Introduction
Spondylolysis refers to a posterior defect of the vertebral body occurring at the pars interarticularis.[1] Typically, this defect results from trauma or chronic repetitive loading and hyperextension. If this instability leads to translation of the vertebral body, this is spondylolisthesis.[1][2] This process requires either a fracture or deformation of the posterior spinal elements resulting in elongation of the pars interarticularis. This condition can potentially occur in all age groups, with the underlying cause varying based on age. If the slip progresses to the point of neurologic compromise, then surgical intervention may be necessary to decompress and stabilize affected segments.[3] Absent any motor deficits, a nonoperative course of analgesia, activity modification, and injections should be the initial therapeutic approach for several months.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Isthmic spondylolisthesis refers to a defect within the pars interarticularis usually from repetitive microtrauma and accounts for the vast majority of cases in children and adolescents.[1][5]
Degenerative spondylolisthesis is the most common form of spondylolisthesis seen in adults.[6] It is due to chronic degenerative changes at the posterior elements resulting in the incompetence of the surrounding ligamentous structures, leading to elongation and slippage.[6]
Acutely, a traumatic spondylolisthesis can occur following a high-energy injury flexion/extension that causes a fracture-dislocation at the posterior elements.[7]
Another type is dysplastic spondylolisthesis which is a result of an abnormal formation of the posterior elements resulting in this subsequent instability.[8]
Epidemiology
The rates of spondylosis and spondylolisthesis vary widely by age group. In the pediatric population, spondylosis is present in about 5% of the population, most commonly (90%) at the L5 to S1 motion segment, although pathology at L4 is more likely to be symptomatic.[1][9] Long-term studies estimate that about 15% of those with a defect (spondylosis) will develop a slip (spondylolisthesis).[10][11] Regarding adults, lumbar spondylolisthesis without a defect in the pars is present in 5% of men, 10% of women.[12] It is not always symptomatic. This degenerative type usually occurs at the L4 to L5 levels (versus isthmic noted at L5 to S1).[6] Degenerative spondylolisthesis is an acquired type of spondylolisthesis occurring much more frequently and gradually in the adult population.[6] Cohorts with degenerative spondylolisthesis will rarely develop a high-grade spondylolisthesis.[13] Furthermore, the chronic natural history of this disease process is such that with further degenerative changes, the vertebral segments may eventually stabilize, and the patients can have subsequent clinical improvements.[13]
Pathophysiology
Repetitive micro-traumas from hyperextension lead to elongated or absent pars interarticularis. This force applies additional stress to the facet joints and subsequent hypermobility leading to advanced degeneration of the disc space.[14] The reduced disc and facet stability results in the translation of the vertebral body, creating a stenotic effect on the exiting nerve roots and/or the spinal canal. In the traumatic setting, flexion-distraction energy may cause a localized vertebral body failure at this segment, predisposing the patient to chronic issues if instability develops.
History and Physical
Initial evaluation of lower back pain initiates by obtaining a history from the patient. This history should pertain to the timeline of pain, radiation of pain, and inciting events. The clinician should pay careful attention to prior episodes of trauma. Low-grade slips and stenotic spinal canals may decompress and relieve pain with leaning forward or sitting. It is crucial to note patient comments such as decreased pain with pushing a grocery cart or walking upstairs as both common actions have the spinal column in forwarding flexion.[15] It is also important in any evaluation of extremity issues to inspect circulation as vascular claudication may mirror or mimic the neurogenic problems.
Classically patients may complain of pain radiating down both buttocks and lower extremities. An evaluation of the patient's walking is also critical to better assess the daily impact that pain or neurological deficits cause. All physical examinations will include assessing the neurologic function of the arms, legs, bladder, and bowels. The keys to a thorough exam are organization and patience. One should evaluate not only strength but also sensation and reflexes. It is also essential to inspect the skin along the back and document the presence of tenderness to compression or palpable step-off.
Performing a straight leg test in a patient positioned supine may also reveal a stenotic canal.[16] This test may also cause local sites of pain as hamstring contractures are often associated with spondylolisthesis.[17] As mentioned above, a thorough neurologic examination is required. Commonly a patient will have L5 radiculopathy resulting in weakness of ankle dorsiflexion and extension of the great toe. This deficit may also diminish the Achilles tendon reflex. L4 radiculopathy may present with weakness at the quadriceps and a decreased patellar tendon reflex.
Documentation is paramount as these initial findings will likely serve as a baseline for all future evaluations.
Evaluation
Evaluation of patients with low-back pain typically includes anterior-posterior (AP) and lateral radiographs of the impacted area. Some physicians will obtain radiographs of the entire spine. A key component to radiographic evaluation is obtaining flexion/extension films, which illustrates vertebral segment stability.[18] Serial standing lateral radiographs obtained in the clinic will help track any potential progression of the slip.
One of the crucial measurements to note regarding slips is the amount of translation between vertebral bodies. The amount of “uncovering” of one endplate from the other determines the grade. There are four grades of spondylolisthesis: Grade 1: 0% to 25%, Grade 2: 26% to 50%, Grade 3: 51% to 75% and Grade 4: 76% to 99%.[12][19] At 100% displacement, patients have developed spondyloptosis.[20] Grades 1 and 2 are considered low-grade slips.[21] Grades 3 and 4 are considered high-grade spondylolisthesis.[19]
An MRI is critical when evaluating patients with suspected spondylosis and spondylolisthesis. Frequently these patients will initially trail a six-week course of physical therapy. Upon follow-up, if the symptomology is still present, the clinician can obtain an MRI at that time.[1] The focus should be on the T2 weighted sagittal and axial images, as these will illustrate any compression of neurologic elements.
Treatment / Management
Non-surgical intervention includes modification of the activity that may have exacerbated the pain, non-steroidal anti-inflammatory medications (NSAIDs), physical therapy, stretching, and occasionally using a lumbosacral orthosis. A 2009 meta-analysis evaluating spondylolysis and grade 1 spondylolisthesis showed almost 84% of adolescent patients treated nonoperatively had a successful clinical outcome at one year.[22] This study also showed no difference in those who did and did not use a brace.[22] Likely it is the activity restriction and not bracing, which determines the overall outcome. Additionally, a course of at least six weeks of physical therapy with an emphasis on core exercise strengthening and stretching should be attempted. Additionally, temporary pain relief is possible with epidural injections, but the potential for subsequent infection risk, while low, is possible.[23][24] (A1)
While most patients improve with nonoperative treatment alone, those failing a conservative treatment course have three options- continued pain, complete avoidance of activities that elicit pain, or surgical intervention. Again, the surgical options for spondylolysis (as well as low-grade spondylolisthesis) should be reserved for those with either neurologic deficits, the progression of a slip, or pain limiting daily functions.[3] The literature regarding the optimal surgical procedure, approach, and roles for decompression and instrumentation remains controversial. While there is still controversy regarding the need for posterior decompression for patients who have just radicular symptoms, what is agreed upon is the need for decompression when a true motor deficit is present.[3][11][25] Additionally, in the setting of retrolisthesis and disc herniation at L5-S1, recent long-term follow-up from the SPORT database has shown non-inferior outcomes in patients with surgically treated disc herniations in the setting of retrolisthesis.[26] The patient needs to understand that while surgical intervention has favorable outcomes for relieving radicular pains, the results are less predictable for non-radiating lower back pain.
Differential Diagnosis
- Lumbosacral disc injuries
- Lumbosacral discogenic pain syndrome
- Lumbosacral facet syndrome
- Lumbosacral spine acute bony injuries
- Lumbosacral spine sprain/strain injuries
- Lumbosacral spondylolisthesis
- Lumbosacral spondylosis
- Myofascial pain in athletes
- Sacroiliac joint injury
Prognosis
The prognosis for patients with spondylolisthesis is generally good. Most patients will respond to conservative treatment. For those with ongoing, severe symptoms not relieved by conservative approaches, surgery can potentially relieve radicular leg symptoms by decompressing nerve roots. Localized lumbar pain may require lumbar fusion in more extreme cases.[27][28]
Complications
Complications of spondylolisthesis tend to be neurological. These can include chronic pain in the lower back or legs, and numbness, tingling, or weakness in the lower extremities. Severe nerve compression can lead to problems with bowel or bladder control; however, this is quite uncommon.[27]
Deterrence and Patient Education
Patients will need to understand their condition and its imposed limitations based on the severity of their particular case. The clinician should review the relevant anatomy and explain the disruption, using spinal models if necessary. A review of the patient's activities and physical demands is prudent (e.g., heavy lifting, prolonged sitting, etc.). Based on the severity of the condition, the clinician may impose physical limitations.
Pearls and Other Issues
Many patients will improve with a nonoperative treatment course directed at activity modification.[22] Patients should understand that surgery frequently will not relieve all pain as irreversible damage to the nerves may have already occurred. The future of minimally invasive treatment options will continue to perfect outcomes for spinal stenosis. Advancements in pain control and endoscopic technologies now allow for select patients and facilities to perform endoscopic disc debridement followed by percutaneous instrumentation on an outpatient basis. Additional research will focus on optimizing treatment outcomes and predicting which patients will develop symptomatic progression of a slip.
Enhancing Healthcare Team Outcomes
Patients with low back pain are best managed by an interprofessional team that includes the emergency department physician, therapist, orthopedic nurse, primary care physician, an orthopedic surgeon. The initial treatment for low back pain is non-surgical and involves a change in lifestyle. Most patients can benefit from exercise, weight loss, and leading an active lifestyle. Surgery is only a recommendation when there is nerve compression, or the patient has failed conservative treatment. The patient must understand that surgery is not always effective, and many patients still experience residual pain and limited range of motion of the lumbar spine. The patient needs to understand that while surgical intervention has favorable outcomes for relieving radicular pains, the results are less predictable for non-radiating lower back pain.
Media
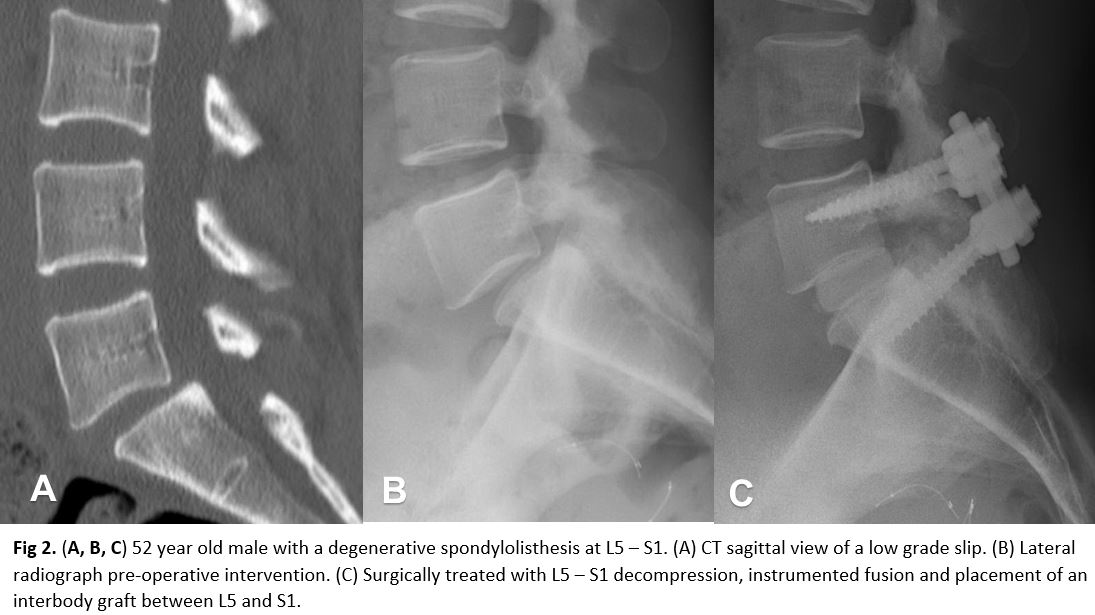
(Click Image to Enlarge)
(Click Image to Enlarge)
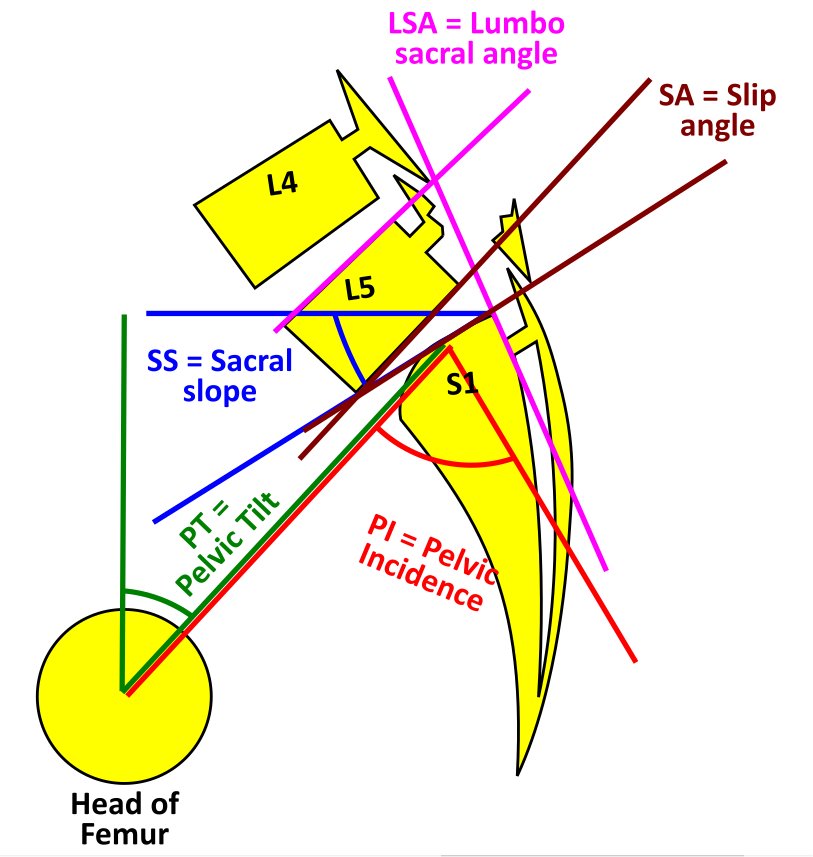
Spondylolysis with Spondylolisthesis, showing spino pelvic parameters, slip, dysplasia of upper endplate of S1, Slip angle (SA = angle between inferior endplate of L5 and line perpendicular to the S1 posterior wall) and lumbo sacral angle (LSA = angle between the superior endplate of L5 and posterior wall of the S1). Contributed by George Ampat FRCS
References
Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. The Journal of the American Academy of Orthopaedic Surgeons. 2006 Jul:14(7):417-24 [PubMed PMID: 16822889]
Foreman P, Griessenauer CJ, Watanabe K, Conklin M, Shoja MM, Rozzelle CJ, Loukas M, Tubbs RS. L5 spondylolysis/spondylolisthesis: a comprehensive review with an anatomic focus. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2013 Feb:29(2):209-16. doi: 10.1007/s00381-012-1942-2. Epub 2012 Oct 23 [PubMed PMID: 23089935]
Level 3 (low-level) evidenceCheung EV, Herman MJ, Cavalier R, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. The Journal of the American Academy of Orthopaedic Surgeons. 2006 Aug:14(8):488-98 [PubMed PMID: 16885480]
Herman MJ, Pizzutillo PD, Cavalier R. Spondylolysis and spondylolisthesis in the child and adolescent athlete. The Orthopedic clinics of North America. 2003 Jul:34(3):461-7, vii [PubMed PMID: 12974495]
Jones TR, Rao RD. Adult isthmic spondylolisthesis. The Journal of the American Academy of Orthopaedic Surgeons. 2009 Oct:17(10):609-17 [PubMed PMID: 19794218]
Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. The Journal of the American Academy of Orthopaedic Surgeons. 2014 Apr:22(4):203-13. doi: 10.5435/JAAOS-22-04-203. Epub [PubMed PMID: 24668350]
Ibebuike K, Roussot M, Watt J, Dunn R. Management challenges of traumatic spondylolisthesis of the Axis with an unusual C2-C3 posterior subluxation in a paediatric patient: case report and literature review. African health sciences. 2018 Jun:18(2):458-467. doi: 10.4314/ahs.v18i2.31. Epub [PubMed PMID: 30602973]
Level 3 (low-level) evidenceBoxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. The Journal of bone and joint surgery. American volume. 1979 Jun:61(4):479-95 [PubMed PMID: 438234]
Saraste H. Long-term clinical and radiological follow-up of spondylolysis and spondylolisthesis. Journal of pediatric orthopedics. 1987 Nov-Dec:7(6):631-8 [PubMed PMID: 2963019]
Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine. 2009 Jan 15:34(2):199-205. doi: 10.1097/BRS.0b013e31818edcfd. Epub [PubMed PMID: 19139672]
Level 2 (mid-level) evidenceOmidi-Kashani F, Ebrahimzadeh MH, Salari S. Lumbar spondylolysis and spondylolytic spondylolisthesis: who should be have surgery? An algorithmic approach. Asian spine journal. 2014 Dec:8(6):856-63. doi: 10.4184/asj.2014.8.6.856. Epub 2014 Dec 17 [PubMed PMID: 25558333]
Bouras T, Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2015 Jul:25 Suppl 1():S167-75. doi: 10.1007/s00590-014-1560-7. Epub 2014 Nov 14 [PubMed PMID: 25394940]
Schulte TL, Ringel F, Quante M, Eicker SO, Muche-Borowski C, Kothe R. Surgery for adult spondylolisthesis: a systematic review of the evidence. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Aug:25(8):2359-67. doi: 10.1007/s00586-015-4177-6. Epub 2015 Sep 12 [PubMed PMID: 26363561]
Level 1 (high-level) evidenceShah SA, Saller J. Evaluation and Diagnosis of Back Pain in Children and Adolescents. The Journal of the American Academy of Orthopaedic Surgeons. 2016 Jan:24(1):37-45. doi: 10.5435/JAAOS-D-14-00130. Epub [PubMed PMID: 26589458]
Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010 Jan:14(1):17-21 [PubMed PMID: 20411054]
Scaia V, Baxter D, Cook C. The pain provocation-based straight leg raise test for diagnosis of lumbar disc herniation, lumbar radiculopathy, and/or sciatica: a systematic review of clinical utility. Journal of back and musculoskeletal rehabilitation. 2012:25(4):215-23. doi: 10.3233/BMR-2012-0339. Epub [PubMed PMID: 23220802]
Level 1 (high-level) evidenceMiyamoto N, Hirata K, Kimura N, Miyamoto-Mikami E. Contributions of Hamstring Stiffness to Straight-Leg-Raise and Sit-and-Reach Test Scores. International journal of sports medicine. 2018 Feb:39(2):110-114. doi: 10.1055/s-0043-117411. Epub 2017 Nov 30 [PubMed PMID: 29190853]
Chen X, Zhou QS, Xu L, Chen ZH, Zhu ZZ, Li S, Qiu Y, Sun X. Does kyphotic configuration on upright lateral radiograph correlate with instability in patients with degenerative lumbar spondylolisthesis? Clinical neurology and neurosurgery. 2018 Oct:173():96-100. doi: 10.1016/j.clineuro.2018.07.020. Epub 2018 Jul 30 [PubMed PMID: 30096570]
Level 2 (mid-level) evidenceHarris IE, Weinstein SL. Long-term follow-up of patients with grade-III and IV spondylolisthesis. Treatment with and without posterior fusion. The Journal of bone and joint surgery. American volume. 1987 Sep:69(7):960-9 [PubMed PMID: 3654708]
Mishra A, Agrawal D, Gupta D, Sinha S, Satyarthee GD, Singh PK. Traumatic spondyloptosis: a series of 20 patients. Journal of neurosurgery. Spine. 2015 Jun:22(6):647-52. doi: 10.3171/2014.10.SPINE1440. Epub 2015 Mar 13 [PubMed PMID: 25768668]
Level 2 (mid-level) evidenceEvans N, McCarthy M. Management of symptomatic degenerative low-grade lumbar spondylolisthesis. EFORT open reviews. 2018 Dec:3(12):620-631. doi: 10.1302/2058-5241.3.180020. Epub 2018 Dec 19 [PubMed PMID: 30697442]
Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. Journal of pediatric orthopedics. 2009 Mar:29(2):146-56. doi: 10.1097/BPO.0b013e3181977fc5. Epub [PubMed PMID: 19352240]
Level 1 (high-level) evidenceDonnally CJ 3rd, Rush AJ 3rd, Rivera S, Vakharia RM, Vakharia AM, Massel DH, Eismont FJ. An epidural steroid injection in the 6 months preceding a lumbar decompression without fusion predisposes patients to post-operative infections. Journal of spine surgery (Hong Kong). 2018 Sep:4(3):529-533. doi: 10.21037/jss.2018.09.05. Epub [PubMed PMID: 30547115]
Ilyas H, Udo-Inyang I Jr, Savage J. Lumbar Spinal Stenosis and Degenerative Spondylolisthesis: A Review of the SPORT Literature. Clinical spine surgery. 2019 Aug:32(7):272-278. doi: 10.1097/BSD.0000000000000841. Epub [PubMed PMID: 31145150]
Donnally CJ 3rd, Madhavan K, Butler AJ, Sheu JI, Massel DH, Green BA, Gjolaj JP. A novel technique for stabilization of high-grade spondylolisthesis with transvertebral fusion without reduction. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Feb:60():170-175. doi: 10.1016/j.jocn.2018.11.001. Epub 2018 Nov 22 [PubMed PMID: 30470650]
Shenoy K, Stekas N, Donnally CJ 3rd, Zhao W, Kim YH, Lurie JD, Razi AE. Retrolisthesis and lumbar disc herniation: a postoperative assessment of outcomes at 8-year follow-up. The spine journal : official journal of the North American Spine Society. 2019 Jun:19(6):995-1000. doi: 10.1016/j.spinee.2018.12.010. Epub 2018 Dec 27 [PubMed PMID: 30594668]
Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. StatPearls. 2023 Jan:(): [PubMed PMID: 32809514]
Austevoll IM, Gjestad R, Solberg T, Storheim K, Brox JI, Hermansen E, Rekeland F, Indrekvam K, Hellum C. Comparative Effectiveness of Microdecompression Alone vs Decompression Plus Instrumented Fusion in Lumbar Degenerative Spondylolisthesis. JAMA network open. 2020 Sep 1:3(9):e2015015. doi: 10.1001/jamanetworkopen.2020.15015. Epub 2020 Sep 1 [PubMed PMID: 32910195]
Level 2 (mid-level) evidence