Introduction
Tibial eminence fractures are uncommon injuries. The condition affects children and adolescents more than adults. Subchondral weakness in the pediatric population causes the anterior cruciate ligament (ACL) insertion site to break.[1]
Considered an ACL injury-equivalent in children, this fracture pattern was first described by Poncet in 1875.[2] The anatomic structure primarily involves the tibial eminence, a nonarticular region located between the condylar surfaces of the tibial plateaus. The ACL inserts 10 to 14 mm posterior to the anterior tibial border and is deeply attached to the subchondral plate.[3] Tibial eminence injury may cause the knee to lose biomechanical function and stability.
As the fracture is an ACL injury-equivalent, this condition can involve neighboring ligaments. The anterior horn of the medial and lateral menisci and the intermeniscal ligament lie anterior to the tibial eminence. Disruption of the tibial eminence can easily entrap these structures when the fracture fragment elevates superiorly.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Historically, tibial eminence fractures most commonly occurred in pediatric patients who fell off of a bike. However, this fracture type has a similar injury mechanism as a mid-substance ACL tear in young adult athletes. Consequently, sports collisions have become another frequent cause of this condition, with increasing athletic participation among young people. Other possible causes include motor vehicle accidents or low-impact injuries where the knee is flexed and the tibia is internally rotated.
In a tibial eminence injury, the compressive forces fracture the bone but leave the ACL intact, causing a break through the cancellous bone below the subchondral plate. Skak et al previously reported that deformation stress from the pediatric distal femur is more likely to damage the tibial eminence than the attached ligaments.[5] A retrospective study found that increased posterior tibial slope may be a risk factor for developing a tibial eminence fracture.[6]
Epidemiology
Tibial eminence fractures are rare injuries, affecting 3 in every 100,000 children who sustain knee injuries per year. This fracture type most commonly affects patients aged 8 to 14 years. These fractures account for 2% to 5% of pediatric knee injuries.[7][8] Overall, tibial eminence fractures constitute 14% of ACL injuries. As much as 40% of tibial eminence fractures have other associated injuries, including meniscal, collateral ligament, capsular, and osteochondral damage.
History and Physical
On history, young patients may present for evaluation after falling off a bicycle onto the involved knee. Initial symptoms include knee effusion, painful ambulation, difficulty bearing weight, and reduced knee range of motion.[9]
As with any fracture, emergencies must first be ruled out during physical examination. The skin should first be assessed for signs of an open fracture. A thorough neurologic and vascular examination should be performed to rule out compartment syndrome.
Hemarthrosis may not be evident in the presence of ligamentous injuries due to capsule disruption, allowing the effusion to escape the joint. The range of motion is usually limited due to pain.
Patients may have laxity on varus and valgus stress tests, indicating a lateral collateral (LCL) or medial collateral ligament (MCL) tear. Anterior and posterior drawer exams can be performed on the knee to assess ACL and PCL laxity. The Lachman test can help confirm an ACL disruption clinically.
A positive McMurray test indicates an accompanying meniscal tear. Tibial eminence fractures are associated with a high rate of meniscal entrapment.[10] Kocher et al reported that entrapment of the medial or lateral meniscus anterior horn or the intermeniscal ligament accompanies 26% of cases of type 2 tibial eminence fractures and 65% of type 3 tibial eminence injuries. About 3.8% of patients present with an associated meniscal tear.[11]
Evaluation
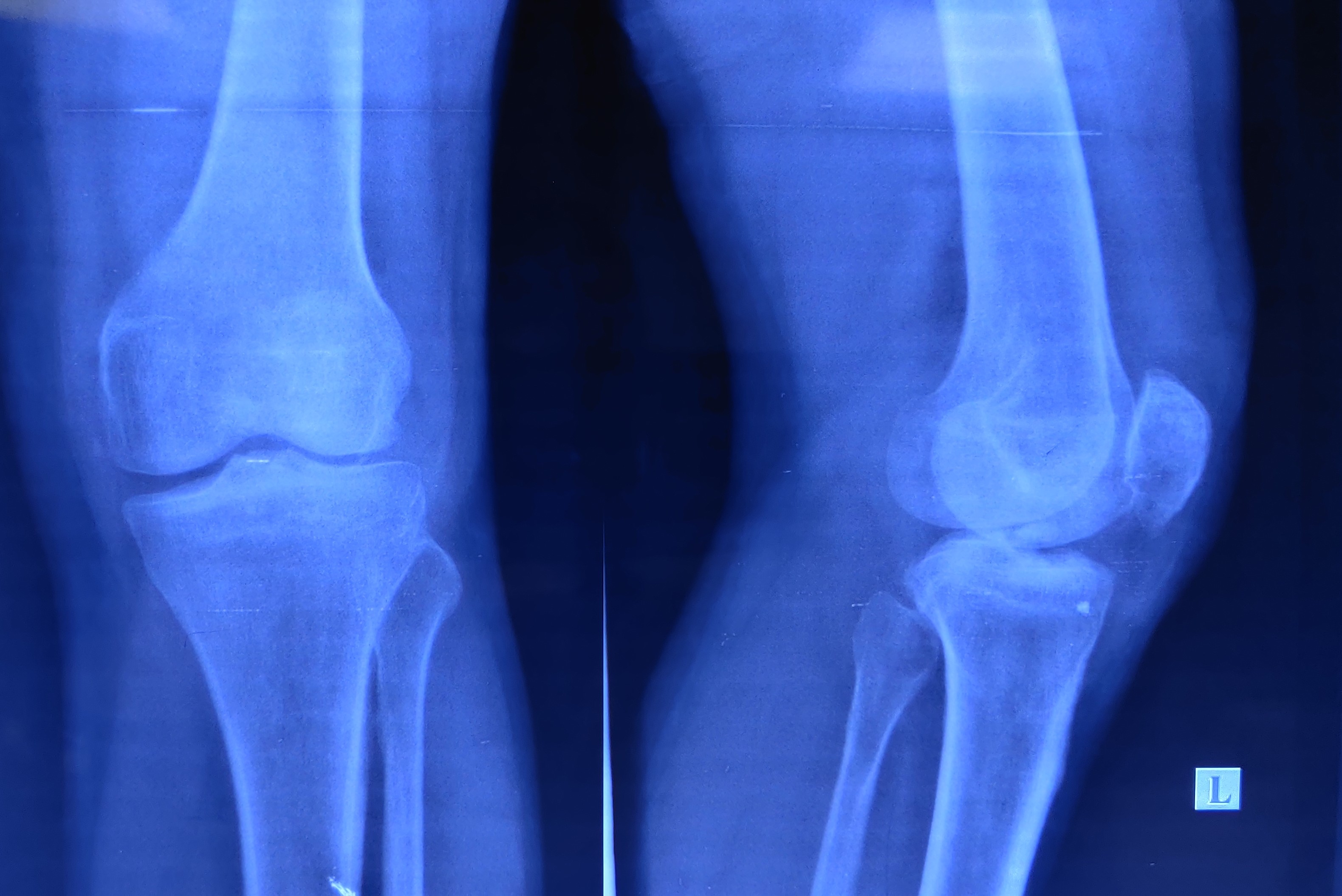
Anteroposterior and lateral (APL) knee x-rays may be obtained initially to assess for bony injury (see Image. Left Knee Tibial Eminence Fracture). Tibial eminence fractures should be visible on plain radiographs. Computed tomography (CT) and magnetic resonance imaging (MRI) may be necessary in cases where plain x-rays cannot ascertain fracture displacement and comminution or if knee ligament involvement cannot be ruled out.[12]
MRI allows detailed assessment for soft tissue damage or the presence of chondral fracture fragments if the tibial spines have not yet ossified (see Image. Tibial Eminence Fracture Magnetic Resonance Imaging). Studies by Kocher et al. and Mitchell et al. showed that types II and III tibial eminence fractures are associated with meniscal tears and entrapment.
Mitchell et al also reported that 7% of such injuries had associated chondral injuries. Additionally, about 48% of type III fractures had an associated meniscal entrapment, and 12% had meniscal tears.[13]
Treatment / Management
Tibial eminence fracture treatment aims to restore the ACL's continuity and stabilizing function, remove the bone fragments limiting the knee's mobility, and maintain the tibial plateau's articular congruity. Essential factors to consider during management planning include the fracture pattern and the presence of associated meniscal and chondral injuries, meniscal entrapment, and tibial plateau fractures.[14][15](B2)
Management Based On Fracture Type
For type I tibial eminence fractures, nonoperative management is considered first. The knee is immobilized in a position of comfort—at 20° of flexion or full extension—then placed in a cylinder cast. Maintenance in 20° flexion enables ACL fiber elongation.[16] Meanwhile, a fully extended position allows the lateral femoral condyle to maintain fracture alignment.[17]
Another report describes treating 14 type I fracture cases in the following sequence: hemarthrosis aspiration, closed reduction in hyperextension for 3 weeks, and cast re-application in 15° of flexion.[18] Hemarthrosis must be drained for symptomatic pain relief and ensure that reduction is complete. However, hyperextension may cause discomfort and pain and increase the risk of compartment syndrome. (B2)
The knee must be immobilized for 6 to 12 weeks or until radiographic union is achieved before transitioning to weight-bearing and range-of-motion exercises. Follow-up radiographs should be obtained right after closed reduction and then weekly or bimonthly until radiographic union is reached. The shortest possible immobilization period is recommended to prevent knee stiffness from long-term immobilization.
A retrospective review reported that a significant number of patients with type I tibial eminence fractures had concomitant injuries, with up to 25% requiring surgical intervention.[19](B2)
Nonoperative management may also be considered for Type II fractures. Fluoroscopy can confirm if closed reduction was performed successfully. Serial radiographs may be obtained on follow-up. However, Kocher et al found that around half of these injuries may have soft-tissue entrapment, rendering them unamenable to closed reduction.
Operative management should be pursued if closed reduction is not successful. Incomplete reduction can lead to difficulty fully extending the knee due to femoral notch impingement. Surgery should also be considered if the injury has an intraarticular extension.
The management options for complex type II tibial eminence fractures include open reduction and internal fixation (ORIF) and arthroscopic fracture fragment excision.
Types III and IV injuries have historically been managed by knee arthrotomy and ORIF. However, superior functional results have made arthroscopic reduction and internal fixation (ARIF) a better option than ORIF. Some combine arthroscopy with arthrotomy to characterize concomitant intraarticular soft tissue injuries before performing ORIF.
Arthroscopic fixation is usually accomplished by suturing or screw implantation after fracture hematoma debridement. Any interposed soft tissue is removed. The surgeon must be careful not to disrupt the tibial physis, which is incompletely developed in this population.
Surgical Fixation Techniques
The surgical options for tibial eminence fractures include open reduction and casting, ORIF, arthroscopic reduction and casting, and ARIF with sutures, screws, K-wires, or suture anchors. Of these, ARIF has become the modern standard of care (see Image. Tibial Eminence Arthroscopic Reduction and Internal Fixation)
Suturing for fracture fixation is technically challenging, although it dispenses the need for hardware removal after recovery. First, the tibial tunnel at the ACL footprint is made. Next, the ACL insertion site is repaired, which may be accomplished using various techniques and suture types. Absorbable sutures are preferred due to potential physis tethering with permanent sutures. Metallic sutures may also be used but must be removed once follow-up x-rays show healing.
After stitching through the ACL, the suture's ends are pulled through the tibial tunnel. The knee is then extended while tension is applied to the sutures to reduce the fragment. The suture is then tied over the bony bridge.
Some surgeons use a bone-tendon-bone fixation device to hold the fragments in place before tensioning.[20] This technique should be considered for comminuted fractures or fractures too small for screw fixation since sutures can fit the ACL and small bone fragments. Additionally, the procedure avoids placing hardware across the physis.[21] An economical three-point, all-inside, all-epiphyseal suture fixation technique using nonabsorbable polyester sutures to repair tibial eminence fractures securely was recently described.[22]
Screw fixation is accomplished in anterograde or retrograde fashion. In anterograde fixation, the knee flexed at 90° after reducing the fracture. The guidewire is then inserted superoanterior to inferoposterior using the anteromedial portal. A cannulated screw is then inserted to fixate the fracture.
In retrograde fixation, the guidewire is inserted through the anterior tibial cortex and directed toward the tibial eminence. The cannulated screw is then placed over the guidewire before fixating the fracture. Retrograde fixation is considered less invasive. However, the fragment must be greater than 15 mm for optimal fixation.
Suture fixation is increasingly becoming more widely used for managing tibial eminence fractures due to the reduced risk of hardware irritation and less need for operative screw removal. Superficially placed screws can damage the articular cartilage. Screw fixation also risks tibial physis growth disturbance, and the size requirement limits its application.
Generally, screw implantation results in a more rigid fixation than suturing. However, good suture fixation may also be achieved using the right suture type. A prospective randomized study found that arthroscopic pull-through suture anchoring was superior to screw fixation, as it provided better clinical and functional results with less re-surgery risk in skeletally mature patients.[23](B2)
Differential Diagnosis
The differential diagnosis of tibial eminence fractures includes the following conditions:
- ACL tear
- Meniscal tear
- LCL or MCL sprain
- Patellar fracture
- Osteochondral fragment
- Femoral condyle fracture
- Tibial plateau fracture
These conditions can be ruled out by obtaining a complete medical evaluation.
Staging
Meyers and McKeever published their classification of tibial eminence fractures in 1959 based on imaging reviews, though this system was modified years later. The modified version is as follows:
- Type I - Non-displaced fracture, with bony apposition
- Type II - Partially anteriorly displaced fracture with the posterior cortex acting as a hinge
- Type III - Completely displaced; type III-A is not rotated, while type III-B is rotated
- Type IV - Comminuted
Classification of these fractures is essential to management.
Prognosis
Without surgical intervention, displaced tibial eminence fractures have a high incidence of knee instability. Pailhe et al reported that patients treated surgically have better functional outcomes than those who did not receive operative treatment. Individuals who undergo surgical reduction and internal fixation generally have good results, with an average Lysholm score of 84.6, and about 81% of patients were satisfied with the results. Patients were able to return to sporting activities in 20 weeks.
The same group also compared ARIF to ORIF and reported no difference in patient outcomes. Individuals treated with screw fixation had comparable results to those treated with suture fixation.[24]
Complications
The potential complications of tibial eminence fractures include the following:
- Loss of motion
- Malunion
- Disuse quadriceps atrophy
- Nonunion
- Physeal disruption or growth disturbance, manifesting as recurvatum deformity, distal femoral valgus deformity, or limb length discrepancy
- Laxity
- Hardware irritation or impingement, most commonly with metal suture and screw fixation
- Mechanical impingement
- Postsurgical arthrofibrosis
- Chondral injury
- Interposed soft tissue
Watts et al found that the incidence of postsurgical arthrofibrosis does not differ significantly from one procedure to another. However, patients who underwent arthroscopic fixation had more risk factors for arthrofibrosis, particularly time to pediatric orthopedic surgery referral and duration of surgery. The same group reported that time to surgery greater than 7 days from injury and operative time exceeding 120 minutes increase arthrofibrosis risk.
Interposed soft tissue within the fracture site can prevent fracture reduction and may lead to malunion. The soft tissues that can impede proper healing include the transverse intermeniscal ligament and anterior horn of the medial or lateral meniscus.[25]
Postoperative and Rehabilitation Care
Nondisplaced fractures should be immobilized for 6 weeks or until evidence of radiographic union is obtained. Isometric closed-chain hamstring and quadricep exercises should be introduced early in rehabilitation to prevent atrophy.
For postoperative rehabilitation, the knee should be immobilized in extension for 2 weeks before gradually initiating range-of-motion exercises. Partial weight-bearing is allowed at 2 weeks with crutches. Quadriceps exercises should be initiated anytime after surgery to avoid postoperative atrophy. Postoperative protocols must be personalized.
Deterrence and Patient Education
Preventing tibial eminence fractures on the primary level involves the following:
- Strength and conditioning between sports events
- Using protective gear when engaging in physical activity
- Allowing ample rest and recovery between activities
- Avoiding overexertion
- Regular medical screening to assess potential injury risk factors
- Balanced nutrition to enhance bone, ligament, and muscle strength
- Following sports safety measures
- Using the proper sports technique
Secondary preventive measures for these injuries include the following:
- Educating patients and their families on the importance of postoperative rehabilitation
- Emphasizing adherence to treatment and follow-up schedules [26]
These measures cannot always prevent tibial eminence fractures and recurrences, though they can significantly reduce injury risk.
Enhancing Healthcare Team Outcomes
Managing tibial eminence fractures should involve collaboration among various healthcare professionals. The interprofessional team members should include the following:
- A primary care pediatrician or emergency physician provides initial evaluation and supportive treatment and sends a referral to the orthopedic surgeon.
- A radiologist evaluates imaging results and aids in management planning.
- An orthopedic surgeon determines the appropriate treatment plan, whether surgical or nonsurgical, for individuals with tibial eminence fractures.
- An anesthesiologist administers anesthesia, ensures patient comfort, and monitors patient status during surgery if required.
- A physical therapist designs exercise programs to improve knee strength, flexibility, and functional recovery after surgery or conservative management. These providers also educate patients on proper exercise and movement techniques to prevent further injury.
- Nursing staff provides health education, monitors the patient's progress, assists with postoperative care, and coordinates appointments and follow-ups.
- A sports medicine specialist provides specialized care to athletes in recovery to allow safe return to sports and prevent injury recurrence.
- An occupational therapist helps patients recover functionality and autonomy in performing daily tasks.
Communication and coordination within the interprofessional team are critical for providing optimal care and facilitating a smooth recovery for individuals with tibial eminence fractures.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
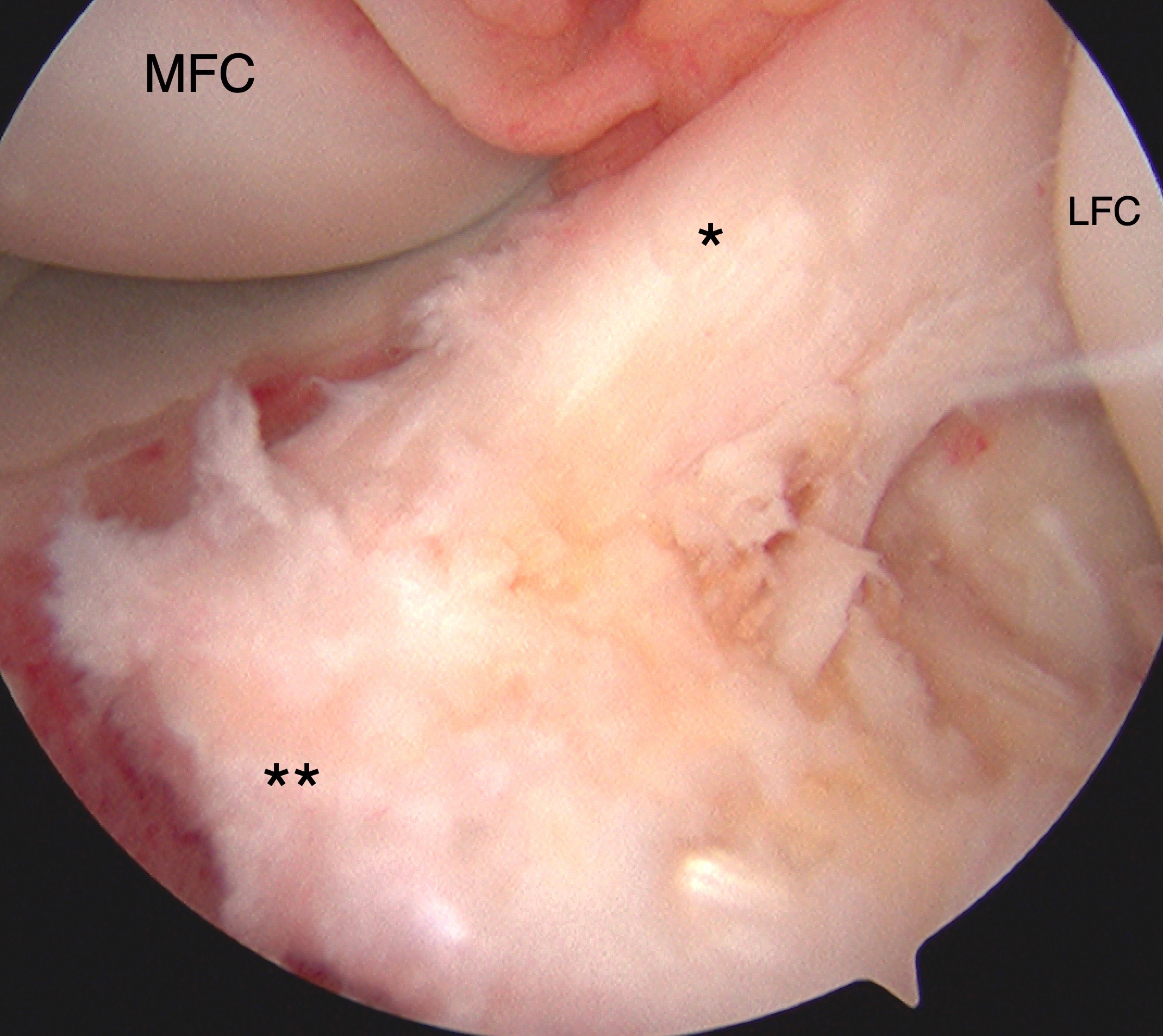
Tibial Eminence Arthroscopic Reduction and Internal Fixation. Tibial eminence avulsion injury confirmed by direct visualization during knee arthroscopy. Arthroscopy-assisted internal fixation was performed using sutures for anchoring. The anterior cruciate ligament (ACL, marked by *) and insertional footprint on the tibia (marked by **) are shown. The medial (MFC) and lateral (LFC) femoral condyles are also labeled for reference.
Contributed by Matthew A Varacallo MD
References
Lafrance RM, Giordano B, Goldblatt J, Voloshin I, Maloney M. Pediatric tibial eminence fractures: evaluation and management. The Journal of the American Academy of Orthopaedic Surgeons. 2010 Jul:18(7):395-405 [PubMed PMID: 20595132]
Anderson CN, Anderson AF. Tibial eminence fractures. Clinics in sports medicine. 2011 Oct:30(4):727-42. doi: 10.1016/j.csm.2011.06.007. Epub 2011 Sep 13 [PubMed PMID: 22018313]
Coyle C, Jagernauth S, Ramachandran M. Tibial eminence fractures in the paediatric population: a systematic review. Journal of children's orthopaedics. 2014 Mar:8(2):149-59. doi: 10.1007/s11832-014-0571-6. Epub 2014 Mar 2 [PubMed PMID: 24585047]
Level 1 (high-level) evidenceShin YW, Uppstrom TJ, Haskel JD, Green DW. The tibial eminence fracture in skeletally immature patients. Current opinion in pediatrics. 2015 Feb:27(1):50-7. doi: 10.1097/MOP.0000000000000176. Epub [PubMed PMID: 25502896]
Level 3 (low-level) evidenceSkak SV. A case of partial physeal closure following compression injury. Archives of orthopaedic and trauma surgery. 1989:108(3):185-8 [PubMed PMID: 2730302]
Level 3 (low-level) evidenceMessner MK, McGee AS, Elphingstone JW, Schartung DF, Frazier MB, Schick S, Brabston EW, Momaya AM. The Relationship Between Posterior Tibial Slope and Pediatric Tibial Eminence Fractures. The American journal of sports medicine. 2023 Jan:51(1):32-37. doi: 10.1177/03635465221137888. Epub 2022 Dec 1 [PubMed PMID: 36453727]
Luhmann SJ. Acute traumatic knee effusions in children and adolescents. Journal of pediatric orthopedics. 2003 Mar-Apr:23(2):199-202 [PubMed PMID: 12604951]
Eiskjaer S, Larsen ST, Schmidt MB. The significance of hemarthrosis of the knee in children. Archives of orthopaedic and traumatic surgery. Archiv fur orthopadische und Unfall-Chirurgie. 1988:107(2):96-8 [PubMed PMID: 3358674]
Perugia D, Basiglini L, Vadalà A, Ferretti A. Clinical and radiological results of arthroscopically treated tibial spine fractures in childhood. International orthopaedics. 2009 Feb:33(1):243-8. doi: 10.1007/s00264-008-0697-6. Epub 2008 Nov 29 [PubMed PMID: 19043709]
Level 2 (mid-level) evidenceOostvogel HJ, Klasen HJ, Reddingius RE. Fractures of the intercondylar eminence in children and adolescents. Archives of orthopaedic and traumatic surgery. Archiv fur orthopadische und Unfall-Chirurgie. 1988:107(4):242-7 [PubMed PMID: 3408321]
Kocher MS, Micheli LJ, Gerbino P, Hresko MT. Tibial eminence fractures in children: prevalence of meniscal entrapment. The American journal of sports medicine. 2003 May-Jun:31(3):404-7 [PubMed PMID: 12750134]
Gans I, Baldwin KD, Ganley TJ. Treatment and Management Outcomes of Tibial Eminence Fractures in Pediatric Patients: A Systematic Review. The American journal of sports medicine. 2014 Jul:42(7):1743-50. doi: 10.1177/0363546513508538. Epub 2013 Nov 20 [PubMed PMID: 24256714]
Level 1 (high-level) evidenceMitchell JJ, Sjostrom R, Mansour AA, Irion B, Hotchkiss M, Terhune EB, Carry P, Stewart JR, Vidal AF, Rhodes JT. Incidence of meniscal injury and chondral pathology in anterior tibial spine fractures of children. Journal of pediatric orthopedics. 2015 Mar:35(2):130-5. doi: 10.1097/BPO.0000000000000249. Epub [PubMed PMID: 24992346]
Level 2 (mid-level) evidenceHunter RE, Willis JA. Arthroscopic fixation of avulsion fractures of the tibial eminence: technique and outcome. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2004 Feb:20(2):113-21 [PubMed PMID: 14760342]
Level 2 (mid-level) evidenceSeon JK, Park SJ, Lee KB, Gadikota HR, Kozanek M, Oh LS, Hariri S, Song EK. A clinical comparison of screw and suture fixation of anterior cruciate ligament tibial avulsion fractures. The American journal of sports medicine. 2009 Dec:37(12):2334-9. doi: 10.1177/0363546509341031. Epub 2009 Sep 8 [PubMed PMID: 19737989]
Level 2 (mid-level) evidenceBeynnon BD, Johnson RJ, Fleming BC, Stankewich CJ, Renström PA, Nichols CE. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension. A comparison of an open and a closed kinetic chain exercise. The American journal of sports medicine. 1997 Nov-Dec:25(6):823-9 [PubMed PMID: 9397272]
Hallam PJ, Fazal MA, Ashwood N, Ware HE, Glasgow MM, Powell JM. An alternative to fixation of displaced fractures of the anterior intercondylar eminence in children. The Journal of bone and joint surgery. British volume. 2002 May:84(4):579-82 [PubMed PMID: 12043782]
Wilfinger C, Castellani C, Raith J, Pilhatsch A, Höllwarth ME, Weinberg AM. Nonoperative treatment of tibial spine fractures in children-38 patients with a minimum follow-up of 1 year. Journal of orthopaedic trauma. 2009 Aug:23(7):519-24. doi: 10.1097/BOT.0b013e3181a13fe4. Epub [PubMed PMID: 19633462]
Level 2 (mid-level) evidenceShimberg JL, Leska TM, Cruz AI Jr, Ellis HB Jr, Patel NM, Yen YM, Tibial Spine Research Interest Group, Schmale GA, Mistovich RJ, Fabricant PD, Ganley TJ, Green DW, Johnson B, Kushare I, Lee RJ, McKay SD, Milbrandt TA, Rhodes J, Sachleben B, Traver JL. Is Nonoperative Treatment Appropriate for All Patients With Type 1 Tibial Spine Fractures? A Multicenter Study of the Tibial Spine Research Interest Group. Orthopaedic journal of sports medicine. 2022 Jun:10(6):23259671221099572. doi: 10.1177/23259671221099572. Epub 2022 Jun 3 [PubMed PMID: 35677019]
Level 2 (mid-level) evidenceKobayashi S, Harato K, Udagawa K, Masumoto K, Jinnouchi M, Toyoda T, Niki Y. Arthroscopic Treatment of Tibial Eminence Avulsion Fracture With Suture Tensioning Technique. Arthroscopy techniques. 2018 Mar:7(3):e251-e256. doi: 10.1016/j.eats.2017.08.078. Epub 2018 Feb 19 [PubMed PMID: 29881697]
Zhao C, Bi Q, Bi M. Management of a type two avulsion fracture of the tibial intercondylar eminence in children: arthroscopic suture fixation versus conservative immobilization. International orthopaedics. 2018 Jun:42(6):1363-1369. doi: 10.1007/s00264-018-3855-5. Epub 2018 Mar 7 [PubMed PMID: 29516235]
Yuan L, Shi R, Chen Z, Ding W, Tan H. The most economical arthroscopic suture fixation for tibial intercondylar eminence avulsion fracture without any implant. Journal of orthopaedic surgery and research. 2022 Jun 25:17(1):327. doi: 10.1186/s13018-022-03219-w. Epub 2022 Jun 25 [PubMed PMID: 35752828]
Jain S, Modi P, Dayma RL, Mishra S. Clinical outcome of arthroscopic suture versus screw fixation in tibial avulsion of the anterior cruciate ligament in skeletally mature patients. Journal of orthopaedics. 2023 Jan:35():7-12. doi: 10.1016/j.jor.2022.10.006. Epub 2022 Oct 20 [PubMed PMID: 36325248]
Level 2 (mid-level) evidencePailhé R, Bauer T, Flecher X, Bonnevialle N, Roussignol X, Saragaglia D, Ehlinger M, SOFCOT. Better functional outcomes for ORIF in tibial eminence fracture treatment: a national comparative multicentric study of ORIF vs ARIF. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2020 Feb:28(2):653-657. doi: 10.1007/s00167-019-05785-9. Epub 2019 Dec 3 [PubMed PMID: 31797020]
Level 2 (mid-level) evidenceWatts CD, Larson AN, Milbrandt TA. Open Versus Arthroscopic Reduction for Tibial Eminence Fracture Fixation in Children. Journal of pediatric orthopedics. 2016 Jul-Aug:36(5):437-9. doi: 10.1097/BPO.0000000000000476. Epub [PubMed PMID: 25887823]
Gilmer BB. Editorial Commentary: Anterior Cruciate Ligament Tibial Eminence Avulsion Fractures: Are They Trying to Tell Us Something? Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2019 May:35(5):1545-1546. doi: 10.1016/j.arthro.2019.02.007. Epub [PubMed PMID: 31054729]
Level 3 (low-level) evidence