Introduction
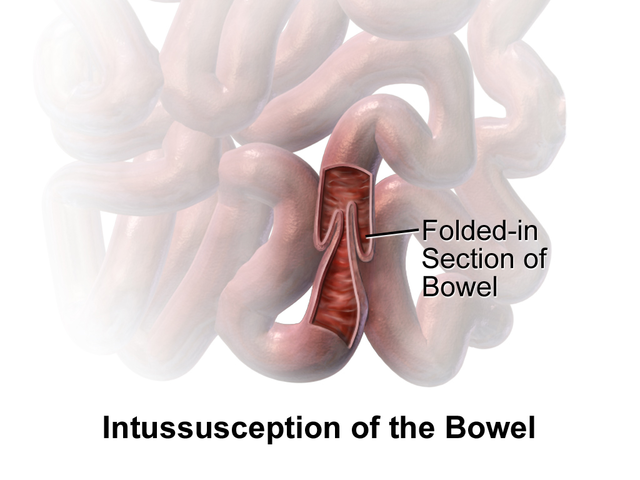
Intussusception is a condition in which part of the intestine folds into the section next to it. Intussusception usually involves the small bowel and rarely the large bowel. Symptoms include abdominal pain, which may wax and wane, vomiting, bloating, and bloody stool. It may result in small bowel obstruction. Other complications may include peritonitis or bowel perforation.[1][2][3][4]
The cause is typically unknown in children, while in adults, a lead point due to cancer is often present. Risk factors in children include infections, cystic fibrosis, and intestinal polyps. Risk factors in adults include endometriosis, bowel adhesions, and intestinal tumors. Medical imaging often supports a diagnosis. In children, ultrasound is a preferred method to diagnose, while in adults, a CT scan is preferred.[5]
Intussusception requires rapid treatment. Treatment in children is typically by an enema with surgery if not successful. In adults, removal of part of the bowel is more often required. Intussusception occurs more commonly in children than adults.[6]
Intussusception occurs more commonly in children than adults; in children, it is more common in males than females. The usual age of occurrence is six to 18 months old.[7]
The rate of intussusception significantly increases over the viral gastroenteritis seasons in some populations. Due to a statically significant increase of intussusception following some forms of rotavirus vaccine, (RRV-TV: Rotashield) form was removed from the market. History of upper respiratory tract infection, otitis media, and flu-like symptoms are present in one-third of the patients before the onset of intussusception. The adenoviral infection has been associated with an increased risk of intussusception. Moreover, in up to two out of five patients with intussusception, positive history of a recent viral enteric or non-enteric infection is present. In a solid population-based study, species C of the adenovirus was established as the strongest predictor of intussusception. However, in the same population, rotavirus infection and poliovirus vaccine were not associated with intussusception. Another study recognized an association with the human herpesvirus 6.[8]
A sub-type of intussusception, called pyloroduodenojejunal intussusception is one of the extremely rare variants of intussusception. Moreover, it is extremely rare in the pediatric population and is predicted in up to 10% of adult patients with intussusception. The underlying causality of pyloroduodenojejunal intussusception, includes pedunculated polyps, Menetrier disease, hamartomas, and gastrointestinal stromal tumors.[9]
Bacterial infections, especially bacterial enteritis, are also associated with intussusception. This association was documented for infection with Salmonella, Escherichia coli, Shigella, or Campylobacter. The intussusception is more common within the first month following the infection.[10][11][12]
Intussusception is not usually immediately life-threatening. It is usually successfully treated with barium, water-soluble, or an air-contrast enema, which both confirms the diagnosis and successfully reduces it. The success rate is more than 80%. However, up to 10% may reoccur within 24 hours.[13]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The causes of intussusception are not known. About 90% of cases of intussusception in children arise from an unknown cause. They can include infections, anatomical factors, and altered motility.[14][15][12]
Known causes may include:
- Infections
- Anatomical factors
- Altered motility
- Meckel's diverticulum
- Duplication
- Polyps
- Appendicitis
- Hyperplasia of Peyer patches
- Idiopathic[16]
An early version of the rotavirus vaccine that is no longer used was thought to cause intussusception, but the current vaccines are not clearly linked.[17]
Epidemiology
Intussusception is usually diagnosed in infancy and early childhood.
- Intussusception strikes about 2000 children in the United States in the first year of life.
- Intussusception is usually seen at five months of life, peaks at four to nine months, and then gradually declines at around 18 months.
- Intussusception occurs more frequently in boys than in girls, with a ratio of approximately 3:1.
- In adults, intussusception represents 1% of bowel obstructions and is associated with neoplasm.[18]
Pathophysiology
Usually, the ileum enters the cecum. Rarely does a part of the ileum or jejunum prolapse into itself. Almost all intussusceptions occur with the intussusceptum having been located proximally to the intussuscipiens. This is because a peristaltic action of the intestine pulls the proximal segment into the distal segment.
- The part that prolapses into the other is called the intussusceptum.
- The part that receives it is called the intussuscipiens.
- An anatomic lead point occurs in approximately 10% of intussusceptions.
The trapped section of the bowel may have its blood supply cut off, which causes ischemia. The mucosa is sensitive to ischemia and responds by causing sloughing off into the gut. This creates a "red currant jelly" stool, which sloughed mucosa, blood, and mucus. "Red currant jelly" occurs in a minority of cases of intussusception and should be considered in the differential diagnosis of children passing any bloody stool.[19]
History and Physical
Early symptoms include periodic abdominal pain, nausea, vomiting (green from bile), pulling legs to the chest, and cramping abdominal pain. Pain is intermittent because the bowel segment transiently stops contracting.
Later signs include rectal bleeding, often with "red currant jelly" stool, and lethargy. Physical examination may reveal a "sausage-shaped" mass. Children may cry, draw their knees up to their chest, or experience dyspnea with paroxysms of pain.
Fever is not a symptom of intussusception but a loop of bowel may become necrotic, secondary to ischemia, which leads to perforation and sepsis, which causes fever.
In rare cases, intussusception may be a complication of Henoch-Schönlein purpura. Such patients often present with severe abdominal pain in addition to the classic signs of Henoch-Schönlein purpura.[20]
Evaluation
Intussusception is often suspected based on an examination, including observation of the Dance sign (Dance sign consists of evaluating the right lower quadrant of the abdomen for retraction, which can be an indication of intussusception).
- A digital rectal examination is helpful, as a finger may feel the intussusceptum.
- A definite diagnosis requires confirmation by imaging modalities.
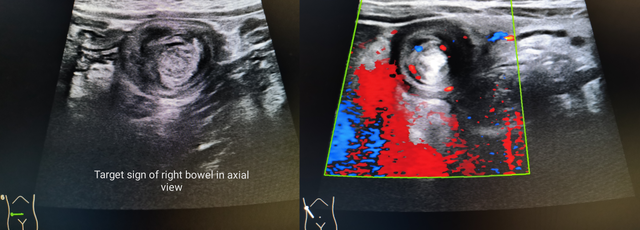
- Ultrasound is the test of choice for the diagnosis of intussusception. The appearance of the target or doughnut sign, usually around 3 cm in diameter, confirms the diagnosis.
- The image seen on transverse sonography or computed tomography is a doughnut shape, created by the hyperechoic central core of the bowel and mesentery surrounded by the hypoechoic outer edematous bowel.
- In longitudinal imaging, intussusception may resemble a sandwich.
An abdominal x-ray may be indicated to check for intestinal obstruction. An air enema may be used for diagnosis, and the same procedure can be used for treatment.
CT scan is sometimes used to make a diagnosis, especially when the Ultrasound imaging remains doubtful. However, in young children, obtaining a CT scan often requires the use of anesthesia and there is also the risk of intravenous contrast and radiation exposure.[21]
Treatment / Management
Intussusception is not usually immediately life-threatening. It is usually successfully treated with barium, water-soluble, or an air-contrast enema, which confirms the diagnosis and successfully reduces it. The success rate is more than 80%. However, up to 10% may reoccur within 24 hours.[22][23][24][25](B2)
Cases that cannot be reduced non-surgically require surgical reduction. In surgical reduction, the surgeon manually squeezes the part that has been telescoped. If the surgeon cannot successfully reduce it, the affected section is surgically removed. The intussusception may also be reduced by laparoscopy, pulling the segments of the intestine apart with forceps.[6](B3)
Differential Diagnosis
- Abdominal hernias
- Appendicitis
- Blunt abdominal trauma in emergency medicine
- Colic
- Cycling vomiting syndrome
- Emergent treatment of gastroenteritis
- Gastric volvulus
- Internal hernia
- Testicular torsion
- Volvulus[26]
Prognosis
Several agents, including glucagon and dexamethasone, have been examined to improve the success rate of enema reduction. Accordingly, the outcomes of adding dexamethasone were found to be promising. However, evidence suggesting the significant effect of adding glucagon in the success rate of enema reduction was lacking.[27]
Complications
Timely management of intussusception is critical to avoid complications, including perforation, bowel necrosis, and rarely short bowel syndrome. On the other hand, postoperative intussusception (POI) might occur as a rare complication following different surgeries. Some surgical procedures that might be complicated with post-operative intussusception include retroperitoneal tumor resection, Ladd procedure, diaphragmatic surgeries, and pancreatectomy. The risk of POI is up to 0.25 % in the pediatric population following laparotomy.[28]
Pearls and Other Issues
Intussusception is a medical emergency if not treated early and may result in death if not reduced. In developing countries, death is almost inevitable.
The prognosis for intussusception is excellent if treated quickly, but if untreated it can lead to death within two to five days. The longer the intestine segment is prolapsed and the longer it goes without a blood supply, the less effective a non-surgical reduction. Prolonged intussusception increases bowel ischemia and necrosis, requiring surgical resection.
The differential diagnosis of intussusception includes acute gastroenteritis and rectal prolapse.
- Abdominal pain, vomiting, and stool with blood and mucus occur in acute gastroenteritis, but diarrhea is the leading symptom.
- In rectal prolapse expect projecting mucosa that can be felt in continuity with the perianal skin, whereas in intussusception, the finger may pass indefinitely into the depth of the sulcus.
It is important to note that air contrast enema is not used to treat adults with intussusception; adults tend to have a lead point or an organic lesion that is often the cause of the problem.
Enhancing Healthcare Team Outcomes
Intussusception is a surgical emergency. The disorder is managed by an interprofessional team that consists of a radiologist, pediatrician, emergency department physician, and a pediadritic surgeon. The majority of cases are reduced non-surgically and have a good outcome. Cases not reduced by air or barium need surgery. Usuallly no bowel resection is required. Complications are rare after surgery and recurrences are very rare.[29] (Level V)
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
McRae JE, Quinn HE, Saravanos GL, McMinn A, Britton PN, Wood N, Marshall H, Macartney K. Paediatric Active Enhanced Disease Surveillance (PAEDS) annual report 2016: Prospective hospital-based surveillance for serious paediatric conditions. Communicable diseases intelligence (2018). 2019 Feb 1:43():. doi: 10.33321/cdi.2019.43.5. Epub 2019 Feb 1 [PubMed PMID: 30727704]
Jia Y, Fu H, Li N, Kang Q, Sheng J. [Diagnosis and treatment for 46 cases of Peutz-Jeghers syndrome]. Zhong nan da xue xue bao. Yi xue ban = Journal of Central South University. Medical sciences. 2018 Dec 28:43(12):1323-1327. doi: 10.11817/j.issn.1672-7347.2018.12.007. Epub [PubMed PMID: 30643048]
Level 3 (low-level) evidence. . :(): [PubMed PMID: 30506792]
Restivo V, Costantino C, Giorgianni G, Cuccia M, Tramuto F, Corsello G, Casuccio A, Vitale F. Case-control study on intestinal intussusception: implications for anti-rotavirus vaccination. Expert review of vaccines. 2018 Dec:17(12):1135-1141. doi: 10.1080/14760584.2018.1546122. Epub 2018 Nov 19 [PubMed PMID: 30407079]
Level 2 (mid-level) evidenceTeixeira H, Hauswirth F, Römer N, Muller MK, Baechtold M. An ileo-colic intussusception reaching down to the descending colon - A case report. International journal of surgery case reports. 2022 Apr:93():107009. doi: 10.1016/j.ijscr.2022.107009. Epub 2022 Apr 2 [PubMed PMID: 35381552]
Level 3 (low-level) evidencePatsikas MN, Papazoglou LG, Paraskevas GK. Current Views in the Diagnosis and Treatment of Intestinal Intussusception. Topics in companion animal medicine. 2019 Dec:37():100360. doi: 10.1016/j.tcam.2019.100360. Epub 2019 Sep 11 [PubMed PMID: 31837757]
Level 3 (low-level) evidenceZhang B, Wu D, Liu M, Bai J, Chen F, Zhang R, Fang Y. The diagnosis and treatment of retrograde intussusception: a single-centre experience. BMC surgery. 2021 Nov 13:21(1):398. doi: 10.1186/s12893-021-01391-0. Epub 2021 Nov 13 [PubMed PMID: 34774032]
Minney-Smith CA, Levy A, Hodge M, Jacoby P, Williams SH, Carcione D, Roczo-Farkas S, Kirkwood CD, Smith DW. Intussusception is associated with the detection of adenovirus C, enterovirus B and rotavirus in a rotavirus vaccinated population. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 2014 Dec:61(4):579-84. doi: 10.1016/j.jcv.2014.10.018. Epub 2014 Nov 4 [PubMed PMID: 25464971]
Level 2 (mid-level) evidenceBari H, Karkhanis S, Dasari BVM. Pyloroduodenojejunal Intussusception due to Hyperplastic Polyp of the Brunner Gland. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2021 Feb:25(2):565-566. doi: 10.1007/s11605-020-04662-y. Epub 2020 Jun 3 [PubMed PMID: 32495134]
Khalifa AB, Jebali A, Kedher M, Trabelsi A. [Infectious etiology of acute idiopathic intussusception in children]. Annales de biologie clinique. 2013 Jul-Aug:71(4):389-93. doi: 10.1684/abc.2013.0859. Epub [PubMed PMID: 23906565]
Pham T, La Paglia D, Pitcher M. Salmonella enteritis: A Rare Cause of Adult Intussusception. Annals of coloproctology. 2017 Oct:33(5):201-203. doi: 10.3393/ac.2017.33.5.201. Epub 2017 Oct 31 [PubMed PMID: 29159169]
Wu PW, Wang CC. Concurrent Campylobacter jejuni bacteremia and intussusception in an immunocompetent five-year-old child. Journal of microbiology, immunology, and infection = Wei mian yu gan ran za zhi. 2019 Apr:52(2):367-369. doi: 10.1016/j.jmii.2018.09.004. Epub 2018 Sep 24 [PubMed PMID: 30293925]
Shen G, Liu H, Guan Z, Shang X, Li J, Zhang C, Zhang J, Liu Y, Hu Q. Clinical features and factors leading to early recurrence of intussusception after saline reduction. JPMA. The Journal of the Pakistan Medical Association. 2020 Oct:70(10):1727-1730. doi: 10.5455/JPMA.21744. Epub [PubMed PMID: 33159742]
Bogdanović M, Blagojević M, Kuzmanović J, Ječmenica D, Alempijević Đ. Fatal intussusception in infancy: forensic implications. Forensic science, medicine, and pathology. 2019 Jun:15(2):284-287. doi: 10.1007/s12024-018-0039-y. Epub 2018 Nov 5 [PubMed PMID: 30397871]
Cha PI, Gurland B, Forrester JD. First Reported Case of Intussusception Caused by Escherichia coli O157:H7 in an Adult: Literature Review and Case Report. Surgical infections. 2019 Jan:20(1):95-99. doi: 10.1089/sur.2018.137. Epub 2018 Oct 25 [PubMed PMID: 30359547]
Level 3 (low-level) evidenceBodnár D, Kiss ÁL, Réti G. [Modern understanding of intussusception and recent trends in management]. Orvosi hetilap. 2020 Aug:161(32):1331-1338. doi: 10.1556/650.2020.31779. Epub [PubMed PMID: 32750021]
Level 3 (low-level) evidenceCho HK, Hwang SH, Nam HN, Han K, Kim B, Kong I, Park K, Lee J. Incidence of intussusception before and after the introduction of rotavirus vaccine in Korea. PloS one. 2020:15(8):e0238185. doi: 10.1371/journal.pone.0238185. Epub 2020 Aug 28 [PubMed PMID: 32857776]
Das MK, Arora NK, Mathai J, Sam CJ, G R, R K, K J, Arunachalam P, Gupta B. Profile and Epidemiology of Intussusception in Children Under-Two Years of Age: A Prospective Surveillance. Indian journal of pediatrics. 2021 Dec:88(12):1187-1194. doi: 10.1007/s12098-021-03776-8. Epub 2021 May 31 [PubMed PMID: 34057604]
Kim PH, Hwang J, Yoon HM, Lee JY, Jung AY, Lee JS, Cho YA. Predictors of failed enema reduction in children with intussusception: a systematic review and meta-analysis. European radiology. 2021 Nov:31(11):8081-8097. doi: 10.1007/s00330-021-07935-5. Epub 2021 May 11 [PubMed PMID: 33974147]
Level 1 (high-level) evidenceCoca Robinot D, Liébana de Rojas C, Aguirre Pascual E. Abdominal emergencies in pediatrics. Radiologia. 2016 May:58 Suppl 2():80-91. doi: 10.1016/j.rx.2016.02.003. Epub 2016 Mar 31 [PubMed PMID: 27041066]
Peyvasteh M, Askarpour S, Javaherizadeh H, Beigom Al-Taha B. Intussuception at atypical ages in children and adults--11 years experiences. Polski przeglad chirurgiczny. 2011 Jun:83(6):304-9. doi: 10.2478/v10035-011-0047-z. Epub [PubMed PMID: 22166546]
Level 2 (mid-level) evidenceZhang Y, Zou W, Zhang Y, Ye W, Chen X, Liu Q, Liu H, Si C, Jia H. Reducing Antibiotic Use for Young Children with Intussusception following Successful Air Enema Reduction. PloS one. 2015:10(11):e0142999. doi: 10.1371/journal.pone.0142999. Epub 2015 Nov 16 [PubMed PMID: 26569111]
Sáez-Llorens X, Velázquez FR, Lopez P, Espinoza F, Linhares AC, Abate H, Nuñez E, Venegas G, Vergara R, Jimenez AL, Rivera M, Aranza C, Richardson V, Macias-Parra M, Palacios GR, Rivera L, Ortega-Barria E, Cervantes Y, Rüttimann R, Rubio P, Acosta CJ, Newbern C, Verstraeten T, Breuer T. A multi-country study of intussusception in children under 2 years of age in Latin America: analysis of prospective surveillance data. BMC gastroenterology. 2013 May 27:13():95. doi: 10.1186/1471-230X-13-95. Epub 2013 May 27 [PubMed PMID: 23710610]
Level 2 (mid-level) evidenceDavidson A. Anesthetic management of common pediatric emergencies. Current opinion in anaesthesiology. 2013 Jun:26(3):304-9. doi: 10.1097/ACO.0b013e328360ea40. Epub [PubMed PMID: 23563798]
Level 3 (low-level) evidenceRice-Townsend S, Chen C, Barnes JN, Rangel SJ. Variation in practice patterns and resource utilization surrounding management of intussusception at freestanding Children's Hospitals. Journal of pediatric surgery. 2013 Jan:48(1):104-10. doi: 10.1016/j.jpedsurg.2012.10.025. Epub [PubMed PMID: 23331801]
Level 2 (mid-level) evidenceGrama F, Onica M, Chitul A, Bezede C, Burcoș T, Cristian D. Appendix intussusception: a challenging differential diagnosis. ANZ journal of surgery. 2020 Oct:90(10):2090-2091. doi: 10.1111/ans.15727. Epub 2020 Jan 25 [PubMed PMID: 31981391]
Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. The Cochrane database of systematic reviews. 2017 Jun 1:6(6):CD006476. doi: 10.1002/14651858.CD006476.pub3. Epub 2017 Jun 1 [PubMed PMID: 28567798]
Level 1 (high-level) evidenceYang G, Wang X, Jiang W, Ma J, Zhao J, Liu W. Postoperative intussusceptions in children and infants: a systematic review. Pediatric surgery international. 2013 Dec:29(12):1273-9. doi: 10.1007/s00383-013-3345-1. Epub 2013 Jul 13 [PubMed PMID: 23852556]
Level 1 (high-level) evidenceXie X, Wu Y, Wang Q, Zhao Y, Chen G, Xiang B. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. Journal of pediatric surgery. 2018 Aug:53(8):1464-1468. doi: 10.1016/j.jpedsurg.2017.08.005. Epub 2017 Aug 8 [PubMed PMID: 28827051]
Level 1 (high-level) evidence