Definition/Introduction
First described by Thomas B. Fitzpatrick in 1972, the Fitzpatrick skin phototypes were developed based on an individual's skin color and their tendency to burn or tan when exposed to sunlight. More specifically, classification was based on a patient's responses to the following questions regarding their skin's reaction to a 45-60 minute, early summer, noon sun exposure in northern latitudes (20-45 degrees): "how painful is your sunburn?" and "how much tan will you develop in a week?" Initially enumerated as skin types I through IV to classify patients with white skin, the Fitzpatrick phototype classification scale was later modified to include types V and VI for persons with darker skin.[1] Generally, a lower Fitzpatrick skin type classification indicates skin that burns more easily than it tans, while a higher Fitzpatrick skin type indicates the opposite (Table 1). The most common skin type in the United States is type III (48%), with types I and II comprising the second largest group (35% in total).[2] See Table. Fitzpatrick Skin Type Descriptions I to VI.
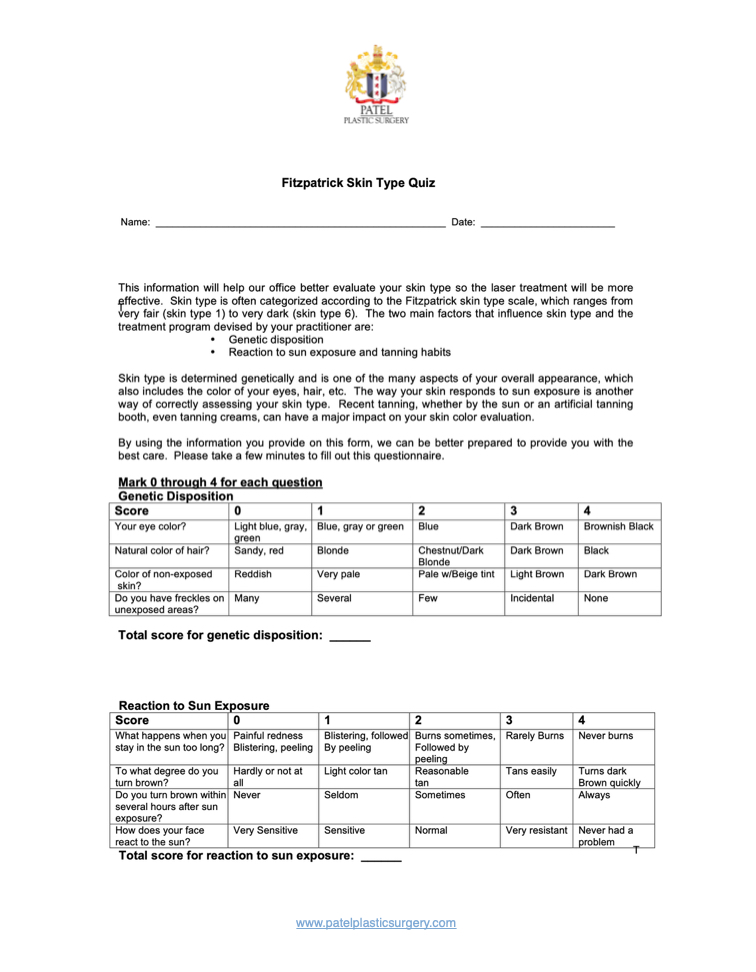
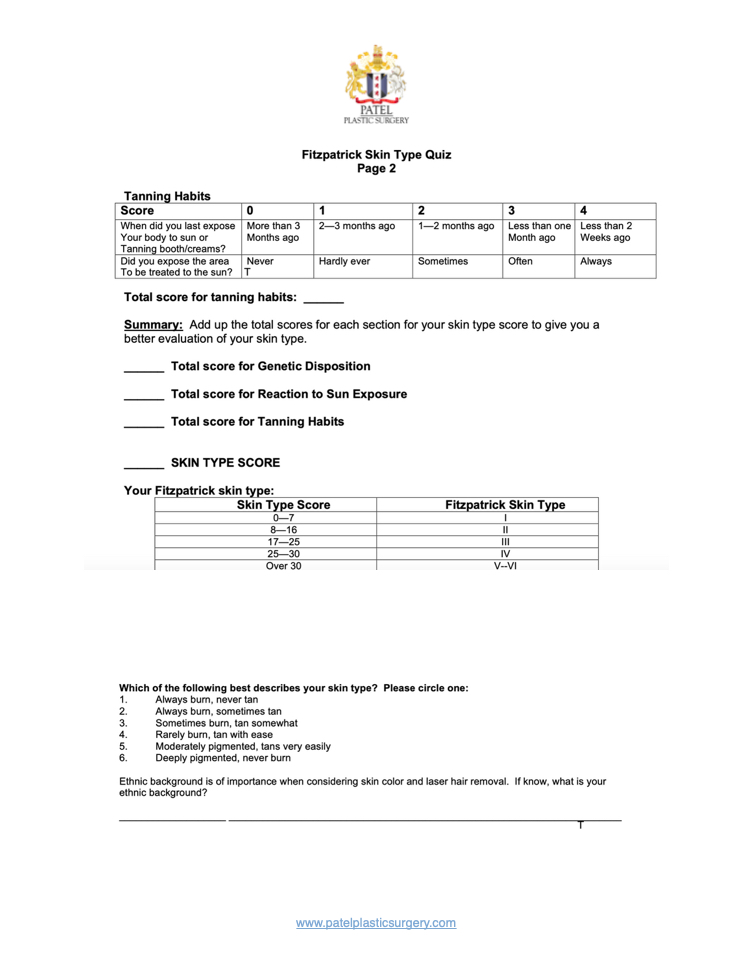
By nature of the criteria, Fitzpatrick's skin type classifications are subjective; however, use of the scale has proven valuable as a diagnostic and therapeutic evaluation tool for many situations. Specifically, these classifications are commonly employed to estimate dosages of particular ultraviolet B (UVB), psoralen with ultraviolet A (PUVA), and laser treatments, as well as to predict skin cancer risk and guide sun protection advice.[3] Though widely used throughout dermatology, plastic surgery, surgical oncology, and other specialties, the Fitzpatrick skin types are not without controversy. Current questions regarding the objective determination, accuracy of self-reporting, and effectiveness in ethnic skin are all major issues of concern with Fitzpatrick skin types. See Images. Fitzpatrick Skin Type Quiz, Questionnaire Pages 1 and 2.
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Objective Determination of Fitzpatrick Skin Types
Given the relative ease of implementation of Fitzpatrick skin typing, it is understandable why this classification system has been so widely applied. However, numerous studies have criticized this system scientifically, and validated objective alternatives have been sought, to achieve a similar outcome of predicting ultraviolet (UV) sensitivity.[4] Methods including the Wood’s lamp for quantification of cutaneous eumelanin and pheomelanin have been implemented; however, both have been unsuccessful in differentiating Fitzpatrick skin types higher than level II.[4]
Currently, spectrophotometers are the primary tool in which melanin density in the epidermis can be estimated and implemented in evaluating the accuracy of self-reported skin types.[4] Spectrophotometers are able to distinguish darkening caused by increased melanin from erythema as a result of inflammation or increased hemoglobin, allowing for a more reliable estimation of the true Fitzpatrick skin type.[5] Spectrophotometers have also been used to distinguish constitutive skin color (baseline skin color in body areas not exposed to light) from facultative skin color (skin color in body areas where light-induced pigmentation changes are seen).[4] Specifically, all 6 Fitzpatrick skin types can be discerned by using a reflectance spectrophotometer along the 450 to 615 nm wavelengths.[4] Unfortunately, this tool is not perfect, and the high costs of both personnel and equipment may prevent the widespread adoption of its use.
Inconsistencies with Self-Reporting and Ethnic Skin
It is important to highlight that the Fitzpatrick skin type is a classification intended to reflect sun sensitivity and not a proxy for racial or phenotypic features. The description of the skin by color – white, brown, black – was meant to denote complexion rather than a self-identification of ethnic origin.[6] For example, a cross-sectional survey of an ethnically diverse population showed self-reported pigmentary phenotypes and race were significant but incomplete predictors of Fitzpatrick skin types.[7]
The difficulty in assessing ethnic skin with the current Fitzpatrick skin type system can be traced to the origin skin types V and VI. When these additional types were created in 1988, the initial intention was to place all black individuals into the type VI category. However, people with mixed heritage or races who identify as black often self-report in a variety of categories, ranging from type IV to type VI.[8] Though the reasons for this are multifaceted, the concept of labeling one’s skin reaction to the sun as tanning or burning lacks reliability, as these words have different meanings to different people. Specifically, participants with a skin of color have been shown not to report painful burns or tanning, or simply not understand the meaning of tanning.[8][9] The functionality of Fitzpatrick skin typing in ethnic skin is also under question. In a population-based study of 2691 participants, this classification system correlated with sun sensitivity in non-Hispanic white and Hispanic participants, but not black participants.[2] In response, multiple scales limited to single ethnic groups have been created, including a Japanese Skin Type scale by Kawada and a scale for individuals of African descent by Willis and Earles, in an attempt to more accurately classify the nuances between ethnic skin.[10]
Laser Therapy in Ethnic Skin
Structural and functional differences between darkly pigmented and lightly pigmented skin are important considerations when performing laser or light-based procedures. In general, darker skin types possess increased epidermal melanin, larger and more widely distributed melanosomes, and reactive fibroblasts.[11] Higher numbered Fitzpatrick skin types are, therefore, associated with these biological characteristics, leading to increased melanin content and epidermal distribution. Increased concentrations of melanin allows for greater protection against ultraviolet radiation, leading to less marked and delayed signs of photoaging.[12]
There are a number of factors to consider when treating individuals with Fitzpatrick skin types IV through VI. Melanin in the epidermis acts as a chromophore, absorbing more laser energy and increasing the risk of adverse events from epidermal injury in those with darkly pigmented skin. To circumvent this risk, longer wavelength lasers are recommended. Deeper penetration of the laser allows for an increased ratio of the temperature of the hair bulb to the temperature of the epidermis, leading to follicular destruction with little epidermal damage.[13] Similarly, lower fluences and longer pulse durations (laser hair removal) or lower treatment densities (laser resurfacing) are suggested for darker-skinned individuals to decrease the risk of thermal injury to the epidermis.[13] Pre- and post-treatment with bleaching agents (for example, hydroquinone cream) has been shown to reduce the risk of post-inflammatory hyperpigmentation, especially after laser resurfacing.[14] Cooling of the epidermis at pre- or post-treatment times can also prevent pigmentary abnormalities, with the most common modalities involving contact or cryogen spray cooling.
With regards to laser or light procedures, the risk of post-procedural hyperpigmentation or hypopigmentation is greater in patients with Fitzpatrick skin types IV through VI. In general, dyschromia is one of the most common reasons why individuals with skin of color visit dermatologists, stemming from their tendency for injury or inflammation to alter pigment production.[15] In addition to the aforementioned recommendations, classification systems such as the Laser Ethnicity Scale have been designed to better predict healing efficacy and times in patients undergoing laser procedures.[16]
Clinical Significance
Fitzpatrick skin types have long been the favored method of classifying an individual’s skin color based on their specific reactions to sun exposure. Clinically, these designations have been employed to estimate dosages, assess cancer risk, or guide counseling (Figures 1 & 2). However, this system has been recognized as ineffectual in certain populations, especially those with darker, non-Caucasian ethnic skin. These individuals are at greater risk of post-procedural pigmentary and scarring-related adverse effects. Thus the accurate determination of Fitzpatrick skin types has important therapeutic consequences. Numerous attempts to create an objective determination of an individual’s skin type have been made; while none are yet considered a gold standard, reflectance spectrophotometers constitute an efficient and noninvasive alternative with a proven record of success.
Nursing, Allied Health, and Interprofessional Team Interventions
While the determination of Fitzpatrick skin types is almost always done by a physician, the administration of laser treatments is a process that may involve many healthcare workers. Physicians, physician assistants, nurse practitioners, nurses, and medical assistants are all involved with laser treatments, and an interprofessional team approach is essential to prevent and/or mitigate pre-, intra-, and post-treatment complications. A detailed education regarding side effects, careful management of expectations, and thorough counseling about results are all essential interprofessional team interventions that will improve outcomes for patients of any Fitzpatrick skin type.[Level 5]
Media
(Click Image to Enlarge)
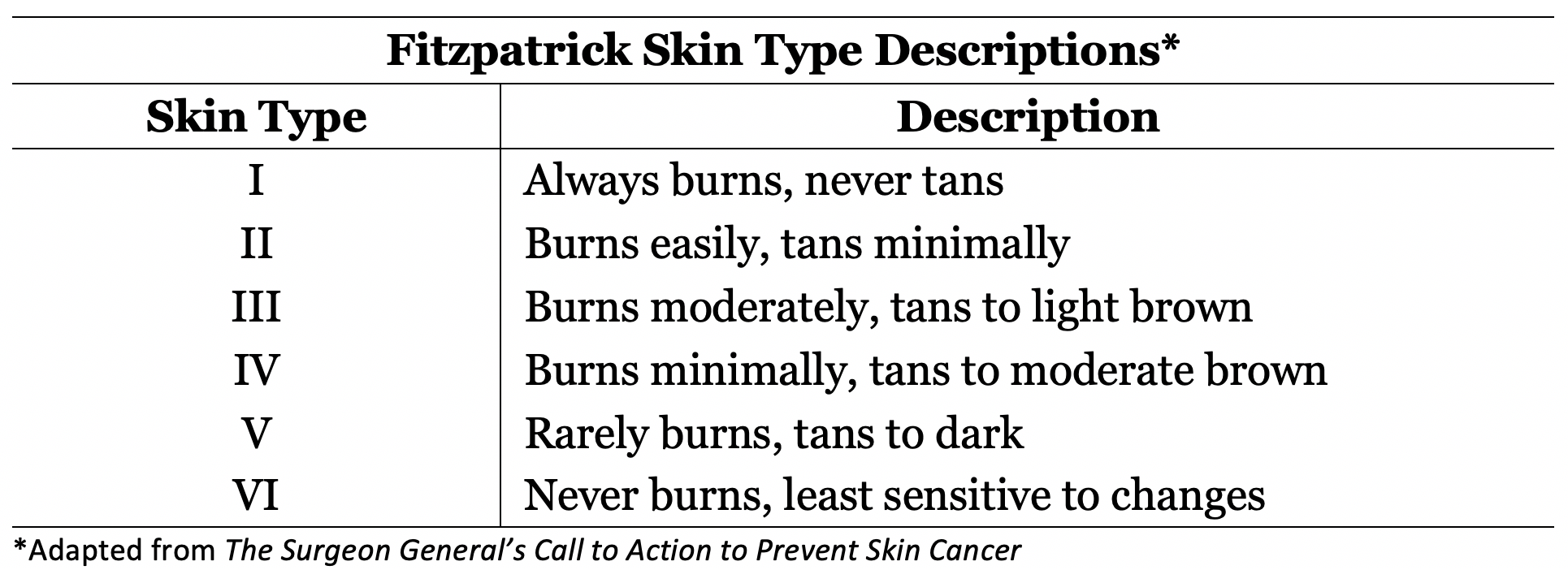
Fitzpatrick Skin Type Descriptions I to VI. The table shows the burning and tanning descriptions for skin types I to VI.
Adapted from the US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2014.
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Archives of dermatology. 1988 Jun:124(6):869-71 [PubMed PMID: 3377516]
Keiser E, Linos E, Kanzler M, Lee W, Sainani KL, Tang JY. Reliability and prevalence of digital image skin types in the United States: results from National Health and Nutrition Examination Survey 2003-2004. Journal of the American Academy of Dermatology. 2012 Jan:66(1):163-5. doi: 10.1016/j.jaad.2011.02.044. Epub [PubMed PMID: 22177642]
Level 3 (low-level) evidenceSachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian journal of dermatology, venereology and leprology. 2009 Jan-Feb:75(1):93-6 [PubMed PMID: 19172048]
Pershing LK, Tirumala VP, Nelson JL, Corlett JL, Lin AG, Meyer LJ, Leachman SA. Reflectance spectrophotometer: the dermatologists' sphygmomanometer for skin phototyping? The Journal of investigative dermatology. 2008 Jul:128(7):1633-40. doi: 10.1038/sj.jid.5701238. Epub 2008 Jan 17 [PubMed PMID: 18200057]
Barsh GS. What controls variation in human skin color? PLoS biology. 2003 Oct:1(1):E27 [PubMed PMID: 14551921]
Amblard P, Beani J, Gautron R, Reymond J, Doyon B. Statistical study of individual variations in sunburn sensitivity in 303 volunteers without photodermatosis. Archives of dermatological research. 1982:274(3-4):195-206 [PubMed PMID: 7165371]
He SY, McCulloch CE, Boscardin WJ, Chren MM, Linos E, Arron ST. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. Journal of the American Academy of Dermatology. 2014 Oct:71(4):731-7. doi: 10.1016/j.jaad.2014.05.023. Epub 2014 Jun 11 [PubMed PMID: 24928709]
Level 2 (mid-level) evidenceEilers S, Bach DQ, Gaber R, Blatt H, Guevara Y, Nitsche K, Kundu RV, Robinson JK. Accuracy of self-report in assessing Fitzpatrick skin phototypes I through VI. JAMA dermatology. 2013 Nov:149(11):1289-94. doi: 10.1001/jamadermatol.2013.6101. Epub [PubMed PMID: 24048361]
Level 2 (mid-level) evidenceRobinson JK, Joshi KM, Ortiz S, Kundu RV. Melanoma knowledge, perception, and awareness in ethnic minorities in Chicago: recommendations regarding education. Psycho-oncology. 2011 Mar:20(3):313-20. doi: 10.1002/pon.1736. Epub [PubMed PMID: 20878831]
Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photo-dermatology. 1986 Dec:3(6):327-33 [PubMed PMID: 3588352]
Alexis AF. Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. The British journal of dermatology. 2013 Oct:169 Suppl 3():91-7. doi: 10.1111/bjd.12526. Epub [PubMed PMID: 24098905]
Alexis AF, Alam M. Racial and ethnic differences in skin aging: implications for treatment with soft tissue fillers. Journal of drugs in dermatology : JDD. 2012 Aug:11(8):s30-2; discussion s32 [PubMed PMID: 22859226]
Level 3 (low-level) evidenceRoss EV, Cooke LM, Timko AL, Overstreet KA, Graham BS, Barnette DJ. Treatment of pseudofolliculitis barbae in skin types IV, V, and VI with a long-pulsed neodymium:yttrium aluminum garnet laser. Journal of the American Academy of Dermatology. 2002 Aug:47(2):263-70 [PubMed PMID: 12140474]
Alajlan AM, Alsuwaidan SN. Acne scars in ethnic skin treated with both non-ablative fractional 1,550 nm and ablative fractional CO2 lasers: comparative retrospective analysis with recommended guidelines. Lasers in surgery and medicine. 2011 Sep:43(8):787-91. doi: 10.1002/lsm.21092. Epub [PubMed PMID: 21956625]
Level 2 (mid-level) evidenceAlexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007 Nov:80(5):387-94 [PubMed PMID: 18189024]
Level 2 (mid-level) evidenceLancer HA. Lancer Ethnicity Scale (LES). Lasers in surgery and medicine. 1998:22(1):9 [PubMed PMID: 9443143]
Level 3 (low-level) evidence