [PubMed PMID: 31449740]
Porter RN,Chafe RE,Newhook LA,Murnaghan KD, Multiple interventions improve analgesic treatment of supracondylar humerus fractures in a pediatric emergency department. Pain research [PubMed PMID: 26125193]