Introduction
A pneumothorax, also known as a collapsed lung, occurs when air (either from the lung or outside) collects in the space between the lung and the chest wall. This condition can present in 1 of 3 ways: spontaneous (primary), secondary, and traumatic. This activity focuses on a subset of traumatic pneumothoraces known as iatrogenic pneumothorax. This refers to a pneumothorax developed secondary to an invasive procedure such as a pulmonary needle biopsy (transthoracic and transbronchial), a central venous line placement, or positive pressure ventilation.[1] As a complication of an invasive procedure, a tension pneumothorax can develop when the pressure in the pleural space is positive throughout the respiratory cycle. This leads to decreased venous return, hypotension, and hypoxia. A pneumothorax can range from asymptomatic to potentially life-threatening. Iatrogenic pneumothorax is a patient safety indicator (PSI) of the above procedures.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
An iatrogenic pneumothorax is a known complication of invasive procedures such as pulmonary needle biopsy (transthoracic and transbronchial), placement of a central venous line, or positive pressure ventilation.[1] However, this condition can arise from many other thorax and abdomen procedures. Case reports include bilateral pneumothoraces after incorrect placement of a nebulization kit in a spontaneously breathing intubated patient,[2] after insertion of a hypoglossal nerve stimulator,[3] or even after acupuncture.[4] However, subclavian insertion of a central venous line (CVL) is the most common procedure associated with an iatrogenic pneumothorax.[5]
Epidemiology
The incidence of an iatrogenic pneumothorax is directly proportional to the number of invasive procedures performed.[6] Patients in unstable trauma or code situations are more likely to undergo an invasive intervention. This, along with limited access to internal jugular sites when a nonfemoral vein site is desired, results in an elevated risk for iatrogenic pneumothorax.[5]
Pathophysiology
Any intervention in proximity to the abdomen, especially the thorax, can cause an iatrogenic pneumothorax. This is especially true when placing a subclavian central venous catheter without ultrasound (ie, "blindly") using landmarks. In landmark-based subclavian central venous catheter placement, per Kilbourne et al,[7] 6 common technical errors include inadequate landmark identification, improper insertion position, insertion of the needle through periosteum, too shallow a trajectory with the needle, the needle aim being too cephalad, and failure to keep the needle in place for wire passage. Landmark technique also depends on the ability and experience of the medical professional performing the procedure, making iatrogenic pneumothorax more likely in a tertiary teaching hospital.[8]
History and Physical
The presentation in a patient with a pneumothorax can range from asymptomatic to life-threatening based on the size, rate of development, and health of the underlying lung. An iatrogenic pneumothorax is part of a differential diagnosis in a patient with pleuritic pain and dyspnea, tachypnea, and tachycardia. Decreased or absent breath sounds on the affected side are highly suspicious. Any pneumothorax can become a tension pneumothorax. Findings could include hypoxia, hypotension, distended neck veins, a displaced trachea, and unilaterally decreased breath sounds.[9]
Evaluation
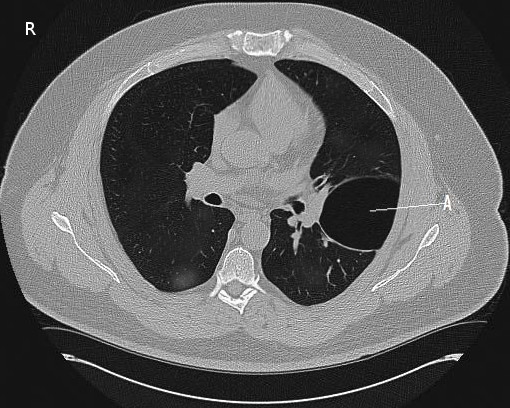
Iatrogenic pneumothorax can be diagnosed clinically. Point-of-care ultrasound has the advantage of being rapid, highly sensitive, specific, and easily repeatable. Suggestive findings include the lack of pleural sliding. A "point sign" (sliding pleural next to nonsliding pleura) is diagnostic. Upright posteroanterior chest radiography has 83% sensitivity (see Image. Left Pneumothorax on X-ray).[9] Chest CT is more sensitive than chest radiography but inherently results in a delay in treatment (see Image. CT Scan, Pneumothorax).
Treatment / Management
First, determine if the patient is stable or unstable. Next, supplemental oxygen at a rate that maintains adequate oxygenation is provided.[10] Some patients with small pneumothoraces may resolve with observation.[11] Definitive treatment options for a pneumothorax include needle aspiration, chest tube drainage, video-assisted thoracic surgery (VATS), and open surgical intervention.[12] Treatment takes precedence over imaging. If felt to be clinically unstable, the traditional first step is to perform a needle aspiration or decompression to reduce the excess air in the pleural space. As a temporary measure, place a large-bore needle in the second intercostal space in the midclavicular line.[13][14] Finger thoracostomy is the most recently used technique. One makes an incision over the lateral chest wall in the "safe triangle" formed by the lateral border of the pectoralis major, the lateral border of the latissimus dorsi, the fifth intercostal space, and the base of the axilla. Next, one inserts a finger over the fifth intercostal space and bluntly dissects into the pleural space. It is fast and safe as it does not cause a pneumothorax and addresses the increasing girth of today's patients. Thoracostomy is the definitive therapy and uses the negative pressure generated by a water seal or suction to reduce air in the pleural space.[15] Chest tubes are inserted in the midclavicular line's second or third intercostal space (Monaldi position). Chest tubes can also be inserted anterior to the midaxillary line of the fourth or fifth intercostal space (Bulau position).[16] The other 2 treatment choices are purely surgical and reserved for severe cases.[17](A1)
Management Algorithm for Iatrogenic Pneumothorax
-
Assessment of patient stability: Determine if the patient is stable or unstable. If unstable, proceed to immediate needle decompression.
-
Oxygenation: Provide supplemental oxygen at a rate to maintain adequate oxygenation.
-
Observation for small pneumothoraces: Some patients with small pneumothoraces may resolve with observation.
-
Definitive treatment options:
- Needle aspiration
- Chest tube drainage
- VATS
- Open surgical intervention
-
Prioritization of treatment over imaging: Treatment takes precedence over imaging.
-
Initial management for clinically unstable patients: Perform needle aspiration or decompression to reduce excess air in the pleural space. As a temporary measure, place a large-bore needle in the second intercostal space in the midclavicular line.
-
Finger thoracostomy: If finger thoracostomy is needed, make an incision over the lateral chest wall in the "safe triangle" formed by the lateral border of the pectoralis major, the lateral border of the latissimus dorsi, the fifth intercostal space, and the base of the axilla. Insert a finger over the fifth intercostal space and bluntly dissect into the pleural space.
-
Definitive therapy: Thoracostomy is definitive therapy. Use negative pressure from a water seal or suction to reduce air in the pleural space. Chest tubes are inserted in either the second or third intercostal space of the midclavicular line (Monaldi position) or anterior to the mid-axillary line of the fourth or fifth intercostal space (Bulau position).
-
Surgical intervention: Surgical interventions for severe cases are VATS and open surgical intervention.
Differential Diagnosis
Although the diagnosis of pneumothorax should be definite and precise, a patient presenting with pleuritic pain without further management should elicit a robust differential diagnosis such as one of the following:
- Myocardial infarct
- Myocardial ischemia
- Pulmonary embolus
- Pericarditis
- Pleurisy
- Pneumonia [10]
Pertinent Studies and Ongoing Trials
Given that iatrogenic pneumothorax is a PSI that is directly related to invasive procedures, most of the pertinent studies and ongoing trials focus on quality improvement and incidence reduction. Central venous catheter insertion is the main cause of iatrogenic pneumothoraces. Therefore, patient factors (eg, underlying condition, anatomy, restlessness, previous procedures), procedure decision-making factors (eg, site or catheter type), and clinical factors influence outcomes.[18]
A quality improvement observational study in a tertiary care hospital demonstrated improvement and a sustained reduction of iatrogenic cases through a multifaceted intervention. This consisted of clinical and documentation standardization, the addition of cognitive aids, simulator training, the use of ultrasound equipment, and feedback to clinical services.[5] Other studies have linked physicians-in-training to worse outcomes due to lack of experience;[8] however, simulation-based mastery has improved patient outcomes.[19]
Prognosis
The estimated risk of pneumothorax recurrence is 23% to 50% over a 1- to 5-year follow-up period, with the highest risk during the first month.[20] However, no data for recurrence or incidence changes specific to iatrogenic pneumothoraces exists. In patients who underwent tube thoracostomy, it is safe to fly as early as 72 hours after tube removal without increased risk of recurrence.[21]
Complications
Tension pneumothorax is the most notable complication of any pneumothorax previously described. This disorder is life-threatening and requires immediate intervention.[22] Another well-described complication of pneumothorax is having a persistent air leak and failure of lung re-expansion, which usually requires further surgical intervention.[23]
Deterrence and Patient Education
A pneumothorax, also known as a collapsed lung, occurs when air (either from the lung or outside) collects in the space between the lung and the chest wall. A collapsed lung caused accidentally during a procedure is called an iatrogenic pneumothorax. Symptoms of a collapsed lung include sharp or stabbing chest pain and trouble breathing. People with small amounts of trapped air may not have any symptoms.
This condition can be an emergency and require immediate treatment. Treatment involves extracting the air trapped between the lung and the chest wall by either a needle, scalpel, finger, or chest tube. Regardless, an inserted chest tube stays in place until the lung expands to its normal size. Some individuals with severe cases may require surgery. After being treated for a collapsed lung with a tube, the chances of having a recurrence are low but possible. Patients should avoid scuba diving and flying in a plane for at least 72 hours.[24]
Pearls and Other Issues
Key facts to keep in mind regarding iatrogenic pneumothorax are as follows:
- Iatrogenic pneumothorax is a PSI condition. It is a traumatic pneumothorax secondary to an invasive procedure or surgery.
- The most common cause is a subclavian central venous line placement.
- Other causes include pulmonary needle biopsy (transthoracic and transbronchial), nasogastric tube placement, or positive pressure ventilation. There are case reports after placing nebulizer kits and acupuncture on the chest wall.
- The presentation is mainly pleuritic chest pain and dyspnea with decreased to absent breath sounds on the affected side during or after a procedure.
- Treatment should not be delayed for imaging.
- The diagnosis is ideally made clinically. Ultrasound evaluation to check for pneumothorax is emerging as a very accurate and rapid tool.
- Treatment is needle decompression followed by tube thoracostomy. VATS and open thoracotomy are reserved for recurrent or severe cases.
Enhancing Healthcare Team Outcomes
Iatrogenic pneumothorax is an important PSI condition associated with morbidity and mortality. Iatrogenic pneumothoraces are attributed to suboptimal procedure techniques/decision-making pitfalls, lack of medical provider experience, and lack of ultrasound use during CVC placement.[25] Clinicians should prioritize the cautious insertion of medical devices, such as central venous catheters and chest tubes, to mitigate the risk of iatrogenic pneumothorax—a potentially serious complication. Clinicians should utilize imaging guidance, like ultrasound, to enhance precision during procedures, avoiding inadvertent lung puncture. The proper technique and regular reassessment of needle or tube placement minimize complications. A high level of awareness for patient-specific factors, such as underlying lung conditions, that may increase susceptibility should be maintained. Adherence to stringent aseptic practices and ongoing education on best practices are crucial for preventing iatrogenic pneumothorax in clinical settings.
In managing iatrogenic pneumothorax, clinicians should promptly recognize symptoms, including respiratory distress and chest pain. The diagnosis should be confirmed and the severity of the condition gauged through imaging (eg, chest x-ray). Small, asymptomatic cases may resolve spontaneously, but more significant or symptomatic pneumothoraces require intervention. Clinicians should opt for conservative measures like observation or supplemental oxygen if the pneumothorax is minor. Needle aspiration or chest tube insertion to evacuate air and re-establish lung expansion should be considered for more severe cases. Clinicians should regularly reassess the patient's respiratory status and adjust treatment accordingly, ensuring a tailored approach for optimal recovery.
Collaboration within an interprofessional team is imperative to cultivate a safety culture and mitigate the risk of iatrogenic pneumothorax. Clear communication among physicians, advanced practitioners, nurses, and specialists ensures comprehensive patient assessment, minimizing procedural errors. Regular interdisciplinary training promotes standardized protocols and enhances collective awareness of potential complications. Systematic reviews have focused on the role of simulation-based education, addressing all the common causes. This training results in the improvement of CVC techniques and the reduction of iatrogenic pneumothorax cases.[26][27][28]
In an academic tertiary care hospital, an interprofessional team, including physicians, nurses, and administrative leaders, improved and sustained a reduction in iatrogenic pneumothoraces. This was performed by implementing clinical documentation standards, cognitive aids, simulation training, purchase/employment of ultrasound equipment, and feedback to clinical services.[5] The role of interprofessional communication and care coordination between health professionals cannot be understated when considering patient outcomes.
Emphasizing a shared responsibility for patient safety encourages open dialogue, enabling quick identification and resolution of issues. By fostering a collaborative approach, healthcare teams can proactively address risk factors, implement preventive measures, and collectively strive for optimal patient outcomes, reducing the incidence of iatrogenic pneumothorax in clinical settings.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Loiselle A, Parish JM, Wilkens JA, Jaroszewski DE. Managing iatrogenic pneumothorax and chest tubes. Journal of hospital medicine. 2013 Jul:8(7):402-8. doi: 10.1002/jhm.2053. Epub 2013 Jun 14 [PubMed PMID: 23765922]
Garg SK, Garg P, Anchan N, Jaiswal A. Iatrogenic Bilateral Simultaneous Pneumothorax: Call for Vigilance. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2017 Sep:21(9):607-609. doi: 10.4103/ijccm.IJCCM_108_17. Epub [PubMed PMID: 28970663]
Arteaga AA, Pitts KD, Lewis AF. Iatrogenic pneumothorax during hypoglossal nerve stimulator implantation. American journal of otolaryngology. 2018 Sep-Oct:39(5):636-638. doi: 10.1016/j.amjoto.2018.06.014. Epub 2018 Jun 14 [PubMed PMID: 29941192]
Tagami R, Moriya T, Kinoshita K, Tanjoh K. Bilateral tension pneumothorax related to acupuncture. Acupuncture in medicine : journal of the British Medical Acupuncture Society. 2013 Jun:31(2):242-4. doi: 10.1136/acupmed-2012-010284. Epub 2013 Feb 28 [PubMed PMID: 23449179]
Level 3 (low-level) evidenceShieh L, Go M, Gessner D, Chen JH, Hopkins J, Maggio P. Improving and sustaining a reduction in iatrogenic pneumothorax through a multifaceted quality-improvement approach. Journal of hospital medicine. 2015 Sep:10(9):599-607. doi: 10.1002/jhm.2388. Epub 2015 Jun 3 [PubMed PMID: 26041246]
Level 2 (mid-level) evidenceCelik B, Sahin E, Nadir A, Kaptanoglu M. Iatrogenic pneumothorax: etiology, incidence and risk factors. The Thoracic and cardiovascular surgeon. 2009 Aug:57(5):286-90. doi: 10.1055/s-0029-1185365. Epub 2009 Jul 23 [PubMed PMID: 19629891]
Level 2 (mid-level) evidenceKilbourne MJ, Bochicchio GV, Scalea T, Xiao Y. Avoiding common technical errors in subclavian central venous catheter placement. Journal of the American College of Surgeons. 2009 Jan:208(1):104-9. doi: 10.1016/j.jamcollsurg.2008.09.025. Epub [PubMed PMID: 19228511]
John J, Seifi A. Incidence of iatrogenic pneumothorax in the United States in teaching vs. non-teaching hospitals from 2000 to 2012. Journal of critical care. 2016 Aug:34():66-8. doi: 10.1016/j.jcrc.2016.03.013. Epub 2016 Mar 31 [PubMed PMID: 27288612]
Swierzy M, Helmig M, Ismail M, Rückert J, Walles T, Neudecker J. [Pneumothorax]. Zentralblatt fur Chirurgie. 2014 Sep:139 Suppl 1():S69-86; quiz S87. doi: 10.1055/s-0034-1383029. Epub 2014 Sep 29 [PubMed PMID: 25264729]
Haynes D, Baumann MH. Management of pneumothorax. Seminars in respiratory and critical care medicine. 2010 Dec:31(6):769-80. doi: 10.1055/s-0030-1269837. Epub 2011 Jan 6 [PubMed PMID: 21213209]
Hefny AF, Kunhivalappil FT, Matev N, Avila NA, Bashir MO, Abu-Zidan FM. Management of computed tomography-detected pneumothorax in patients with blunt trauma: experience from a community-based hospital. Singapore medical journal. 2018 Mar:59(3):150-154. doi: 10.11622/smedj.2017074. Epub 2017 Jul 25 [PubMed PMID: 28741012]
Tupchong K. Update: Is Needle Aspiration Better Than Chest Tube Placement for the Management of Primary Spontaneous Pneumothorax? Annals of emergency medicine. 2018 Jul:72(1):e1-e2. doi: 10.1016/j.annemergmed.2018.02.025. Epub 2018 Apr 1 [PubMed PMID: 29615265]
Bruschettini M, Romantsik O, Ramenghi LA, Zappettini S, O'Donnell CP, Calevo MG. Needle aspiration versus intercostal tube drainage for pneumothorax in the newborn. The Cochrane database of systematic reviews. 2016 Jan 11:(1):CD011724. doi: 10.1002/14651858.CD011724.pub2. Epub 2016 Jan 11 [PubMed PMID: 26751585]
Level 1 (high-level) evidenceNaik ND, Hernandez MC, Anderson JR, Ross EK, Zielinski MD, Aho JM. Needle Decompression of Tension Pneumothorax with Colorimetric Capnography. Chest. 2017 Nov:152(5):1015-1020. doi: 10.1016/j.chest.2017.04.179. Epub 2017 May 10 [PubMed PMID: 28499514]
Wang C, Lyu M, Zhou J, Liu Y, Ji Y. Chest tube drainage versus needle aspiration for primary spontaneous pneumothorax: which is better? Journal of thoracic disease. 2017 Oct:9(10):4027-4038. doi: 10.21037/jtd.2017.08.140. Epub [PubMed PMID: 29268413]
Drinhaus H, Annecke T, Hinkelbein J. [Chest decompression in emergency medicine and intensive care]. Der Anaesthesist. 2016 Oct:65(10):768-775 [PubMed PMID: 27629501]
Delpy JP, Pagès PB, Mordant P, Falcoz PE, Thomas P, Le Pimpec-Barthes F, Dahan M, Bernard A, EPITHOR project (French Society of Thoracic and Cardiovascular Surgery), EPITHOR project French Society of Thoracic and Cardiovascular Surgery. Surgical management of spontaneous pneumothorax: are there any prognostic factors influencing postoperative complications? European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2016 Mar:49(3):862-7. doi: 10.1093/ejcts/ezv195. Epub 2015 Jun 12 [PubMed PMID: 26071433]
Tsotsolis N, Tsirgogianni K, Kioumis I, Pitsiou G, Baka S, Papaiwannou A, Karavergou A, Rapti A, Trakada G, Katsikogiannis N, Tsakiridis K, Karapantzos I, Karapantzou C, Barbetakis N, Zissimopoulos A, Kuhajda I, Andjelkovic D, Zarogoulidis K, Zarogoulidis P. Pneumothorax as a complication of central venous catheter insertion. Annals of translational medicine. 2015 Mar:3(3):40. doi: 10.3978/j.issn.2305-5839.2015.02.11. Epub [PubMed PMID: 25815301]
Barsuk JH, Cohen ER, Williams MV, Scher J, Jones SF, Feinglass J, McGaghie WC, O'Hara K, Wayne DB. Simulation-Based Mastery Learning for Thoracentesis Skills Improves Patient Outcomes: A Randomized Trial. Academic medicine : journal of the Association of American Medical Colleges. 2018 May:93(5):729-735. doi: 10.1097/ACM.0000000000001965. Epub [PubMed PMID: 29068818]
Level 1 (high-level) evidenceBaumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA, AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001 Feb:119(2):590-602 [PubMed PMID: 11171742]
Level 1 (high-level) evidenceZonies D, Elterman J, Burns C, Paul V, Oh J, Cannon J. Trauma patients are safe to fly 72 hours after tube thoracostomy removal. The journal of trauma and acute care surgery. 2018 Sep:85(3):491-494. doi: 10.1097/TA.0000000000001976. Epub [PubMed PMID: 29782482]
Roberts DJ, Leigh-Smith S, Faris PD, Blackmore C, Ball CG, Robertson HL, Dixon E, James MT, Kirkpatrick AW, Kortbeek JB, Stelfox HT. Clinical Presentation of Patients With Tension Pneumothorax: A Systematic Review. Annals of surgery. 2015 Jun:261(6):1068-78. doi: 10.1097/SLA.0000000000001073. Epub [PubMed PMID: 25563887]
Level 1 (high-level) evidenceSlade M. Management of pneumothorax and prolonged air leak. Seminars in respiratory and critical care medicine. 2014 Dec:35(6):706-14. doi: 10.1055/s-0034-1395502. Epub 2014 Dec 2 [PubMed PMID: 25463161]
Imran JB, Eastman AL. Pneumothorax. JAMA. 2017 Sep 12:318(10):974. doi: 10.1001/jama.2017.10476. Epub [PubMed PMID: 28898380]
Giacomini M, Iapichino G, Armani S, Cozzolino M, Brancaccio D, Gallieni M. How to avoid and manage a pneumothorax. The journal of vascular access. 2006 Jan-Mar:7(1):7-14 [PubMed PMID: 16596523]
Soffler MI, Hayes MM, Smith CC. Central venous catheterization training: current perspectives on the role of simulation. Advances in medical education and practice. 2018:9():395-403. doi: 10.2147/AMEP.S142605. Epub 2018 May 25 [PubMed PMID: 29872360]
Level 3 (low-level) evidenceMa IW, Brindle ME, Ronksley PE, Lorenzetti DL, Sauve RS, Ghali WA. Use of simulation-based education to improve outcomes of central venous catheterization: a systematic review and meta-analysis. Academic medicine : journal of the Association of American Medical Colleges. 2011 Sep:86(9):1137-47. doi: 10.1097/ACM.0b013e318226a204. Epub [PubMed PMID: 21785310]
Level 1 (high-level) evidenceSekiguchi H, Tokita JE, Minami T, Eisen LA, Mayo PH, Narasimhan M. A prerotational, simulation-based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest. 2011 Sep:140(3):652-658. doi: 10.1378/chest.10-3319. Epub 2011 Jun 9 [PubMed PMID: 21659429]