Anatomy, Bony Pelvis and Lower Limb: Lateral Femoral Cutaneous Nerve
Anatomy, Bony Pelvis and Lower Limb: Lateral Femoral Cutaneous Nerve
Introduction
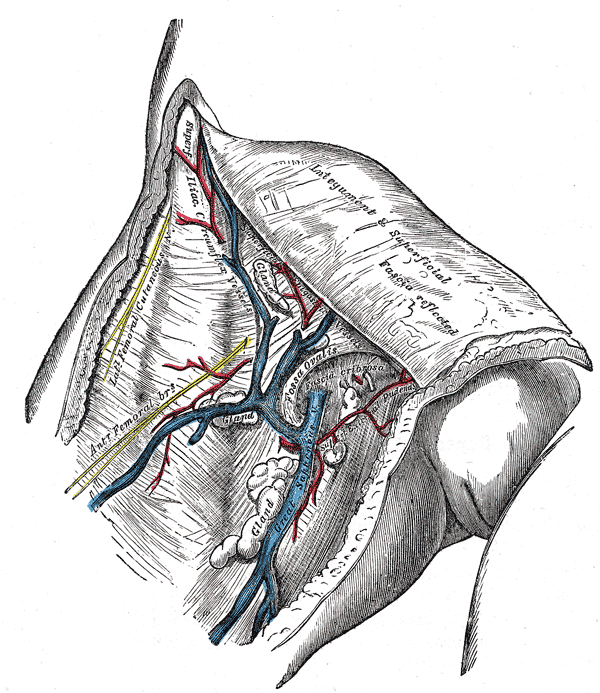
Many nerves of the lumbar plexus provide sensation to the thigh, including the lateral femoral cutaneous nerve (LFCN). The lateral femoral cutaneous nerve is usually derived from the dorsal branches of the L2 and L3 ventral rami. It appears from under the lateral border of the psoas major and travels towards the notch on the anterior superior iliac spine (ASIS), exiting the lesser pelvis by passing under the inguinal ligament. The lateral femoral cutaneous nerve branches into anterior and posterior divisions and provides sensation to the anterolateral and lateral thigh, respectively. The pathology associated with the lateral femoral cutaneous nerve is meralgia paresthetica, also known as Bernhardt-Roth syndrome, which is characterized by loss of sensation on the anterolateral and lateral thigh and has numerous etiologies, including obesity, diabetes, and tight clothing.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The lateral femoral cutaneous nerve exclusively carries afferent sensory fibers. Most commonly, the lateral femoral cutaneous nerve is formed from the L2 and L3 nerve roots. It first appears at the lateral border of the psoas major, then moves parallel to the iliac crest and in an oblique fashion across the iliacus muscle toward the anterior superior iliac spine. Here, the lateral femoral cutaneous nerve branches into a left and a right nerve. The left branch of the LFCN dives behind the lower descending colon and provides sensation to the parietal peritoneum in the iliac fossa. The right branch passes posterolateral to the cecum behind the fascia iliaca, outside the peritoneum. The left and right branches both run underneath the inguinal ligament, anterior to, through, or posterior to the sartorius muscle and 10 mm medial to ASIS and into the thigh. Once distal to the inguinal ligament, the lateral femoral cutaneous nerve branches into anterior and posterior divisions. The anterior branch exits the fascia lata more distally than the posterior branch and provides sensation to the anterolateral thigh as distally as the knee. It also forms part of the peripatellar plexus along with the anterior division of the femoral nerve and the infrapatellar branch of the saphenous nerve. The posterior division provides sensation to the skin of the lateral thigh, covering the area from the greater trochanter (and sometimes the gluteal skin) to half-way down the thigh. Meralgia paresthetica is more commonly seen in the distribution of the anterior division than the posterior division, although both may be affected.[2][3]
Physiologic Variants
The anatomy of the lateral femoral cutaneous nerve is commonly variable. The nerve has been noted exiting the pelvis in seven different locations in relation to the inguinal ligament and ASIS. It most commonly exits medial to ASIS and under the inguinal ligament but has also been seen exiting the pelvis medial to ASIS and superior to the inguinal ligament. The LFCN may also exit superior to ASIS itself or even lateral to ASIS. Occasionally, the lateral femoral cutaneous nerve passes through ASIS, the inguinal ligament, or sartorius; however, it can be found medial to the sartorius 86% of the time. The distance from the nerve to ASIS is also highly variable, creating a zone in which the LFCN might be found, ranging from 10 mm (most common) to 46 mm medially. The bifurcation pattern of the lateral femoral cutaneous nerve is also highly variable. The nerve may bifurcate in the thigh (most common), in the pelvis, near the exit to the pelvis, or the LFCN may trifurcate or quadrificate.[4]
Most commonly, the lateral femoral cutaneous nerve originates directly from L2-L3 nerve roots in the lumbar plexus, but it has also been noted to arise from L1 and L2, or L3 and L4. It may form as a collateral branch of the femoral nerve, or it might be absent altogether, and sensation to the anterolateral thigh is replaced by the ilioinguinal nerve, a branch of the anterior femoral cutaneous nerve, or a branch of the genitofemoral nerve.[3][2]
Surgical Considerations
Many surgical procedures can lead to iatrogenic nerve injury, especially for anatomical variants involving early bifurcation, as this can lead to more nerve divisions of which to be mindful. Inguinal hernia repair is one such surgery where the variations in the anatomy of the LFCN can lead to iatrogenic injury. During laparoscopic inguinal hernia repair, the incidence of nerve injury is approximately 2%. This nerve is also at risk of injury during aesthetic abdominoplasties, and it is suggested to approach the 4 cm area surround ASIS with careful dissection to avoid iatrogenic injury of the lateral femoral cutaneous nerve. During bone graft harvesting, the LFCN is also at potential risk, as the size of the bone graft and incision can increase the likelihood of nerve injury and lead to the recommendation to keep incisions at least 3 cm away from ASIS.
Another procedure where the location of the LFCN is of particular interest is bone graft harvesting. Factors such as the size of the graft and size of the incision can greatly influence the risk of injury. The current suggestions are that the grafts should be less than 3 cm in size and that the incisions should be at least 3 cm or more away from the palpable point of the ASIS. The anterior approach in hip arthroplasty is superior to the posterior approach, as it lowers the risk of dislocation and provides less risk to the hip adductors; however, the risk to the LFCN is greater, with 81% of patients undergoing an anterior hip arthroplasty report new onset neurapraxia in the distribution of the LFCN. The current standard of practice to avoid LFCN damage suggests that incisions are made parallel to the LCFN.[1] One method to avoid lateral femoral cutaneous nerve damage is to use ultrasound guidance as a tool to visualize the nerve and ensure its safety during these surgical procedures.[5]
Clinical Significance
The lateral femoral cutaneous nerve is subject to injury from many sources, and this injury leads to meralgia paresthetica, the loss of sensation in the distribution of the LFCN, often accompanied by swelling and neuroma formation. In patients with diabetes mellitus, the incidence of meralgia paresthetica has been reported as 247 out of 100,000 people, which is five times the incidence of the general population.[6]
Injury is usually the result of external compression or trauma near ASIS, the nerve’s most vulnerable point. The most common culprit of impingement is underneath the inguinal ligament, which can develop both spontaneously or after injury.[7] Some common mechanisms of external compression include wearing a seatbelt or wearing pants that are too tight. Carrying a cell phone, wallet, or gun on the hip has also been implicated.(8) Obesity and pregnancy can also cause external compression due to pannus formation.[6] In dancers, the Sartorius is often the culprit of compression during positions requiring the leg to be turned out. Scar formation may also result in nerve compression.[7]
Media
(Click Image to Enlarge)
References
Tomaszewski KA, Popieluszko P, Henry BM, Roy J, Sanna B, Kijek MR, Walocha JA. The surgical anatomy of the lateral femoral cutaneous nerve in the inguinal region: a meta-analysis. Hernia : the journal of hernias and abdominal wall surgery. 2016 Oct:20(5):649-57. doi: 10.1007/s10029-016-1493-7. Epub 2016 Apr 26 [PubMed PMID: 27115766]
Level 1 (high-level) evidenceCarai A, Fenu G, Sechi E, Crotti FM, Montella A. Anatomical variability of the lateral femoral cutaneous nerve: findings from a surgical series. Clinical anatomy (New York, N.Y.). 2009 Apr:22(3):365-70. doi: 10.1002/ca.20766. Epub [PubMed PMID: 19173255]
Level 2 (mid-level) evidenceDibenedetto LM, Lei Q, Gilroy AM, Hermey DC, Marks SC Jr, Page DW. Variations in the inferior pelvic pathway of the lateral femoral cutaneous nerve: implications for laparoscopic hernia repair. Clinical anatomy (New York, N.Y.). 1996:9(4):232-6 [PubMed PMID: 8793216]
Kosiyatrakul A, Nuansalee N, Luenam S, Koonchornboon T, Prachaporn S. The anatomical variation of the lateral femoral cutaneous nerve in relation to the anterior superior iliac spine and the iliac crest. Musculoskeletal surgery. 2010 May:94(1):17-20. doi: 10.1007/s12306-010-0054-y. Epub 2010 Feb 5 [PubMed PMID: 20135245]
Ozaki Y, Baba T, Homma Y, Tanabe H, Ochi H, Bannno S, Watari T, Kaneko K. Preoperative ultrasound to identify distribution of the lateral femoral cutaneous nerve in total hip arthroplasty using the direct anterior approach. SICOT-J. 2018:4():42. doi: 10.1051/sicotj/2018037. Epub 2018 Sep 17 [PubMed PMID: 30222102]
Weng WC, Wei YC, Huang WY, Chien YY, Peng TI, Wu CL. Risk factor analysis for meralgia paresthetica: A hospital-based study in Taiwan. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2017 Sep:43():192-195. doi: 10.1016/j.jocn.2017.04.024. Epub 2017 May 13 [PubMed PMID: 28511974]
Schwaiger K, Panzenbeck P, Purschke M, Russe E, Kaplan R, Heinrich K, Mandal P, Wechselberger G. Surgical decompression of the lateral femoral cutaneous nerve (LFCN) for Meralgia paresthetica treatment: Experimental or state of the art? A single-center outcome analysis. Medicine. 2018 Aug:97(33):e11914. doi: 10.1097/MD.0000000000011914. Epub [PubMed PMID: 30113491]