Introduction
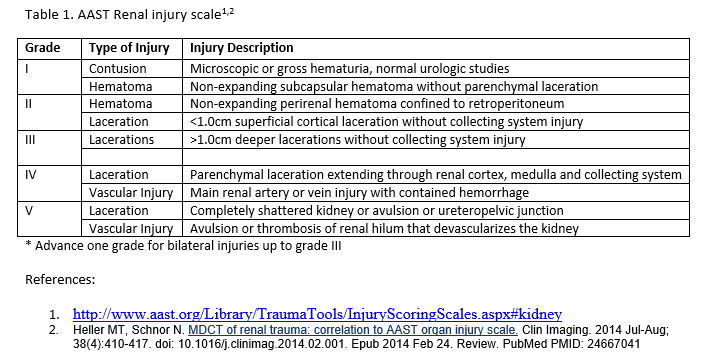
Renal trauma can result in injury to the parenchyma or the renal vasculature which can cause bleeding or injury to the collecting system with possible leakage of urine. Overall, genitourinary tract injuries are rare (10% of all traumas) with the most commonly affected organ being the kidney.[1] Renal trauma accounts for about 1% to 5% of all trauma patients, the majority of which are due to blunt abdominal trauma (80% to 90%).[2][3][4] Although less common, penetrating renal trauma can be up to 20% depending on the location and population served.[3] There is a predominance of young men involved in sports, motor vehicle accidents, assaults or fall (mean age 30) that are noted to more commonly have traumatic renal injuries.[2][5] Based on the American Association for the Surgery of Trauma classification, renal injuries are classified into five grades of injury[3][6] which helps to direct treatment approach and anticipated outcome. The evolution of the management of traumatic renal injuries has evolved into a more non-operative approach as it has been shown that for the same injury angioembolization is successful in preserving a functional kidney as opposed to urgent surgical exploration that frequently resulted in nephrectomy.[7][8] However, it is important to note that renal bleeding that is life threatening still warrants surgical exploration in the hemodynamic unstable patient and remains as an absolute indication.[3][9]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Blunt renal trauma is more common than penetrating renal trauma. The causes of blunt renal trauma in order of frequency are: motor vehicle accidents, falls, sports injuries and pedestrian struck injuries. Blunt injuries can result from a direct blow to the organ, crushing of the organ against the paravertebral muscles or due to rapid deceleration forces. Rapid deceleration can cause avulsion at the ureteropelvic junction, avulsion of the renal vessels, or arterial dissection/thrombosis leading to a devascularized kidney. The most common cause of penetrating renal injury is due to gunshot wounds followed by stab wounds.[5]
Epidemiology
As previously stated, renal trauma accounts for about 1% to 5% of all trauma patients, the majority of which are due to blunt abdominal trauma (80% to 90%).[2][3][4] Of those patients that present with blunt abdominal trauma, 8% to 10 % will have a renal injury while 6% will have a renal injury if it was penetrating.[4] Traumatic blunt or penetrating renal injuries have an 86% association rate with concomitant injuries.[5] Morbidity and mortality are highly dependent on the grade of injury, concomitant injuries, and management intervention. Although renal trauma is still a significant cause of morbidity, renal loss has declined because of a “standard of care” approach in non-operative management for the hemodynamically stable patient regardless of injury grade.[5] The reduction of renal loss is due to the popularization of superselective renal artery angioembolization where there is selective embolization of the bleeding vessel that is targeted to the affected portion of the kidney compared to traditional main artery embolization or nephrectomy resulting in complete loss of the kidney.[5]
History and Physical
Trauma patients with blunt or penetrating injuries to the chest, abdomen, and pelvis have an increased risk of a renal injury, and so it is important to be on high alert during history taking in these patients for possible renal injury. It is also important to recognize the patient with preexisting renal anatomic abnormalities as they can have a significant renal injury with minor trauma, emphasizing the importance of an adequate history intake in these patients.
These patients need a careful examination of their chest, abdomen, flank, and genitourinary regions. Renal injury should be highly suspected in the patient with tenderness, pain, palpable mass or ecchymosis in their flank, abdomen or back.[2] Hematuria increases the suspicion of renal injury but, it is not always present, especially in the polytrauma patient.[10] In penetrating trauma, location of renal injury can be anticipated based on entry or exit wounds based on the form of penetrating trauma (stabbing versus gunshot). For example, a stab wound in the anterior axillary line raises concern for renal hilum (vessels, nerves, ureter) injury whereas, if the posterior axillary line was the point of insertion then the renal parenchyma will more likely be injured. However, for gunshot wounds the trajectory can vary and even though the entry or exit points increases the suspicion of renal trauma, there may not be any renal injury at all.
Evaluation
Laboratory Evaluation
Standard trauma labs should be obtained, for example, complete blood count (CBC), comprehensive metabolic panel (CMP), coagulation panel, lactate, among others, along with urine for analysis. Hematuria is observed more in the blunt renal trauma patient than penetrating renal trauma and if present has an increased frequency of microscopic hematuria versus gross hematuria. Although hematuria can be the landmark of renal injury, the degree of hematuria (present or not) has not shown correlation in predicting the severity of renal injury.[10]
Imaging Evaluation
The modality of choice in the suspected renal trauma patient is contrast-enhanced computed tomography with immediate and delayed imaging.[2][1][6] The different phases of imaging allow evaluation of the renal cortex, renal vessels, and collecting system more accurately because they enhance at different time frames,[11] differentiating urine extravasation from active bleeding.[6] A computed tomography (CT) scan delineates injury findings and severity that would be seen if surgery was performed and the contrast allows evaluation of the renal vessels,[6] where a blush on imaging would support active extravasation. Frequently the first imaging that a trauma patient receives is in the trauma bay with a focused assessment with sonography for trauma (FAST) exam. This imaging exam is conducted to assess for intraabdominal or pericardial fluid, that if present will be highly indicative of bleeding in the trauma patient and assist in timely diagnosis and aid in the decision if operative intervention is warranted.[6] It is an exam that is operator dependent and it’s limited in retroperitoneal bleeding and minor renal injuries.[6] In the hemodynamically stable patient or those who have responded well to resuscitation efforts can be further assessed with contrast-enhanced computed tomography.[7][4] It is important to note that a negative scan does not rule out renal injury and further evaluation is dependent on the patient’s clinical status.[10] Finally, if there is hemodynamic instability that warranted immediate surgical intervention, an intraoperative intravenous urography (IVU) should be performed.[2] Doing so allows assessment of the second kidney function which can further guide the surgical approach to the affected kidney.
Renal imaging should be included, but not limited to the following clinical scenarios[12]:
- Blunt abdominal trauma with gross and microscopic hematuria
- Blunt abdominal trauma with hemodynamic instability
- Penetrating trauma to the chest, abdomen, flank or back and any entry/exit wounds that eludes a trajectory that includes the kidneys
- High clinical suspicion based on the mechanism of injury (i.e., displaced rib fractures adjacent to the kidney, high-speed motor vehicle accident, fall from significant height)
Injury Grading
The American Association for the Surgery of Trauma (AAST) grading system the most common injury grading system used for renal trauma.[4][6][11] Contrast-enhanced CT, which is the gold standard for renal imaging is utilized to grade the renal injury based on this classification system [6].
Treatment / Management
Non-Operative Management
An established consensus among trauma and urological surgeons that initial, non-operative management in the hemodynamically stable renal trauma patient have better overall outcome.[13][2][7][3][14][15][8] The success of this approach is highly due to the advancement in CT imaging allowing classification of the renal injury and the advances made in the techniques of angioembolization.[14][8][12] Non-operative management initially entails supportive care in an intensive care unit (ICU) setting, serial clinical exams, serial hematocrits every 6 to 8 hours, transfusion of blood products and angioembolization or drain placement for urine leakage.[12] With this initial non-operative approach renal function can be preserved and unnecessary nephrectomy avoided.[3][12] As the patient stabilizes, serial labs can decrease in frequency and patient can be downgraded from the ICU to the floor or possibly discharged home. Finally, it is recommended that patients with grade IV or V, if managed non-operatively, should have a repeat contrast enhanced CT 48 to 72 hours from initial scan or earlier if clinically warranted to evaluate for the common complications of bleeding or urinoma in these high grade injuries.[16](A1)
Angiographic Embolization
Selective angiography with angioembolization has revolutionized the evaluation and management of the bleeding patient from a renal injury with a successful embolization rate as high as 88% and renal salvage rate up to 92%.[7][3] An interventional radiologist is needed for this procedure and can be only done at the institutions where they can be available immediately. If this service is not available then the patient should be transferred if it's stable to do so. Angioembolization is preferred over surgery as it has been shown to reduce renal loss and preserve renal function and so increase renal salvage overall.[13][7][3][8](B2)
Operative Management
Renal injury patients who are hemodynamically unstable, unresponsive to resuscitative measures or fail non-operative management should be taken for operative intervention.[9][14][12][17] Persistent bleeding requiring continued red blood cells transfusion or angioembolization, persistent or worsening urine extravasation, renal pelvis or proximal ureteral avulsion are other indication that require surgical intervention.[12] Primary goal in surgical intervention is to control the bleeding and salvage the kidney if possible. If nephrectomy is being considered, it is critical to locate the contralateral kidney by palpation to assure the patient has another kidney. An intravenous pyelogram can be done intraoperatively as well to check for a contralateral functional kidney, which could influence intraoperative management.[4] Operative intervention does not equate to nephrectomy. For example, some injuries can be closed primarily like small stab wounds to the renal parenchyma or injuries to the renal pelvis while partial nephrectomy can be done if sufficient functional renal parenchyma can be obtained.[6][12](A1)
Management Highlights[6][12](A1)
- Most renal injuries are low grade (I through III) and are managed supportively but it doesn't preclude these patients from angiographic embolization (i.e, active bleeding) or surgery (i.e hemodynamic instability)
- Grade IV injuries without expanding hematomas with hemodynamic stability can undergo a trial period of supportive management
- Pelvis-calyceal system injuries can be managed initially with stenting or drainage of the urinoma followed with surgical repair or nephrectomy if failed
- Complete ureteropelvic injuries or renal pedicle avulsion as seen in grade V injuries require surgical repair
- Partial ureteropelvic injuries can be treated with stenting or by diverting the urinary drainage
- All penetrating wounds associated with active bleeding, urine leakage or involve the hilum need to be surgically explored
Differential Diagnosis
- Acute tubular necrosis
- Azotemia
- Chronic kidney disease
- Emergent management of acute glomerulonephritis
- Hemolytic uremic syndrome
- Henoch-Schonlein purpura
- Hyperkalemia
- Hypermagnesemia
- Hypernatremia
- Hypertensive emergencies
Complications
Active bleeding is a complication of traumatic renal injury that is critical and guides the acute management of the injury. Active bleeding is more commonly seen with high-grade injuries (IV and V) but, it can also be seen in lower grade injuries as well (II and III). Delayed bleeding is noted in 2 to 3 weeks from injury and is usually due to either an arteriovenous malformation (AVM) or pseudoaneurysm. AVMs and pseudoaneurysms are sequelae that are more commonly seen with higher grade injuries and penetrating trauma. While active bleeding is a more critical complication with renal trauma necessitating immediate attention, urine extravasation is much more common finding and can be seen in about 7% of patients with renal injuries. Urinoma develops when the urine becomes encapsulated, most commonly in the subcapsular space. Most urinomas will resolve without intervention, and the few that are persistent or become infected will require percutaneous or surgical drainage. Furthermore, hydronephrosis, chronic pyelonephritis, and postrenal hypertension are delayed complications that can also be seen.[18][4]
The most common complications following non-operative management of high grade traumatic renal injuries are hematuria, fever, acute kidney injury and urinoma compared to wound infection, perinephric abscess and urinary tract infection following operative management of these injuries.[16]
Enhancing Healthcare Team Outcomes
In general, an interprofessional approach to patient care among interprofessional health professionals should be the goal for every healthcare facility. The key to implementing this is to utilize an evidence-based approach across all levels of care. In the setting of renal trauma, there is evidence of this collaborative effort in how the management of renal trauma has changed to a more renal salvage approach in light of supporting data and advancement in procedural techniques. Most frequently, the trauma surgeons are the clinicians encountering traumatic renal injuries and are very equipped in knowledge and experience in the management of these injuries. However, in the surgical setting where a nephrectomy may be questionable, it is best to involve the urological service to increase the probability of preserving the kidney when feasible. Urological specialty nursing can perform monitoring, assess therapeutic effectiveness, and keep the team informed of progress or lack of the same. Finally, upon discharge from the hospital or trauma service, post-renal trauma patients should have routine follow up with their primary care physician (possibly for life), especially if high-grade injury or post-nephrectomy, to monitor for hypertension. Therefore, it is important to educate the patient and involve social services as needed to help the patient achieve the best outcome given his or her injury.
Media
References
Baghdanian AH, Baghdanian AA, Armetta A, Babayan RK, LeBedis CA, Soto JA, Anderson SW. Utility of MDCT findings in predicting patient management outcomes in renal trauma. Emergency radiology. 2017 Jun:24(3):263-272. doi: 10.1007/s10140-016-1473-3. Epub 2016 Dec 21 [PubMed PMID: 28004326]
Ząbkowski T, Skiba R, Saracyn M, Zieliński H. Analysis of Renal Trauma in Adult Patients: A 6-Year Own Experiences of Trauma Center. Urology journal. 2015 Sep 4:12(4):2276-9 [PubMed PMID: 26341772]
McPhee M, Arumainayagam N, Clark M, Burfitt N, DasGupta R. Renal injury management in an urban trauma centre and implications for urological training. Annals of the Royal College of Surgeons of England. 2015 Apr:97(3):194-7. doi: 10.1308/003588414X14055925061117. Epub [PubMed PMID: 26263803]
Heller MT, Schnor N. MDCT of renal trauma: correlation to AAST organ injury scale. Clinical imaging. 2014 Jul-Aug:38(4):410-417. doi: 10.1016/j.clinimag.2014.02.001. Epub 2014 Feb 24 [PubMed PMID: 24667041]
Voelzke BB, Leddy L. The epidemiology of renal trauma. Translational andrology and urology. 2014 Jun:3(2):143-9. doi: 10.3978/j.issn.2223-4683.2014.04.11. Epub [PubMed PMID: 26816762]
Dayal M, Gamanagatti S, Kumar A. Imaging in renal trauma. World journal of radiology. 2013 Aug 28:5(8):275-84. doi: 10.4329/wjr.v5.i8.275. Epub [PubMed PMID: 24003353]
Hotaling JM, Sorensen MD, Smith TG 3rd, Rivara FP, Wessells H, Voelzke BB. Analysis of diagnostic angiography and angioembolization in the acute management of renal trauma using a national data set. The Journal of urology. 2011 Apr:185(4):1316-20. doi: 10.1016/j.juro.2010.12.003. Epub 2011 Feb 22 [PubMed PMID: 21334643]
Breyer BN, McAninch JW, Elliott SP, Master VA. Minimally invasive endovascular techniques to treat acute renal hemorrhage. The Journal of urology. 2008 Jun:179(6):2248-52; discussion 2253. doi: 10.1016/j.juro.2008.01.104. Epub 2008 Apr 18 [PubMed PMID: 18423679]
Level 2 (mid-level) evidenceJoseph DK, Daman D, Kinler RL, Burns K, Jacobs L. Management of Major Blunt Renal Injury: A Twelve-Year Review at an Urban, Level I Trauma Hospital. The American surgeon. 2018 Mar 1:84(3):451-454 [PubMed PMID: 29559064]
Brandes SB, McAninch JW. Urban free falls and patterns of renal injury: a 20-year experience with 396 cases. The Journal of trauma. 1999 Oct:47(4):643-9; discussion 649-50 [PubMed PMID: 10528597]
Level 2 (mid-level) evidenceGross JA, Lehnert BE, Linnau KF, Voelzke BB, Sandstrom CK. Imaging of Urinary System Trauma. Radiologic clinics of North America. 2015 Jul:53(4):773-88, ix. doi: 10.1016/j.rcl.2015.02.005. Epub 2015 Apr 9 [PubMed PMID: 26046510]
Mingoli A, La Torre M, Migliori E, Cirillo B, Zambon M, Sapienza P, Brachini G. Operative and nonoperative management for renal trauma: comparison of outcomes. A systematic review and meta-analysis. Therapeutics and clinical risk management. 2017:13():1127-1138. doi: 10.2147/TCRM.S139194. Epub 2017 Aug 31 [PubMed PMID: 28894376]
Level 1 (high-level) evidencevan der Wilden GM, Velmahos GC, Joseph DK, Jacobs L, Debusk MG, Adams CA, Gross R, Burkott B, Agarwal S, Maung AA, Johnson DC, Gates J, Kelly E, Michaud Y, Charash WE, Winchell RJ, Desjardins SE, Rosenblatt MS, Gupta S, Gaeta M, Chang Y, de Moya MA. Successful nonoperative management of the most severe blunt renal injuries: a multicenter study of the research consortium of New England Centers for Trauma. JAMA surgery. 2013 Oct:148(10):924-31. doi: 10.1001/jamasurg.2013.2747. Epub [PubMed PMID: 23945834]
Level 2 (mid-level) evidenceMartin JG, Shah J, Robinson C, Dariushnia S. Evaluation and Management of Blunt Solid Organ Trauma. Techniques in vascular and interventional radiology. 2017 Dec:20(4):230-236. doi: 10.1053/j.tvir.2017.10.001. Epub 2017 Nov 10 [PubMed PMID: 29224654]
Aragona F, Pepe P, Patanè D, Malfa P, D'Arrigo L, Pennisi M. Management of severe blunt renal trauma in adult patients: a 10-year retrospective review from an emergency hospital. BJU international. 2012 Sep:110(5):744-8. doi: 10.1111/j.1464-410X.2011.10901.x. Epub 2012 Feb 7 [PubMed PMID: 22313622]
Level 2 (mid-level) evidenceMorey AF, Brandes S, Dugi DD 3rd, Armstrong JH, Breyer BN, Broghammer JA, Erickson BA, Holzbeierlein J, Hudak SJ, Pruitt JH, Reston JT, Santucci RA, Smith TG 3rd, Wessells H, American Urological Assocation. Urotrauma: AUA guideline. The Journal of urology. 2014 Aug:192(2):327-35. doi: 10.1016/j.juro.2014.05.004. Epub 2014 May 20 [PubMed PMID: 24857651]
Xu J, Yu Q, Zhu S, Li S. Evaluation of a lens opacities classification system II (LOCS II) in the survey population-based sample. Yan ke xue bao = Eye science. 1991 Sep:7(3):140-2 [PubMed PMID: 1842367]
Level 3 (low-level) evidenceStarnes M, Demetriades D, Hadjizacharia P, Inaba K, Best C, Chan L. Complications following renal trauma. Archives of surgery (Chicago, Ill. : 1960). 2010 Apr:145(4):377-81; discussion 381-2. doi: 10.1001/archsurg.2010.30. Epub [PubMed PMID: 20404289]