Introduction
Intravascular ultrasound (IVUS) is an intravascular imaging modality primarily used in interventional cardiology to characterize lesion morphology, quantify plaque burden, guide stent sizing, assess stent expansion, and identify procedural complications.[1] Using a dedicated catheter with ultrasound-based technology an image is obtainable from inside an artery producing cross-sectional images with a 360-degree view of the vessel. This technology overcomes many of the limitations of angiography, which utilizes x-ray technology to produce a 2-dimensional lumenogram of a 3-dimensional structure. Rather than assessing the vessel from the outside as with angiography, IVUS provides the assessment from within the vessel.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
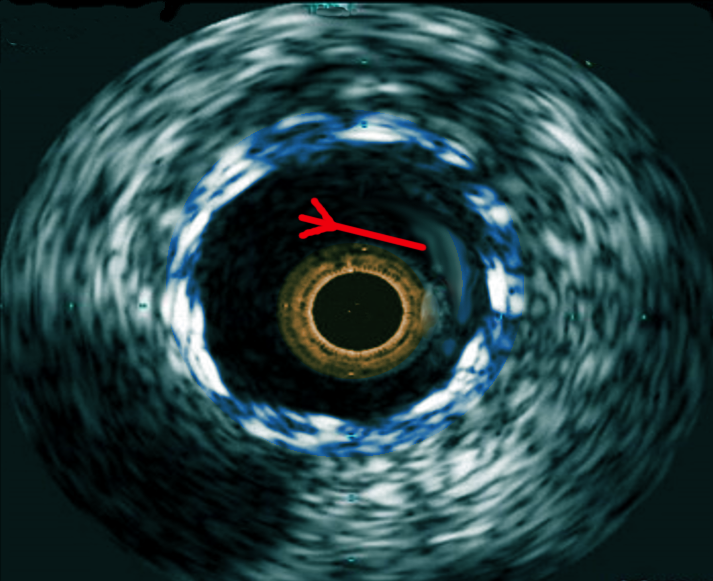
Intravascular ultrasound of a coronary artery allows for identification and delineation of the lumen and the 3 layers of the arterial wall: the inner tunica intima, the muscular tunica media, and the outer tunica adventitia. The smooth muscle cells comprising the tunica media does not reflect ultrasound waves and appears dark in the gray-scale cross-sectional image, permitting easy identification. Intravascular imaging with IVUS characterizes and quantifies plaque. IVUS assessment can distinguish between calcified plaque, lipid, and neointimal proliferation. IVUS allows for the identification of calcified plaque that may be undetectable from angiography alone.[2] For evaluation of stent failure with stent thrombosis or in-stent restenosis, IVUS plays a critical role to identify the mechanism of stent failure, guiding appropriate therapy.
Indications
IVUS has indications for a wide range of uses in patients undergoing cardiac catheterization and percutaneous coronary interventions (PCI).
The following are the recommendations made regarding the use of IVUS for PCI, according to guidelines from the American College of Cardiology (ACC).[3]
CLASS IIa:
- IVUS is a reasonable option to assess angiographically indeterminant left main CAD (Level of Evidence: B)
- IVUS and coronary angiography are within reason 4 to 6 weeks and 1-year post cardiac transplantation to rule out donor CAD, detect rapidly progressive cardiac allograft vasculopathy, and provide prognostic information (Level of Evidence: B)
- IVUS is a reasonable option to determine the mechanism of stent restenosis (Level of Evidence: C)
CLASS IIb:
- IVUS may be reasonable in assessing non–left main coronary arteries possessing angiographically intermediate coronary stenoses (i.e., 50% to 70% diameter stenosis) (Level of Evidence: B)
- IVUS may be considered for the guidance of coronary stent implantation, especially in cases of left main coronary artery (LMCA) stenting (Level of Evidence: B)
- IVUS may be reasonable for the determination of the mechanism of stent thrombosis (Level of Evidence: C)
CLASS III:
- IVUS for routine lesion assessment is not a recommendation if revascularization with PCI or CABG is not being contemplated (Level of Evidence: C)
European Guidelines have been updated more recently, and the 2018 guidelines from the European Society of Cardiology (ESC) recommends IVUS to assess the severity and optimize the treatment of unprotected left main coronary lesions (Class IIa, level of evidence B).[4] Additionally, the ESC recommends that IVUS should be considered to detect stent related mechanical problems leading to restenosis (Class IIa, level of evidence C) and IVUS should be considered in selected patients to optimize stent implantation (Class IIa, level of evidence B).
Contraindications
While no true absolute contraindications for IVUS exist, extreme vessel tortuosity and angulation that would preclude the ability to deliver an IVUS catheter to the area of interest is a relative contraindication. As with any instrumentation of the coronary arteries, IVUS use is accompanied by systemic anticoagulation during the procedure. Consequently, an indirect IVUS contraindication would be a patient who is not a suitable candidate for systemic anticoagulation or a patient who is not a candidate for angiography and cardiac catheterization in general.
Equipment
IVUS obtains images from a piezoelectric transducer that produces sound waves. IVUS catheters divide into two main categories based on the mechanism of transducer design. IVUS catheters currently in use are either solid-state phased array incorporating multiple stationary piezoelectric transducers or consist of a rotational design based on a single piezoelectric transducer.[5] Solid-state phased array IVUS catheters have the advantage of a broad depth of field and are often the preferred imaging modality in larger vessels such as for peripheral interventions. Rotational IVUS offers the advantage of an automated pullback allowing for measurements in determining lesion length and stent length selection.
Multimodality IVUS catheters, combining IVUS and an additional intravascular technology are now commercially available with combined IVUS and near-infrared spectroscopy (NIRS) and under investigation for future use with IVUS and optical coherence tomography (OCT).
Personnel
IVUS catheters transmit an image to a dedicated console for image analysis. Ancillary catheterization laboratory staff can prepare the IVUS catheter. An interventional cardiologist or vascular surgeon manipulates the catheter inside of the body. Online assessment can be performed to characterize plaque morphology and assess minimal lumen area (MLA), determine plaque burden, and identify segments of normal artery.
Preparation
The preparation of IVUS imaging catheters varies slightly with each manufacturer but is mostly a straightforward process that consists of flushing the catheter system with saline and connecting the catheter to a console. Systemic anticoagulation and intracoronary nitroglycerin should be administered before the insertion of IVUS to minimize and prevent the risk of thrombus and vasospasm.
Technique or Treatment
Performance of IVUS assessment of a vessel can be with either a manual or automatic pullback. Automated pullback allows for length measurements by producing a longitudinal profile, which is useful for the determination of the appropriate stent length that should be selected. Stent diameter selection the identification of and then measuring the proximal and distal references. Following stent implantation, IVUS can assess the minimal stent area (MSA), a prognostic indicator closely associated with the likelihood of future events related to the stent.[6]
Complications
Complications due to IVUS use are uncommon but may include dissection, perforation, arrhythmia, thrombosis, and vasospasm as can occur during any instrumentation of a coronary vessel.[7] Particular care is necessary for highly tortuous vessels.
Clinical Significance
For assessment of left main coronary arteries, IVUS can be used to determine lesion significance and guide revascularization. The use of IVUS often leads to a change in the PCI strategy.[8] Clinical data from multicenter randomized trials and meta-analyses have consistently demonstrated that the use of IVUS can lead to a reduction in adverse clinical events.[9][10][11][12] IVUS assessment following PCI can determine predictors for restenosis based on post-intervention cross-sectional area.[13] Despite several decades of data supporting the use and benefits of IVUS, utilization remains low in the United States.[14]
Enhancing Healthcare Team Outcomes
IVUS is an important adjunctive tool in the cardiac catheterization laboratory that can be useful to determine plaque morphology and guide percutaneous coronary interventions. Image interpretation is an important skill with IVUS use to optimize clinical outcomes. The use of IVUS has been associated with improved clinical outcomes in both an all-comers population and those with long lesions undergoing stent implantation (28 mm stent implanted).[9][10][Level I]
To provide the best outcome, interprofessional team involvement is necessary. The nurse needs to be well aware of the procedure and complications and assist the interventional cardiologist or vascular surgeon as they manipulate the catheter inside of the body. Prior to the procedure, the nurse should assist with pre-operative screen for allergies or injuries that may hinder the performance of the procedure. If there is a concern, the should report back to the clinician. Often the nurse will need to assist with position and preparation of the patient. The nurse should also monitor vital signs and the ECG during the procedure and should alert the surgeon if there are changes in vitals signs or an untoward change in the cardiac monitor. Always quickly reporting to the surgeon if there is a concern. Post-procedure the nurse must monitor for signs of bleeding or infection. Again, quickly informing the surgeon if there is a concern. The best outcomes will be achieved if an interprofessional approach is taken in regards to the performance of this procedure. [Level V] [15]
Media
References
Parviz Y,Shlofmitz E,Fall KN,Konigstein M,Maehara A,Jeremias A,Shlofmitz RA,Mintz GS,Ali ZA, Utility of intracoronary imaging in the cardiac catheterization laboratory: comprehensive evaluation with intravascular ultrasound and optical coherence tomography. British medical bulletin. 2018 Mar 1; [PubMed PMID: 29360941]
Mintz GS,Popma JJ,Pichard AD,Kent KM,Satler LF,Chuang YC,Ditrano CJ,Leon MB, Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation. 1995 Apr 1; [PubMed PMID: 7895353]
Levine GN,Bates ER,Blankenship JC,Bailey SR,Bittl JA,Cercek B,Chambers CE,Ellis SG,Guyton RA,Hollenberg SM,Khot UN,Lange RA,Mauri L,Mehran R,Moussa ID,Mukherjee D,Nallamothu BK,Ting HH, 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 22065485]
Level 1 (high-level) evidenceNeumann FJ,Sousa-Uva M,Ahlsson A,Alfonso F,Banning AP,Benedetto U,Byrne RA,Collet JP,Falk V,Head SJ,Jüni P,Kastrati A,Koller A,Kristensen SD,Niebauer J,Richter DJ,Seferovic PM,Sibbing D,Stefanini GG,Windecker S,Yadav R,Zembala MO, 2018 ESC/EACTS Guidelines on myocardial revascularization. European heart journal. 2018 Aug 25; [PubMed PMID: 30165437]
Garcìa-Garcìa HM,Gogas BD,Serruys PW,Bruining N, IVUS-based imaging modalities for tissue characterization: similarities and differences. The international journal of cardiovascular imaging. 2011 Feb; [PubMed PMID: 21327914]
Song HG,Kang SJ,Ahn JM,Kim WJ,Lee JY,Park DW,Lee SW,Kim YH,Lee CW,Park SW,Park SJ, Intravascular ultrasound assessment of optimal stent area to prevent in-stent restenosis after zotarolimus-, everolimus-, and sirolimus-eluting stent implantation. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 22815193]
Hausmann D,Erbel R,Alibelli-Chemarin MJ,Boksch W,Caracciolo E,Cohn JM,Culp SC,Daniel WG,De Scheerder I,DiMario C, The safety of intracoronary ultrasound. A multicenter survey of 2207 examinations. Circulation. 1995 Feb 1; [PubMed PMID: 7828285]
Level 2 (mid-level) evidenceWitzenbichler B,Maehara A,Weisz G,Neumann FJ,Rinaldi MJ,Metzger DC,Henry TD,Cox DA,Duffy PL,Brodie BR,Stuckey TD,Mazzaferri EL Jr,Xu K,Parise H,Mehran R,Mintz GS,Stone GW, Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014 Jan 28; [PubMed PMID: 24281330]
Level 2 (mid-level) evidenceZhang J,Gao X,Kan J,Ge Z,Han L,Lu S,Tian N,Lin S,Lu Q,Wu X,Li Q,Liu Z,Chen Y,Qian X,Wang J,Chai D,Chen C,Li X,Gogas BD,Pan T,Shan S,Ye F,Chen SL, Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation: The ULTIMATE Trial. Journal of the American College of Cardiology. 2018 Dec 18; [PubMed PMID: 30261237]
Level 2 (mid-level) evidenceHong SJ,Kim BK,Shin DH,Nam CM,Kim JS,Ko YG,Choi D,Kang TS,Kang WC,Her AY,Kim YH,Hur SH,Hong BK,Kwon H,Jang Y,Hong MK, Effect of Intravascular Ultrasound-Guided vs Angiography-Guided Everolimus-Eluting Stent Implantation: The IVUS-XPL Randomized Clinical Trial. JAMA. 2015 Nov 24; [PubMed PMID: 26556051]
Level 1 (high-level) evidenceMintz GS, Intravascular ultrasound and outcomes after drug-eluting stent implantation. Coronary artery disease. 2017 Jun; [PubMed PMID: 28441172]
Steinvil A,Zhang YJ,Lee SY,Pang S,Waksman R,Chen SL,Garcia-Garcia HM, Intravascular ultrasound-guided drug-eluting stent implantation: An updated meta-analysis of randomized control trials and observational studies. International journal of cardiology. 2016 Aug 1; [PubMed PMID: 27153138]
Level 1 (high-level) evidenceMintz GS,Popma JJ,Pichard AD,Kent KM,Salter LF,Chuang YC,Griffin J,Leon MB, Intravascular ultrasound predictors of restenosis after percutaneous transcatheter coronary revascularization. Journal of the American College of Cardiology. 1996 Jun; [PubMed PMID: 8636553]
Smilowitz NR,Mohananey D,Razzouk L,Weisz G,Slater JN, Impact and trends of intravascular imaging in diagnostic coronary angiography and percutaneous coronary intervention in inpatients in the United States. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 30019831]
Malik AH,Yandrapalli S,Aronow WS,Panza JA,Cooper HA, Intravascular ultrasound-guided stent implantation reduces cardiovascular mortality - Updated meta-analysis of randomized controlled trials. International journal of cardiology. 2019 Jul 10 [PubMed PMID: 31345647]
Level 1 (high-level) evidence