Introduction
Posterior spinal decompression is one of the most common surgical procedures to release neural structures when nonoperative treatment has failed and is usually the procedure performed for degenerative conditions such as spinal stenosis, especially in middle-aged and elderly patients.[1] It is one of the most common spinal surgeries among cohorts more than 65 years of age. The classical laminectomy constitutes a central, facet joint sparing laminectomy. The spinous process and the lamina are removed limited laterally to the medial part of facet joints. There was no benefit in preserving the midline structures.[2] The central canal, the lateral recesses, and the neural foramina need to be decompressed for good clinical recovery and prevention of failed back surgery syndrome.
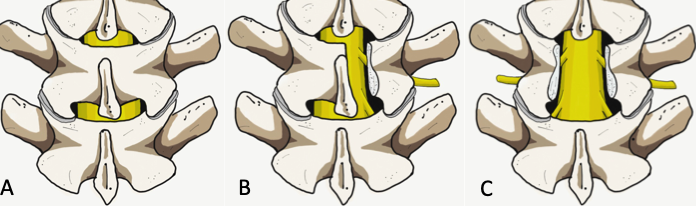
Currently, there are several techniques to accomplish posterior spinal decompression, such as open or minimally invasive laminectomy, hemilaminectomy, laminotomies, and laminoplasty. Decompression techniques classify as direct and indirect; direct procedures involve those techniques with visualization of the dural sac during the surgery, such as laminectomy. On the other hand, indirect decompression takes place without dural sac visualization. Laminectomy alone or associated with fusion is one of the most common procedures performed by a spinal surgeon.[3]
The goals of the surgery include:
- Reduce neurological claudication
- Halt clinical deficits and
- Promote functional ambulation.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Proper knowledge of the posterior vertebral arch and laminae anatomy is imperative to understanding the principles of laminectomy.
The laminae belong to the posterior vertebral arch, extended medially from the base of the spinous process to the junction between the superior and inferior facet joints, acting as a stabilization structure of the spine in association with the facet joint and also as a spinal cord and nerve root protective layer. The laminae's general anatomy consists of a superior and inferior border, an anterior surface in contact with the medullary canal, and a posterior surface that serves as erector spinae muscles attachment. The shape and thickness of the laminae vary according to the anatomical region. Laminar height tends to decrease from C2 to C4 and then increases towards a peak at T8. From T9 to L4 tends to decrease in height and increase in length having at L5 the lowest lumbar height; on the other hand, from cervical to lumbar, laminae width decreases progressively up to the narrowest at T4 in the thoracic region and then increases steadily to reach the widest at L5.
Regarding the thickness, it increases from the cervical to lumbar regions.[4]
A better understanding of the laminae anatomy in different spinal regions may improve surgery success and avoid iatrogenic complications such as nerve root or spinal cord injury.
Indications
The main indication for laminectomy is the presence of spinal canal stenosis; spinal canal narrowing has multiple etiologies, such as congenital, metabolic, traumatic, or tumoral; however, degenerative stenosis is the most common cause. According to Wiltse, spinal stenosis can also be classified into central stenosis, lateral recess, foraminal and extraforaminal stenosis.[5] Also, Lee et al. classified the lateral region into three zones of nerve root compression: entrance zone (lateral recess), mid zone (foraminal region), and exit zone (extraforaminal region) in order to clarify anatomy and surgical strategy.[6] Laminectomy is especially effective for the treatment of central and lateral recess stenosis.
Central stenosis is the most common, and the main symptom is neurogenic claudication, which includes pain, tingling, or cramping sensation in the lower extremity. On the other hand, lateral recess, foraminal, and extraforaminal stenosis may cause radiculopathy, patients with central stenosis may experience more symptoms in standing position and during walking, and pain is usually relieved by leaning forward or in a sitting position. In cases of central stenosis, straight leg raising and femoral nerve stretching test are usually normal.
When symptoms derived from stenosis do not respond to conservative treatment, surgical management such as decompression with or without fusion is usually a consideration.
Fusion techniques are required when stenosis is associated with spinal instability, degenerative or isthmic spondylolisthesis, kyphosis, or scoliosis, as laminectomy alone may increase the risk of spinal instability in these conditions.[7] However, in cases of low-grade degenerative spondylolisthesis, the literature exhibits variable results regarding the risk of instability after laminectomy alone; some studies support fusion in cases of degenerative spondylolisthesis.[8] On the other hand, Wang et al., in a recent meta-analysis, found no increased risk of instability after laminectomy, especially in patients without predominant symptoms of mechanical back pain and after minimally invasive procedures.[9]
Other important indications for laminectomy are primary or secondary tumors, infection (peridural abscesses), trauma (fractures that compromise the spinal canal), and stenosis associated with the deformity.
The radiological armamentarium required in the workup includes:
- CT-criteria for central stenosis include anteroposterior diameter (< 10 mm) and cross-sectional area (< 70 mm2) of spinal canal.[10]
- MRI –Gold standard imaging modality
- Dynamic flexion /extension films- to rule out instability and spondylolisthesis
- EMG- for differentiating distal neuropathies
- Plan X-ray- hip and knee- confounding osteoarthritis
The causes of spinal stenosis can be categorized as:
- Congenital: Achindroplastis dwarfism
- Acquired:
- Degeneration
- Trauma
- Space occupying lesions: Tumors, cysts
- Osseous lesions: Paget and Ankylosing spondylitis.
Indications for laminectomy include:
- Central or lateral canal stenosis refractory to 12 weeks of medication, physical therapy, and injections[11]
- Presence of intractable pain or progressive neurological deficits
- Presentation with cauda equina syndrome
Contraindications
- Spondylolisthesis
- Scoliosis and
- Lateral listhesis
Poor surgical candidates include:
- Patients with multiple medical comorbidities
- Patients with depression, compromised walking, and concurrent scoliosis
Equipment
- Standard radiolucent table with spinal frames and foams pads
- C-arm to localize level and minimize skin size incision
- Laminectomy instrument set (bone cutting rongeurs, high-speed burr, Kerrison rongeurs, forceps, ball tip, angled spatula spreader, bayonet-shaped curettes, hollow probes, tubular retractors, and dilators for MIS approaches)
Personnel
- One or two spinal surgeons, a registered OT nurse staff, and anesthesiologists
- Neuromonitoring is usually a recommendation in cervical or dorsal laminectomies and lumbar cases when there is an increased risk of nerve injury
Preparation
Laminectomy is performed with the patient in the prone position on a support frame with foam pads for nipples and ASIS (anterior superior iliac crest spine), leaving the abdomen free, avoiding abdominal pressure decreases epidural venous pressure and, therefore, surgical site bleeding.
Arms are positioned at 90 degrees abduction and flexion to prevent axillary nerve injury.
Technique or Treatment
Laminectomy can be performed through a traditional open approach or with a minimally invasive technique.
The traditional open approach requires a posterior midline incision (3 to 4 cm in length for a single level) and subperiosteal dissection along spinous processes to detach and retract paraspinous muscles from the spinous processes medially to the lateral laminar border avoiding damage to the facet joint. Spinous processes may be resected along with dorsal laminae to expose ligamentum flavum with bone cutting rongeur or a burr, resection of ligamentum flavum is possible with Woodson elevator and spatula, and medial facetectomies can be performed to decompress the lateral recess. The foraminal region can is reachable with Kerrison rongeurs. Use of a ball tip or angled probe help to assess foraminal size. Great care is necessary to avoid damage to pars interarticularis and more than 50% of the facet joint to decrease the risk of instability. The decompression procedure is usually complete upon confirmation of the dural sac, exiting, and descending nerve roots.
Minimally Invasive Surgical (MIS) techniques include laminotomy and microendoscopic laminotomy with tubular retractors. Contemporary literature supports these procedures resulting in better preservation of posterior musculature, decreased intraoperative bleeding, and postoperative pain.[12][13]
Even though MIS approaches may have some early outcome advantages over open procedures, the economic value and cost-effectiveness of MIS require further investigation.
A recent systematic review compared conventional laminectomy with three different techniques that avoid removing the spinous process (unilateral laminotomy, bilateral laminotomy, and split spinous process laminotomy). A decreased postoperative back pain for bilateral laminotomy and split spinous laminotomy was found; however, there were no observable clinically significant differences. Further, there was no difference in terms of hospital length of stay, operative time, and complications of these techniques compared to conventional laminectomy.[14]
The salient surgical steps in classical decompressive laminectomy can be summarized as follows:
- Prone positioning
- The abdomen should be made free of any undue pressure
- Anatomical localization aided with fluoroscopy
- Superficial tissue and muscle dissection to reach the spinous process
- Subperiosteal dissection of lamina-not exceeding axis of facet joints in classical laminectomy and not exceeding tip of the transverse process in others
- Spinous process removal via large rongeur or Horsley bone cutter
- Removal of the lamina via Leksell rongeur starting from the inter-laminar space
- Removal of thickened ligament flavum via Kerrison rongeur
- A high-speed drill to thin the lamina followed by its removal via Kerrison can also be undertaken
- Undercutting of medial facet and decompression of respective foramina
- Layered wound closure after ensuring hemostasis and placement of a drain
Complications
Instability: Damage to the pars interarticularis is a risk. Damage to more than fifty percent of facets on both sides or complete facets on one side intraoperatively mandates fusion surgery. Since L1-3 has a narrow surgical corridor for decompression, preservation of pars is of paramount importance at these levels.[15]
Bony Re-growth[16]
Kyphosis: due to disruption of posterior tension banding function of posterior Osseo-ligamentous complex.[17][18]
Spinal epidural hematoma: maximum risk at the L2/3 level.[19]
Dural tear: The incidence is 3.1% to 13% and 8.1% to 17.4% for primary and revision surgery, respectively. It increases the risk of surgical site infections, postoperative deficits, and delirium. The most location is the lower surgical field near the nerve root, followed by the dorsal sac.PMC4206814 Previous surgery and older age were found to be risk variables.[20] The dural closure technique does not impact revision surgery rates or its complications. Primary repair followed by bed rest is advocated.[21] Minimal access surgeries produce minimal dead space, reducing the risk of pseudomeningocele and CSF fistula.
Mortality: incidence of 0.5 to 2.3%.
Clinical Significance
Laminectomy is one of the most common procedures performed among spinal surgeons to treat spinal stenosis. This technique, correctly performed, correlates with symptomatic improvement and early recovery with relatively low complication rates. Even when the benefits of surgical versus nonsurgical treatment in lumbar stenosis have not been proven. [Level 1] Laminectomy remains an effective surgical technique for various conditions affecting the spinal canal, such as tumors, epidural abscess, and spondylotic myelopathy.[22]
Results of the Procedure
- The success rate of 90% with a patient satisfaction rate of above 75%
- Pain and weakness resolve early, whereas dysesthesias may take up to two years
- Reoperation Rate-18% within five years
Causes of Failure
- Adjacent segment stenosis
- Disc herniation
- Spondylolisthesis
- Re-stenosis[23]
Variants of Classical Laminectomy (high-risk factors precluding true decompression)
- Bilateral laminotomies
- Skip laminectomy
- Split spinous process decompression
- Bilateral decompression from a unilateral approach
Different Surgical Modalities
- Decompression with conventional laminectomy
- Bilateral decompression via the unilateral approach
- Decompression with fusion: Fusion has increased risks of blood loss, infection, longer hospital stays, and higher costs.[24][25] Decompression alone is not inferior to fusion surgeries.[26][27][27] A concomitant fusion should be considered for patients with spondylolisthesis, scoliosis, and lateral listhesis.
- Augmentation laminoplasty causes less surgical trauma.[28][29][30]
- Endoscopic decompression: low risk of recurrence, preserve stability, minimal blood loss and complications[31][32][33][34][35][36]
- Interspinous process devices: high dislocation, fracture of the spinous process, and low cost-effectiveness.[37][38]
- Decompression with Interlaminar stabilization
- Decompression with lumbar spinal process-splitting laminectomy: less postoperative pain.[39]
- Minimally invasive tubular decompression: reduced trauma, rapid recovery, shorter operating time and lesser intraoperative blood loss, and a better satisfaction rate.[40][41][42] ranked top for most outcomes for treating single-segment LSS.[43]
- Microscopic decompression.[16][44]
- Robot-assisted.[45]
Helpful Armamentarium
- Machine learning and Artificial Intelligence.[46]
- Surgical simulations.[47]
- Intraoperative sonography to confirm restoration of the subarachnoid space.[48][49]
- Intraoperative neuromonitoring has not been found to be reliable at predicting new neurologic deficits but is a useful adjunct to ease the surgeon when no intraoperative abnormalities are detected.[50]
- Anti-fibrotic agents may prevent epidural fibrosis and adhesions.[51]
- The 3D-printed artificial lamina may help in facilitating stability.[52]
Enhancing Healthcare Team Outcomes
Laminectomy is among the most common procedures spinal surgeons perform to decompress the spinal canal in various conditions. Preoperative and postoperative patient care is crucial to improving outcomes of laminectomy. General practitioners, nurses, and pharmacists should advise the patient to change lifestyle, such as weight control and stop smoking. Making referrals to other professionals is essential when concomitant and associated pathologies could be present. All involved members of the interprofessional team need to communicate across interprofessional lines to achieve optimal outcomes. [Level 5]
Complete comprehensive preoperative planning requires assessment. It is essential to carefully document neurological status before surgery and develop correct and complete operative consent describing the magnitude, scope, and detailed complications of the surgery, as well as detailed alternatives considering nonoperative management. The nurse plays a role during the preoperative preparation of patients undergoing spine surgery. The nurse assists the clinician during the procedure and helps with the proper positioning of the patient. The nurse monitors the patient's vital signs before, during, and after the procedure. If there are any untoward changes in the patient's observations, the nurse should immediately alert the clinician and document the findings in the patient's medical records. The nurse should counsel patients appropriately about their care plans and ensure that the patient understands all components of valid consent. The best possible outcome for patients undergoing laminectomy could only be fostered through clear and efficient communication and collaboration among the interprofessional team members. [Level 5]
Relief of symptoms by bending forward is a reliable clinical variable in canal stenosis.[53] Physical variables alone were not found to be predictors of a favorable postoperative outcome.[54] A combination of clinical and radiological variables is of utmost importance.[55][56] The relief of pain after epidural steroid injections may be a good prognostic indicator of surgical outcome. The neurological deficit and low comorbidity were good prognostic indicators for favorable outcomes.[57] Increased signal intensity within the cord is a prognostic variable.[58]
Multivariate analysis showed medical comorbidities, previous laminectomy, and accidental durotomy increased the risk of surgical complications.[59] Independent risk factors for readmission were long operative time, previous spinal surgery, and extended hospital stays.[60]
Multi-national Scandinavia study showed similar indications for decompression surgery but significant differences in advocating arthrodesis. Fusion did not improve effectiveness.[61] There was no significant difference in the clinical outcome while comparing unilateral laminotomy with crossover, bilateral laminotomy, and spinous process osteotomy.[62]
Outpatient Versus Inpatient Surgery
Outpatient surgery is comparable to inpatient surgery. Risk variables such as BMI >30 kg/m^2, age ≥55 years, functional dependency, medical comorbidities, and operative time >90 minutes have been linked to increased risk of complications in cohorts undergoing outpatient surgery.
Nursing, Allied Health, and Interprofessional Team Interventions
The nurse's role in the postoperative period should include finite management of intravenous fluids, foley catheter care until ambulating, administering antibiotics, pain control, wound/dressing care, encouraging patient ambulation, and advanced diet when appropriate.
Nursing, Allied Health, and Interprofessional Team Monitoring
Postoperative patient monitoring is essential for recognizing some early complications, especially CSF leakage from dural sac tears; it is crucial to evaluate the wound by looking for some suggestive signs, such as wound bulging or CSF sinus. Clinical signs of CSF leakage, such as headache and dizziness, should raise alert from possible complications.
The presence of erythema, increased pain, or swelling may raise the suspicion of wound infection.
Media
(Click Image to Enlarge)
References
Binder DK, Schmidt MH, Weinstein PR. Lumbar spinal stenosis. Seminars in neurology. 2002 Jun:22(2):157-66 [PubMed PMID: 12524561]
Elmqvist E, Lindhagen L, Försth P. No Benefit with Preservation of Midline Structures in Decompression for Lumbar Spinal Stenosis: Results From the National Swedish Spine Registry 2-Year Post-Op. Spine. 2022 Apr 1:47(7):531-538. doi: 10.1097/BRS.0000000000004313. Epub [PubMed PMID: 34923549]
Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis. The Cochrane database of systematic reviews. 2005 Oct 19:2005(4):CD001352 [PubMed PMID: 16235281]
Level 1 (high-level) evidenceXu R, Burgar A, Ebraheim NA, Yeasting RA. The quantitative anatomy of the laminas of the spine. Spine. 1999 Jan 15:24(2):107-13 [PubMed PMID: 9926378]
Arnoldi CC, Brodsky AE, Cauchoix J, Crock HV, Dommisse GF, Edgar MA, Gargano FP, Jacobson RE, Kirkaldy-Willis WH, Kurihara A, Langenskiöld A, Macnab I, McIvor GW, Newman PH, Paine KW, Russin LA, Sheldon J, Tile M, Urist MR, Wilson WE, Wiltse LL. Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clinical orthopaedics and related research. 1976 Mar-Apr:(115):4-5 [PubMed PMID: 1253495]
Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine. 1988 Mar:13(3):313-20 [PubMed PMID: 3388117]
Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997 Dec 15:22(24):2807-12 [PubMed PMID: 9431616]
Level 1 (high-level) evidenceGhogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC. Laminectomy plus Fusion versus Laminectomy Alone for Lumbar Spondylolisthesis. The New England journal of medicine. 2016 Apr 14:374(15):1424-34. doi: 10.1056/NEJMoa1508788. Epub [PubMed PMID: 27074067]
Wang M, Luo XJ, Ye YJ, Zhang Z. Does Concomitant Degenerative Spondylolisthesis Influence the Outcome of Decompression Alone in Degenerative Lumbar Spinal Stenosis? A Meta-Analysis of Comparative Studies. World neurosurgery. 2019 Mar:123():226-238. doi: 10.1016/j.wneu.2018.11.246. Epub 2018 Dec 18 [PubMed PMID: 30576810]
Level 2 (mid-level) evidenceSteurer J, Roner S, Gnannt R, Hodler J, LumbSten Research Collaboration. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC musculoskeletal disorders. 2011 Jul 28:12():175. doi: 10.1186/1471-2474-12-175. Epub 2011 Jul 28 [PubMed PMID: 21798008]
Level 1 (high-level) evidenceWeinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H, SPORT Investigators. Surgical versus nonsurgical therapy for lumbar spinal stenosis. The New England journal of medicine. 2008 Feb 21:358(8):794-810. doi: 10.1056/NEJMoa0707136. Epub [PubMed PMID: 18287602]
Level 1 (high-level) evidenceRahman M, Summers LE, Richter B, Mimran RI, Jacob RP. Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the "classic" open approach. Minimally invasive neurosurgery : MIN. 2008 Apr:51(2):100-5. doi: 10.1055/s-2007-1022542. Epub [PubMed PMID: 18401823]
Level 2 (mid-level) evidencePhan K, Mobbs RJ. Minimally Invasive Versus Open Laminectomy for Lumbar Stenosis: A Systematic Review and Meta-Analysis. Spine. 2016 Jan:41(2):E91-E100. doi: 10.1097/BRS.0000000000001161. Epub [PubMed PMID: 26555839]
Level 1 (high-level) evidenceOverdevest G, Vleggeert-Lankamp C, Jacobs W, Thomé C, Gunzburg R, Peul W. Effectiveness of posterior decompression techniques compared with conventional laminectomy for lumbar stenosis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2015 Oct:24(10):2244-63. doi: 10.1007/s00586-015-4098-4. Epub 2015 Jul 17 [PubMed PMID: 26184719]
Njoku IU, Park JY, Munim MA, Clarke A, Cheng CW. An Anatomic Study Examining Lumbar Pars Interarticularis Distance and Spinal Canal Width in Relation to Lumbar Decompressive Surgery. International journal of spine surgery. 2022 Jun 20:16(4):646-50. doi: 10.14444/8292. Epub 2022 Jun 20 [PubMed PMID: 35728832]
Shimauchi-Ohtaki H, Minami M, Takahashi T, Kanematsu R, Honda F, Hanakita J. Lumbar Canal Stenosis Caused by Marked Bone Overgrowth after Decompression Surgery. Case reports in orthopedics. 2022:2022():9462399. doi: 10.1155/2022/9462399. Epub 2022 Jun 3 [PubMed PMID: 35692944]
Level 3 (low-level) evidenceTakahashi K, Ogawa S, Isefuku S, Hashimoto K, Aizawa T. Post-laminectomy cervical flexion myelopathy and its possible pathomechanism: A case report. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2022 May 24:():. pii: S0949-2658(22)00122-1. doi: 10.1016/j.jos.2022.05.002. Epub 2022 May 24 [PubMed PMID: 35623992]
Level 3 (low-level) evidenceYang K, Li XY, Wang Y, Kong C, Lu SB. Mechanisms of compensatory for cervical lordosis changes after laminectomy with fusion. BMC surgery. 2022 Apr 7:22(1):129. doi: 10.1186/s12893-022-01577-0. Epub 2022 Apr 7 [PubMed PMID: 35392874]
Bekki H, Arizono T, Inokuchi A, Imamura R, Hamada T, Oyama R, Hyodo Y, Kinoshita E, Kido M. Risk Factors for Incidence of Postoperative Spinal Epidural Hematoma Following Multilevel Microendoscopic Laminectomy. Spine surgery and related research. 2022:6(1):45-50. doi: 10.22603/ssrr.2021-0025. Epub 2021 Jun 11 [PubMed PMID: 35224246]
Smorgick Y, Baker KC, Herkowitz H, Montgomery D, Badve SA, Bachison C, Ericksen S, Fischgrund JS. Predisposing factors for dural tear in patients undergoing lumbar spine surgery. Journal of neurosurgery. Spine. 2015 May:22(5):483-6. doi: 10.3171/2015.1.SPINE13864. Epub 2015 Feb 20 [PubMed PMID: 25700240]
Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. The Journal of bone and joint surgery. American volume. 1998 Dec:80(12):1728-32 [PubMed PMID: 9875930]
Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. The Cochrane database of systematic reviews. 2016 Jan 29:2016(1):CD010264. doi: 10.1002/14651858.CD010264.pub2. Epub 2016 Jan 29 [PubMed PMID: 26824399]
Level 1 (high-level) evidenceAwaya T, Nishimura Y, Eguchi K, Nagashima Y, Ando R, Akahori S, Yoshikawa S, Haimoto S, Hara M, Takayasu M, Saito R. Radiological Analysis of Minimally Invasive Microscopic Laminectomy for Lumbar Canal Stenosis with a Focus on Multilevel Stenosis and Spondylolisthesis. World neurosurgery. 2022 Aug:164():e224-e234. doi: 10.1016/j.wneu.2022.04.079. Epub 2022 Apr 25 [PubMed PMID: 35483569]
Katz JN, Zimmerman ZE, Mass H, Makhni MC. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA. 2022 May 3:327(17):1688-1699. doi: 10.1001/jama.2022.5921. Epub [PubMed PMID: 35503342]
McDonald CL, Hershman SH, Hogan W, Alsoof D, DiSilvestro KJ, Zhang AS, Kuris EO, Daniels AH. Cervical Laminoplasty Versus Posterior Laminectomy and Fusion: Trends in Utilization and Evaluation of Complication and Revision Surgery Rates. The Journal of the American Academy of Orthopaedic Surgeons. 2022 Sep 1:30(17):858-866. doi: 10.5435/JAAOS-D-22-00106. Epub 2022 May 30 [PubMed PMID: 35640093]
Abdel-Fattah AR, Bell F, Boden L, Ferry J, McCormick C, Ross M, Cameron I, Smith T, Baliga S, Myint PK. To fuse or not to fuse: The elderly patient with lumbar stenosis and low-grade spondylolisthesis. Systematic review and meta-analysis of randomised controlled trials. The surgeon : journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2023 Feb:21(1):e23-e31. doi: 10.1016/j.surge.2022.02.008. Epub 2022 Mar 16 [PubMed PMID: 35305933]
Level 1 (high-level) evidenceRevesz DF, Charalampidis A, Gerdhem P. Effectiveness of laminectomy with fusion and laminectomy alone in degenerative cervical myelopathy. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2022 May:31(5):1300-1308. doi: 10.1007/s00586-022-07159-1. Epub 2022 Mar 14 [PubMed PMID: 35288770]
Ovalioglu TC, Ozdemir Ovalioglu A, Canaz G, Gunes M, Babur M, Emel E. Efficacy of Spinous Process Splitting Decompression Compared with Conventional Laminectomy for Degenerative Lumbar Stenosis. World neurosurgery. 2022 Aug:164():e1233-e1242. doi: 10.1016/j.wneu.2022.06.015. Epub 2022 Jun 9 [PubMed PMID: 35691518]
Afshari FT, Slator N, Fayeye O, Ramakrishnan PK, Solanki GA. Spinal canal stenosis in children with achondroplasia: the role of augmentation laminoplasty-a 15-year single institution experience. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2023 Jan:39(1):229-237. doi: 10.1007/s00381-022-05566-9. Epub 2022 Jun 2 [PubMed PMID: 35654849]
Schmeiser G, Bergmann JI, Papavero L, Kothe R. Surgical Treatment of Multilevel Degenerative Cervical Myelopathy: Open-Door Laminoplasty and Fixation via Unilateral Approach. A Feasibility Study. Journal of neurological surgery. Part A, Central European neurosurgery. 2022 Sep:83(5):494-501. doi: 10.1055/s-0041-1739224. Epub 2021 Dec 15 [PubMed PMID: 34911089]
Level 2 (mid-level) evidenceOichi T, Oshima Y, Chikuda H, Ohya J, Matsui H, Fushimi K, Tanaka S, Yasunaga H. In-hospital complication rate following microendoscopic versus open lumbar laminectomy: a propensity score-matched analysis. The spine journal : official journal of the North American Spine Society. 2018 Oct:18(10):1815-1821. doi: 10.1016/j.spinee.2018.03.010. Epub 2018 Mar 19 [PubMed PMID: 29567515]
Deng Y, Yang M, Xia C, Chen Y, Xie Z. Unilateral biportal endoscopic decompression for symptomatic thoracic ossification of the ligamentum flavum: a case control study. International orthopaedics. 2022 Sep:46(9):2071-2080. doi: 10.1007/s00264-022-05484-0. Epub 2022 Jun 21 [PubMed PMID: 35725953]
Level 2 (mid-level) evidenceChen T, Zhou G, Chen Z, Yao X, Liu D. Biportal endoscopic decompression vs. microscopic decompression for lumbar canal stenosis: A systematic review and meta-analysis. Experimental and therapeutic medicine. 2020 Sep:20(3):2743-2751. doi: 10.3892/etm.2020.9001. Epub 2020 Jul 13 [PubMed PMID: 32765769]
Level 1 (high-level) evidenceLi Y, Bi J, Sun Z, Ren J, Liu X, Sun N, Wang J, Li R. Phase I 270° single-incision percutaneous spinal endoscopy for decompression treatment of thoracic spinal stenosis. Scientific reports. 2022 Jun 8:12(1):9448. doi: 10.1038/s41598-022-13666-4. Epub 2022 Jun 8 [PubMed PMID: 35676323]
Zhu C, Deng X, Pan H, Zhang W. Unilateral biportal endoscopic laminectomy with lateral mass screw fixation for treating cervical spinal stenosis. Acta neurochirurgica. 2022 Jun:164(6):1529-1533. doi: 10.1007/s00701-022-05212-y. Epub 2022 Apr 29 [PubMed PMID: 35486201]
Lewandrowski KU, Abraham I, Ramírez León JF, Soriano Sánchez JA, Dowling Á, Hellinger S, Freitas Ramos MR, Teixeira De Carvalho PS, Yeung C, Salari N, Yeung A. Differential Agnostic Effect Size Analysis of Lumbar Stenosis Surgeries. International journal of spine surgery. 2022 Apr:16(2):318-342. doi: 10.14444/8222. Epub [PubMed PMID: 35444041]
Zini C, Bellini M, Masala S, Marcia S. Percutaneous Interspinous Spacer in Spinal-Canal-Stenosis Treatment: Pros and Cons. Medicina (Kaunas, Lithuania). 2019 Jul 16:55(7):. doi: 10.3390/medicina55070381. Epub 2019 Jul 16 [PubMed PMID: 31315310]
Poetscher AW, Gentil AF, Ferretti M, Lenza M. Interspinous process devices for treatment of degenerative lumbar spine stenosis: A systematic review and meta-analysis. PloS one. 2018:13(7):e0199623. doi: 10.1371/journal.pone.0199623. Epub 2018 Jul 6 [PubMed PMID: 29979691]
Level 1 (high-level) evidenceVoglis S, Tosic L, Höbner LM, Hofer AS, Stienen MN, Regli L, Bellut D, Dias SF. Spinous-Process-Splitting Versus Conventional Decompression for Lumbar Spinal Stenosis: Comparative Study with Respect to Short-Term Postoperative Pain and Analgesics Use. World neurosurgery. 2022 Apr:160():e80-e87. doi: 10.1016/j.wneu.2021.12.094. Epub 2021 Dec 29 [PubMed PMID: 34973440]
Level 2 (mid-level) evidenceZhao XB, Ma YJ, Ma HJ, Zhang XY, Zhou HG. Clinical Efficacy of Posterior Percutaneous Endoscopic Unilateral Laminotomy with Bilateral Decompression for Symptomatic Cervical Spondylotic Myelopathy. Orthopaedic surgery. 2022 May:14(5):876-884. doi: 10.1111/os.13237. Epub 2022 Apr 19 [PubMed PMID: 35441460]
Ohtomo N, Nakamoto H, Miyahara J, Yoshida Y, Nakarai H, Tozawa K, Fukushima M, Kato S, Doi T, Taniguchi Y, Matsubayashi Y, Higashikawa A, Takeshita Y, Kawamura N, Inanami H, Tanaka S, Oshima Y. Comparison between microendoscopic laminectomy and open posterior decompression surgery for single-level lumbar spinal stenosis: a multicenter retrospective cohort study. BMC musculoskeletal disorders. 2021 Dec 20:22(1):1053. doi: 10.1186/s12891-021-04963-6. Epub 2021 Dec 20 [PubMed PMID: 34930238]
Level 2 (mid-level) evidenceZhao H, Ren R, Ma W, Xu S, Peng L, Zhong Z, Zheng Y. Comparison of Laminoplasty vs. Laminectomy for Cervical Spondylotic Myelopathy: A Systematic Review and Meta-Analysis. Frontiers in surgery. 2021:8():790593. doi: 10.3389/fsurg.2021.790593. Epub 2022 Jan 17 [PubMed PMID: 35111804]
Level 1 (high-level) evidenceLiang Z, Xu X, Chen X, Zhuang Y, Wang R, Chen C. Clinical Evaluation of Surgery for Single-Segment Lumbar Spinal Stenosis: A Systematic Review and Bayesian Network Meta-Analysis. Orthopaedic surgery. 2022 Jul:14(7):1281-1293. doi: 10.1111/os.13269. Epub 2022 May 18 [PubMed PMID: 35582931]
Level 1 (high-level) evidenceNerland US, Jakola AS, Solheim O, Weber C, Rao V, Lønne G, Solberg TK, Salvesen Ø, Carlsen SM, Nygaard ØP, Gulati S. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ (Clinical research ed.). 2015 Apr 1:350():h1603. doi: 10.1136/bmj.h1603. Epub 2015 Apr 1 [PubMed PMID: 25833966]
Level 2 (mid-level) evidenceLi Z, Jiang S, Song X, Liu S, Wang C, Hu L, Li W. Collaborative spinal robot system for laminectomy: a preliminary study. Neurosurgical focus. 2022 Jan:52(1):E11. doi: 10.3171/2021.10.FOCUS21499. Epub [PubMed PMID: 34973664]
Soin A, Hirschbeck M, Verdon M, Manchikanti L. A Pilot Study Implementing a Machine Learning Algorithm to Use Artificial Intelligence to Diagnose Spinal Conditions. Pain physician. 2022 Mar:25(2):171-178 [PubMed PMID: 35322974]
Level 3 (low-level) evidenceMelcher C, Hussain I, Kirnaz S, Goldberg JL, Sommer F, Navarro-Ramirez R, Medary B, Härtl R. Use of a High-Fidelity Training Simulator for Minimally Invasive Lumbar Decompression Increases Working Knowledge and Technical Skills Among Orthopedic and Neurosurgical Trainees. Global spine journal. 2022 Feb 28:():21925682221076044. doi: 10.1177/21925682221076044. Epub 2022 Feb 28 [PubMed PMID: 35225716]
Biczok A, Fuetsch M, Siller S, Patzig M, Tonn JC, Zausinger S. Intraoperative ultrasonography in laminectomy for degenerative cervical spondylotic myelopathy: a clinical and radiological evaluation. Acta neurochirurgica. 2022 Jul:164(7):1873-1881. doi: 10.1007/s00701-022-05232-8. Epub 2022 May 10 [PubMed PMID: 35536511]
Rustagi T, Das K, Chhabra HS. Revisiting the Role of Intraoperative Ultrasound in Spine Surgery for Extradural Pathologies: Review and Clinical Usage. World neurosurgery. 2022 Aug:164():118-127. doi: 10.1016/j.wneu.2022.04.116. Epub 2022 Apr 30 [PubMed PMID: 35504481]
Koffie RM, Morgan CD, Giraldo JP, Angel S, Walker CT, Godzik J, Catapano JS, Hemphill C, Uribe JS. Should Somatosensory and Motor Evoked Potential Monitoring Be Used Routinely in All Posterior Cervical Operations for Degenerative Conditions of the Cervical Spine? World neurosurgery. 2022 Jun:162():e86-e90. doi: 10.1016/j.wneu.2022.02.080. Epub 2022 Feb 24 [PubMed PMID: 35219916]
Ding Q, Wei Q, Sheng G, Wang S, Jing S, Ma T, Zhang R, Wang T, Li W, Tang X, Wu H, Liu C. The Preventive Effect of Decorin on Epidural Fibrosis and Epidural Adhesions After Laminectomy. Frontiers in pharmacology. 2021:12():774316. doi: 10.3389/fphar.2021.774316. Epub 2021 Dec 16 [PubMed PMID: 34975478]
Li J, He Z, Liu X, Li S, Yin Y, Fang G, Chen Y, Pang G, Lu J, Liu Z, Ye G. 3D-Printed Bionic Titanium Alloy Artificial Lamina Prevents Epidural Adhesion and Restores the Stability After Laminectomy in Pigs. Journal of biomedical nanotechnology. 2022 Mar 1:18(3):875-883. doi: 10.1166/jbn.2022.3290. Epub [PubMed PMID: 35715907]
Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 2010 Dec 15:304(23):2628-36. doi: 10.1001/jama.2010.1833. Epub [PubMed PMID: 21156951]
Level 3 (low-level) evidenceMarchand AA, Houle M, O'Shaughnessy J, Châtillon CÉ, Descarreaux M. Physical Predictors of Favorable Postoperative Outcomes in Patients Undergoing Laminectomy or Laminotomy for Central Lumbar Spinal Stenosis: Secondary Analysis of a Randomized Controlled Trial. Frontiers in neurology. 2022:13():848665. doi: 10.3389/fneur.2022.848665. Epub 2022 Apr 15 [PubMed PMID: 35493839]
Level 1 (high-level) evidencePrasad BC, Ramesh Chandra VV, Devi BV, Chivukula SS, Pundarikakshaiah K. Clinical, radiological, and functional evaluation of surgical treatment in degenerative lumbar canal stenosis. Neurology India. 2016 Jul-Aug:64(4):677-83. doi: 10.4103/0028-3886.185378. Epub [PubMed PMID: 27381113]
Munakomi S. Letter to the Editor. Reappraising role of clinical evaluations in degenerative lumbar spine pathologies. Journal of neurosurgery. Spine. 2019 Mar 8:():1-2. doi: 10.3171/2018.10.SPINE181282. Epub 2019 Mar 8 [PubMed PMID: 30849747]
Level 3 (low-level) evidenceFoulongne E, Derrey S, Ould Slimane M, Levèque S, Tobenas AC, Dujardin F, Fréger P, Chassagne P, Proust F. Lumbar spinal stenosis: which predictive factors of favorable functional results after decompressive laminectomy? Neuro-Chirurgie. 2013 Feb:59(1):23-9. doi: 10.1016/j.neuchi.2012.09.005. Epub 2012 Dec 14 [PubMed PMID: 23246374]
Zhang C, Yang S, Wang L, Wang N, Ke Z, Liu P, Zhang C, Xiong C, Zhao R, Liang H, Luo X. Preoperative Magnetic Resonance Imaging Signal Intensity Classification Is Associated With Clinical Presentation and Surgical Outcomes in Myelopathy Caused by Thoracic Ossification of Ligamentum Flavum: A Multicenter Study. Global spine journal. 2021 Dec 16:():21925682211067752. doi: 10.1177/21925682211067752. Epub 2021 Dec 16 [PubMed PMID: 34911374]
Level 2 (mid-level) evidenceRault F, Briant AR, Kamga H, Gaberel T, Emery E. Surgical management of lumbar spinal stenosis in patients over 80: is there an increased risk? Neurosurgical review. 2022 Jun:45(3):2385-2399. doi: 10.1007/s10143-022-01756-w. Epub 2022 Mar 3 [PubMed PMID: 35243565]
Cho PG, Kim TH, Lee H, Ji GY, Park SH, Shin DA. Incidence, reasons, and risk factors for 30-day readmission after lumbar spine surgery for degenerative spinal disease. Scientific reports. 2020 Jul 29:10(1):12672. doi: 10.1038/s41598-020-69732-2. Epub 2020 Jul 29 [PubMed PMID: 32728078]
Lønne G, Fritzell P, Hägg O, Nordvall D, Gerdhem P, Lagerbäck T, Andersen M, Eiskjaer S, Gehrchen M, Jacobs W, van Hooff ML, Solberg TK. Lumbar spinal stenosis: comparison of surgical practice variation and clinical outcome in three national spine registries. The spine journal : official journal of the North American Spine Society. 2019 Jan:19(1):41-49. doi: 10.1016/j.spinee.2018.05.028. Epub 2018 May 21 [PubMed PMID: 29792994]
Level 2 (mid-level) evidenceHermansen E, Austevoll IM, Hellum C, Storheim K, Myklebust TÅ, Aaen J, Banitalebi H, Anvar M, Rekeland F, Brox JI, Franssen E, Weber C, Solberg TK, Furunes H, Grundnes O, Brisby H, Indrekvam K. Comparison of 3 Different Minimally Invasive Surgical Techniques for Lumbar Spinal Stenosis: A Randomized Clinical Trial. JAMA network open. 2022 Mar 1:5(3):e224291. doi: 10.1001/jamanetworkopen.2022.4291. Epub 2022 Mar 1 [PubMed PMID: 35344046]
Level 1 (high-level) evidence