Introduction
Lymphocytosis, defined by an increase in absolute lymphocyte count (ALC) to more than 4000 lymphocytes/microL in adult patients, is a common hematologic abnormality. ALC calculates as the total white blood cell count (WBC) multiplied by the percentage of lymphocytes in the peripheral blood. Different lymphocyte subsets (T cells, B cells, or NK cells) may be increased depending on the particular etiology. Lymphocytes represent around 20 to 40% of WBC. The definition of relative lymphocytosis is an increase in WBC of more than 40% in the presence of a normal absolute white cell count. In this review, we present the most common causes in adult patients, in addition to a general approach to diagnosis and management of frequently encountered etiologies.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Distinguishing reactive from malignant lymphocytosis can be challenging and may vary depending on age and other demographics. The following is a list of the most common etiologies.
- Infectious:
- Viral infections:
- Epstein-Barr Virus (EBV): Infectious Mononucleosis (IM) is a classic example of viral infections associated with lymphocytosis. Acute IM is a disease characterized by fever, lymphadenopathy, pharyngitis, splenomegaly, and various hematologic manifestations, among which lymphocytosis is the most common and presents in up to two-thirds of cases.[1]
- Cytomegalovirus (CMV): CMV can cause a disease indistinguishable from EBV IM.
- Human Immunodeficiency Virus (HIV): Although chronic HIV infection resulted in lymphopenia and decreased CD4+ lymphocytes count, primary HIV infection can lead to an acute febrile mononucleosis-like illness with associated lymphocytosis. A negative heterophile test can help distinguish the two.[2]
- Other Viruses: Influenza, hepatitis, mumps, measles, rubella, and human T Lymphocytic virus type 1 (HTLV-1), adenovirus, to name a few.
- Bacterial Infections: Most of the acute bacterial infections will cause neutrophilia; however, notable exceptions include:
- Bartonella henselae: Bartonella henselae leads to cat scratch disease, a disease transmitted by scratch or bite from an infected cat, that leads mostly to self-limited lymphadenopathy, but can be associated with ocular or neurologic manifestations. Lymphocytes are large and atypical.
- Bordetella Pertussis: Pertussis is characterized by increased lymphocytes that are small with a deeply cleaved nucleus, clinical correlation is needed to differentiate from some lymphoid malignancies that might share the morphologic appearance.
- Other: Brucellosis, syphilis, malaria
- Parasitic Infections:
- Toxoplasma Gondii: symptomatic toxoplasmosis occurs most commonly in immunocompromised hosts. Lymphocytosis with atypical lymphocytes is a hematologic hallmark of the disease, that can present as a mononucleosis-like illness.[3]
- Other: Babesiosis
- Mycobacterial Tuberculosis
- Viral infections:
- Lymphoproliferative disorders: Lymphocytes tend to be monomorphic in malignant causes in contradiction to the pleomorphic lymphocytes in reactive causes. Some common etiologies are listed here:
- Chronic Lymphocytic Leukemia (CLL): CLL is the most common leukemia in adult patients in the USA. Lymphocytes are over 5000 cells/microL per definition and are typically small mature looking with dense nuclei and compact chromatin, also called "soccer ball" cells. Numerous smudge cells resulting from damage during the preparation of peripheral blood smear slide are characteristic of patients diagnosed with CLL.
- Non-Hodgkin Lymphoma (NHL): Bone marrow can have involvement in around 30% of cases, and peripheral blood lymphocytosis varies between different types.[4] Lymphoma cells can have different sizes or shapes depending on the lymphoma type.[5] The following are some examples of NHL associated with lymphocytosis:
- Mantle cell lymphoma (MCL): MCL is an uncommon NHL; however, it frequently correlates with lymphocytosis.[4][6] The cells of the blastoid variant of MCL are typically large with a moderate amount of cytoplasm and indented nuclei.[5]
- Marginal Zone Lymphoma (MZL): The lymphocytosis is associated with anemia and thrombocytopenia. Typical lymphocytes in MZL have villous cytoplasmic projections.
- Hairy Cell Leukemia: "hairy cells" have regular cytoplasmic projections through the entire periphery of the cell that may resemble "villous" cells; however, typical immunophenotype is different (discussed below).
- Follicular Lymphoma (FL): FL cells are larger than typical normal lymphocytes but smaller than MCL cells. "Cleaved" lymphocytosis can occur, which refers to the cleft appearing nuclei. Other disorders with angulated or cleaved lymphocytes include pertussis and MCL as above in addition to Sezary Syndrome and Adult T cell lymphoma/leukemia (ATLL).[4]
- Sezary Syndrome: It represents the leukemic phase of cutaneous T cell lymphoma. Characteristic Sezary cells have cribriform nuclei with compact chromatin.
- ATLL: this is aggressive leukemia caused by HTLV-1. It is common in Japan, the Carribean, and the southeastern US.
- Large Granular Lymphocyte Leukemia (LGL): T-LGL cells are typically large with multiple azurophilic granules, and the disease is associated with pancytopenia symptoms, splenomegaly, and Rheumatoid Arthritis.
- Acute lymphoblastic lymphoma (ALL): It is associated with increased lymphoblasts rather than more mature lymphocytes.
- Drugs and drug hypersensitivity reactions: Certain medications such as allopurinol, carbamazepine, vancomycin, and sulfa drugs may have correlated drug reactions with eosinophilia and systemic symptoms (DRESS), and this can be related to lymphocytosis. The relatively new CLL medication Bruton tyrosine kinase (BTK) inhibitor Ibrutinib has resulted in impressive responses; however, it correlates with the worsening of lymphocytosis upon initiation of the medication. It likely represents a redistribution of CLL cells from lymphoid tissues to the peripheral blood and does not indicate a suboptimal response to therapy.[7]
- Monoclonal B Lymphocytosis (MBL): this refers to the presence of monoclonal B cells at a level less than 5000 cells/microL in the absence of features of lymphoproliferative disorders, splenomegaly or cytopenias. These B cells most commonly have the same phenotype of those seen in CLL (CLL-like); however, their phenotype may be different (atypical MBL).
- Congenital B cell Lymphocytosis: this is due to germline heterozygous missense mutation in CARD11, a scaffolding protein required for nuclear factor kappa B (NF-KB) in both B and T lymphocytes.[8] It typically progresses to CLL by the 4th decade of life.
- Persistent B-cell polyclonal B-Lymphocytosis: It is a rare clinical entity described as polyclonal binucleated lymphocytes occurring predominantly in young smoker woman. Unlike CLL or MBL, lymphocytes are polyclonal with the expression of both kappa and lambda chains. It is associated with HLA DR-7 and IgM polyclonal gammopathy and exhibits a stable clinical and biological course.[9]
- Stress: Severe and emergency medical conditions may correlate with transient lymphocytosis that would precede neutrophilia. Most patients had cardiac conditions, status epileptics, or epinephrine use.[10]
- Asplenia: similar to other blood components, lymphocyte count, may increase post-splenectomy but typically stays stable for years.
Epidemiology
The epidemiology of lymphocytosis varies by age and particular etiologies. Below is some demographic data for the most common causes.
- EBV: EBV infection is widespread worldwide among all age groups, and around 90% of adults will eventually become seropositive. IM though traditionally peaks in young adults at age 15 to 24 years, but can happen later in life.[11] Symptomatic clinical infection is much more common in the Caucasians compared to African Americans.[12]
- Pertussis and cat-scratch disease: pertussis predominantly affects children less than ten years of age, but could occur in adults where it might portend a more severe course in the elderly.[13] Cat-scratch disease is also more common among children and young adults. Within the US, it is more common in the southeastern region, where the incidence might be as high as 6.4 cases per 100000 people.
- CLL: CLL is the most common leukemia in adult patients in the US, especially in older adults with a median age of diagnosis of 70 years. It is more common in men (male to female ratio of around 1.5 to 1) and more common among the White population.
- NHL: The frequency of peripheral blood lymphocytosis varies by the type of lymphoma and ranges from 20 to 80%.[5]
- MBL: The prevalence of MBL is very high compared to CLL and reaches 5 to 9% in the population over 60 years of age. MBL is also more common in males than in females.[14]
- Drug reaction with eosinophilia and systemic symptoms (DRESS): Lymphocytosis in DRESS can occur in around 30 to 70% of cases.
Pathophysiology
The pathophysiology of lymphocytosis varies by etiology. Increased lymphocyte production may be either due to a clonal process or a reactive process. Also, redistribution of lymphoid cells may be the primary etiology in some patients presenting with lymphocytosis. The mechanism of some of the most common causes follows:
- EBV: During the early stages of IM, EBV infects resting B-cells, and a large number of infected B cells circulate the blood. The atypical lymphocytes, however, are activated cytotoxic CD8+ cells that appear 1 to 3 weeks after onset of symptoms. In the patients infected with EBV, memory B-cells are latently infected and lead to chronic infection with possible reactivation and predisposition to lymphoproliferative disorders.[15]
- Pertussis: the mechanism of lymphocytosis in pertussis may be due to decreased extravasation of lymphocytes from peripheral blood to lymphoid organs and/or expansion of morphologically normal CD4+ T cells.[16]
- Congenital B-cell lymphocytosis: as discussed above, this is related to mutations in CARD11, a scaffolding protein required for nuclear factor Kappa B (NF-KB) in both B and T lymphocytes.
- CLL: several genetic and chromosomal lesions paly a role in the malignant development of CLL B lymphocytes, in addition to antigens that could play a role in malignant cell selection. Examples of genetic mutations include NOTCH1, a regulator of hematopoietic progenitor cells differentiation, and TP53, a tumor suppressor gene. A full appraisal of the pathogenesis of this disorder is beyond the scope of this review.
- NHL: several chromosomal abnormalities are present, depending on the type of lymphoma. Classic examples include t(11,14) in MCL and associated overexpression of cyclin D1, a cell cycle regulator, and t(14,18) in FL, leading to overexpression of BCL2, an anti-apoptotic protein.
History and Physical
History and physical (H&P) is an essential part of the evaluation as it might reveal the underlying etiology, or may help to point out the need for an expedited evaluation. Some of the critical points in H&P include:
- The clinical setting is crucial as it occurs in patients presenting to the emergency department following seizures, trauma, or cardiac events.
- The patient has a personal or family history of a lymphoproliferative disorder.
- The patient has a history of B-symptoms (fever, weight loss, and night sweats) that could point out a clonal process.
- Demographics: age is an important feature, as some cases occur in specific populations (e.g., CLL is mainly a disease of the elderly), while others are more common in certain groups (for example, AIM is common in young adults).
- Surgical history: Splenectomy is associated with lymphocytosis.
- Medications review.
- History for methods of transmissions if certain viral infections are suspected (e.g., sexual history in HIV).
- The physical exam findings should be interpreted in the clinical context as rash, lymphadenopathy, or splenomegaly can occur in different malignant or reactive disorders.
Evaluation
The evaluation of lymphocytosis begins with a detailed history and physical examination. The complete blood count (CBC) and review of the peripheral blood smear (PBS) are essential to start an appropriate workup.
- CBC: CBC review will help to confirm the presence of absolute lymphocytosis and to delineate abnormalities in other blood components such as hemoglobin and platelets. Anemia and thrombocytopenia might indicate a clonal disorder such as CLL or lymphoma. Also, the magnitude of the rise and the presence of abnormal or immature forms of cells (e.g., blasts) will help dictate the urgency of evaluation.
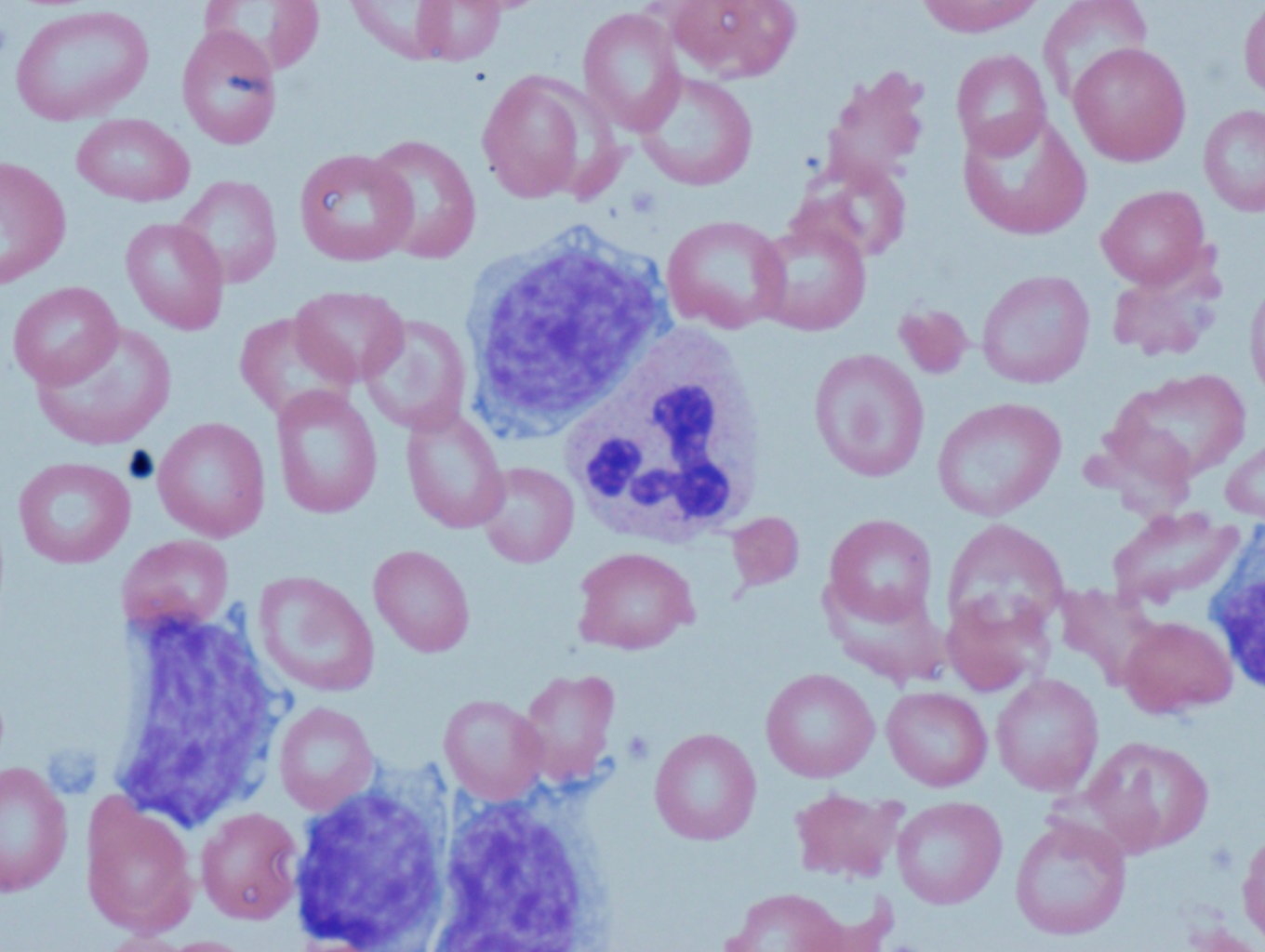
- PBS: examples of distinct lymphocyte forms that may be identifiable on PBS include:
- Small mature looking lymphocytes and "smudge cells" in CLL and MBL
- Atypical large lymphocytes are visible in EBV and other viral infections such as CMV or early HIV
- Lymphocytes that are cleaved angulated, or have indented nuclei can be associated with pertussis or malignancies such as follicular lymphoma.
- "Hairy cells" with regular cytoplasmic projections are seen in hairy cell leukemia
- Sezary Cells have cribriform nuclei with compact chromatin
- "Villous" lymphocytes are seen in MZL
- Large lymphocytes with multiple azurophilic granules are present in T-LGL
- Lymphoblasts in ALL
- Additional testing:
- Flow Cytometry: Peripheral blood flow cytometry is essential to determine the proliferation of monoclonal cells. It is a costly test and should not be ordered routinely on all patients with lymphocytosis.
- Certain features on peripheral blood smear or on review of CBC which prompt a physician to order flow cytometry include:
- The presence of lymphoblasts on the peripheral blood smear, suggesting ALL- This should also prompt a referral to a tertiary care center to obtain further workup.
- The presence of other abnormal lymphocyte morphology on PBS as detailed above
- ALC more than 30000 cells/microL
- Persistent unexplained lymphocytosis for more than one month
- Abnormalities in other cell lines including anemia and thrombocytopenia
- Presence of lymphadenopathy and/or hepatosplenomegaly in the right clinical context where reactive causes have been ruled out
- Flow cytometry patterns are beneficial in delineating clonality and differentiating clonal disorders as follows:
- CLL: lymphocytes are CD5+, CD23+, CD20 (dim), CD10-, cyclin D1-, weak sIg (surface immunoglobulin), FMC -, CD200 +
- MCL: lymphocytes are CD5+, CD23-, CD10-, CD20+, sIg +, cyclin D1 +, FMC +, CD200-
- FL: lymphocytes are CD5-, CD10+, CD20+, sIg+ and often BCL2+, BCL6+
- MZL: lymphocytes are CD5-, CD10-, CD20+, sIg+, cyclin D1-
- HCL: lymphocytes are CD5-, CD10-, CD20+, sIg+, CD11c+, CD25+, CD103+
- T-LGL: lymphocytes are CD3+, CD8+, CD16+, CD56+
- Certain features on peripheral blood smear or on review of CBC which prompt a physician to order flow cytometry include:
- Fluorescence in situ hybridization (FISH), karyotype, and mutation analysis: FISH, karyotype, and certain mutation analysis help diagnose and risk stratification of hematologic malignancies, especially CLL and lymphomas. The FISH can not only help to ascertain the clonal nature of lymphocytosis but also helps to confirm the diagnosis of certain lymphomas. Examples include:
- FL: characterized by t(14,18)
- MCL: characterized by t(11,14)
- HCL: characterized by the presence of BRAF mutation
- CLL: different karyotypic abnormalities including del 17p, del 11q, trisomy 12, and del 13q14.
- Flow Cytometry: Peripheral blood flow cytometry is essential to determine the proliferation of monoclonal cells. It is a costly test and should not be ordered routinely on all patients with lymphocytosis.
Treatment / Management
The management of lymphocytosis depends on the underlying etiology. While some causes reflect only a reactive or physiologic process that does not need any intervention (e.g., stress or asplenia), others indicate a malignant or clonal process that might require intervention.
- Acute infectious mononucleosis: The management is typically supportive, with analgesics and/or non-steroidal anti-inflammatory drugs (NSAIDs). As the majority of patients have splenomegaly, they should be instructed to avoid contact sports during the early acute stage to avoid splenic rupture. The use of corticosteroids is controversial, and the current body of literature does not provide enough evidence to support its use for symptomatic relief.[17]
- Other infectious causes: The management of the underlying etiology directs the treatment. For example; The management of pertussis differs from infants to adolescents and adults. Antibiotics (e.g., azithromycin or clarithromycin) are generally indicated in adult patients when presenting within three weeks of the cough onset. Likewise, appropriate antimicrobials are an option Bartonella Henselae, MTB, HIV, or toxoplasmosis.
- CLL: The management of CLL has moved towards the use of targeted therapies such as BTK inhibitors (Ibrutinib), BCL-2 inhibitor (Venetoclax), and PI3K inhibitors (Idelalisib). In general, the first step in CLL management is by appropriate selection of patients needing therapy. These are patients with progressive cytopenias, constitutional symptoms, progressive or symptomatic lymphadenopathy, and hepatosplenomegaly. The second important step in CLL management relies on risk stratification and predictive factors. Particularly, the presence of 17p del or TP53 mutation predicts for lack of response from standard chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab (FCR) or bendamustine plus rituximab (BR). These patients are better suited for the use of BTK inhibitors (Ibrutinib) or Venetoclax in combination with the humanized anti-CD20 monoclonal antibody obinutuzumab. The phase III ECOG-E1912 has proved the superiority of the combination of Ibrutinib and rituximab (IbRx) over the FCR regimen in younger patients (age less than 70 years) diagnosed with CLL without del17 mutation. The progression-free survival (89.4% in the IbRx arm vs. 72.9% in the FCR arm at 3 years; hazard ratio for progression or death, 0.35; 95% confidence interval [CI], 0.22 to 0.56; P<0.001)and overall survival (98.8% in the IbRx arm vs. 91.5% in FCR arm at 3 years; hazard ratio for death, 0.17; 95% CI, 0.05 to 0.54; P<0.001) were significantly prolonged in patients diagnosed with CLL, even in those with IGHV mutation.[18]
- NHL: The management of NHL management depends on the histology. For instance, where a patient diagnosed with 'double-hit' DLBCL may require prompt initiation of treatment, a patient diagnosed with low-grade FL can be monitored clinically for signs of growth or transformation. The treatment options for NHL have increased with the advent of targeted agents. The typical medications, namely, rituximab, doxorubicin, cyclophosphamide, vincristine, and steroids (either prednisone or dexamethasone) are still in use as first-line treatment in various permutations and combinations. However, newer drugs like brentuximab vedotin (anti-CD-30 and drug conjugate), lenalidomide, obinutuzumab, etc. are being tested and approved in both first-line and second-line setting to improve patient outcomes. The treatment of MCL requires more intense chemotherapy, with a possibility of performing autologous stem cell transplantation in consolidation. Purine analogs (cladribine and pentostatin) are standard treatments for HCL. Methotrexate is usually the initial drug for T-LGL patients requiring therapy.
- MBL: All patients diagnosed with MBL can receive clinical monitoring. Typically, they follow up with their hematologist twice a year for the first two years for high count CLL-like MBL and atypical MBL, which can extend longer for stable patients. Only symptomatic patients or those whose blood tests show a worsening lymphocytosis warrant further imaging and bone marrow aspirate and biopsy.
- DRESS: The first step in managing patients with DRESS is to withdraw the offending drug. Supportive measures usually suffice. Topical or systemic corticosteroids may be needed depending on the extent of involvement of the skin and/or other organs. (A1)
Differential Diagnosis
The differential diagnosis of lymphocytosis is broad and was discussed above in the etiology section.
Medical Oncology
Keys points pertinent to malignant causes of lymphocytosis were discussed in the above sections.
Prognosis
The prognosis of a patient with lymphocytosis depends on the underlying etiology. Examples of specific disease prognosis are as follows:
- Acute IM: Most patients recover from the acute episode of mononucleosis, although some continue to have fatigue for a prolonged period.[19] However, EBV infected latent B cells may lead to the development of EBV-related lymphoproliferative disorders, including post-transplant lymphoproliferative disorder (PTLD), Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma in immunocompromised individuals.[19]
- Other infections: Pertussis in adults may cause prolonged symptoms (greater than two weeks).[20] Prior to antiretroviral therapy, advanced HIV infection median overall survival was dismal, ranging from 12 to 18 months. Prognosis depends on many factors, including the ability to successfully implement antiretroviral therapies, and there are several indices used to estimate survival in HIV infections (e.g., Veterans Aging Cohort Study index).
- CLL: CLL prognosis is highly dependant on risk stratification and whether a patient presents with high-risk features or not. These latter include a high-risk karyotype (del 17p and del 11q), unmutated IGHV status, high ZAP-70, CD38, and Beta-2 microglobulin levels.[21][22]
- NHL: The prognosis depends on the type of histology. Histologies like FL, MZL, and HL are incurable but have a prolonged indolent course. On the other hand, DLBCL and T-cell lymphomas are aggressive but responsive to therapy.
- DRESS: mortality rates from DRESS are reported to be around 5 to 10%.[21] However, most patients will recover following offending drug withdrawal.
Complications
The complications from lymphocytosis coincide with the underlying etiology where leukemia is the most common underlying disease.
- Hyperleukocytosis: Defined as a white cell count above 100000 cells/microL. It is more commonly seen in patients diagnosed with acute myeloid leukemia but can appear in patients presenting with acute lymphoblastic leukemia as well as CML. Hyperleukocytosis can lead to leukostasis and consequent symptoms like vision loss, stroke, myocardial infarction, etc. Prompt initiation of white-cell lowering treatment (either hydroxyurea or leukapheresis) is required to relieve the symptoms.[22]
- Infectious mononucleosis: splenic rupture and chronic fatigue are short term complications that may happen in patients with infectious mononucleosis. B-cell malignancies are potential long term sequelae of EBV infection, including PTLD, HL, and NHL, which usually occur in the immunocompromised patients.[23]
- CLL: Leukostasis is uncommon in CLL. Autoimmune processes may complicate CLL, including autoimmune hemolytic anemia and immune thrombocytopenia. Hypogammaglobulinemia, with or without recurrent infections, is also common. CLL patients are also at a higher risk of developing secondary malignancies, including solid and hematologic ones.[24]
- DRESS: DRESS patients may have different organ involvement, including liver, lung, and kidneys. Further, these patients are reported to have a higher subsequent incidence of autoimmune diseases as well as future drug reactions to potentially structurally unrelated medications.
Consultations
Appropriate consultation between primary care physicians (PCP) and hematologists is paramount. While some causes of lymphocytosis will resolve with observation or supportive management alone, others may need more prompt evaluation. The presence of highly elevated counts (ALC greater than 30000 cells/microL) or rapidly increasing ones should alert PCP to consult hematology specialists. Likewise, hematology consultants should direct management in cases needing intervention and provide guidance when clinical monitoring is appropriate.
Deterrence and Patient Education
Lymphocytosis by itself is often a sign of an underlying disorder. Recognition of its presence, as defined by an ALC over 4000 cells/microL, is the first step. A second important issue is the recognition of the urgency or lack of it in referral to hematology. A detailed history, coupled with a complete physical examination and review of complete blood counts, provides a preliminary idea regarding the underlying etiology. Patients with no alarming features and typical history for a reactive cause of lymphocytosis can be reassured and monitored clinically. Patients with infectious mononucleosis should be instructed to refrain from contact sports during the acute phase of their illness that fatigue may continue after the resolution of other symptoms.
Any alarming features, like significant weight loss, anorexia, excessive night sweats, or an abnormal physical exam (lymphadenopathy or hepato-splenomegaly), should trigger a hematology referral and workup. Patients with suspicion or confirmation of leukemia should receive a prompt referral to academic centers specializing in the treatment of leukemia.
Pearls and Other Issues
- The definition of lymphocytosis in adults is an ALC over 4000 cells/microL and can be due to elevation of different lymphocytes compartments
- Common causes of reactive lymphocytosis: infections (EBV, CMV, pertussis, cat-scratch disease, HIV, etc.), drug reactions (DRESS), stress, and asplenia.
- Common causes of lymphocytosis secondary to monoclonal expansion: CLL/SLL, MBL (ALC under 5000 cells/microL), NHL (MZL, FL, MCL), T-LGL, HCL, Scezary syndrome.
- Lymphocytosis is detected incidentally in the majority of the patients.
- The evaluation starts with an extensive history and physical and review of peripheral blood smear review, which may direct for the need for further testing (flow cytometry, karyotype, and FISH).
- Clues to the presence of clonal lymphoproliferative disorders include a highly elevated ALC, presence of abnormal lymphocyte forms on PBS, and the presence of other cytopenias.
- The underlying etiology determines management and prognosis.
- Communication between PCP and hematologists is essential to guide management and to implement interventions promptly.
Enhancing Healthcare Team Outcomes
Lymphocytosis is often incidental and detected on routine peripheral blood count. It is essential to keep a thorough and systematic approach to diagnose the underlying etiology appropriately. A comprehensive history and a detailed physical examination are critical as they provide important clues towards the etiology of lymphocytosis. An Interprofessional team, including primary care physicians (PCP), internists, pathologists, and hematologists, is essential for establishing an accurate diagnosis and initiating appropriate management. This team will also include nursing and pharmacy personnel, depending on the significance of the findings and ultimate diagnosis. Often a pharmacist specializing in oncology will be required to assist with medication selection, management, and family education. An oncology nurse may be required to help with the coordination of care. The family clinician is often the first point of contact. They should familiarize themselves with common causes of lymphocytosis and also recognize alarming features that would prompt additional investigations. All hematologists should review the peripheral blood smear and obtain a peripheral blood flow cytometry if needed. However, if the smear detects an alarming finding, then a trained heme-pathologist must be consulted for confirmation. When clinical observation is appropriate, then communication between the hematologist and the PCP/internist as well as pharmacist and nursing staff should be clear and unambiguous to reassure the patient.
Lymphocytosis has many underlying causes with different approaches to diagnosis and management. The management of lymphocytosis, which occurs secondary to an underlying malignancy like lymphoma or leukemia, is directed towards the underlying cause and is supported by level I evidence.
Media
(Click Image to Enlarge)
References
Brigden ML, Au S, Thompson S, Brigden S, Doyle P, Tsaparas Y. Infectious mononucleosis in an outpatient population: diagnostic utility of 2 automated hematology analyzers and the sensitivity and specificity of Hoagland's criteria in heterophile-positive patients. Archives of pathology & laboratory medicine. 1999 Oct:123(10):875-81 [PubMed PMID: 10506437]
Rosenberg ES, Caliendo AM, Walker BD. Acute HIV infection among patients tested for mononucleosis. The New England journal of medicine. 1999 Mar 25:340(12):969 [PubMed PMID: 10094651]
Level 3 (low-level) evidenceFiala M, Heiner DC, Turner JA, Rosenbloom B, Guze LB. Infectious mononucleosis and mononucleosis syndromes. The Western journal of medicine. 1977 Jun:126(6):445-59 [PubMed PMID: 195404]
Arber DA, George TI. Bone marrow biopsy involvement by non-Hodgkin's lymphoma: frequency of lymphoma types, patterns, blood involvement, and discordance with other sites in 450 specimens. The American journal of surgical pathology. 2005 Dec:29(12):1549-57 [PubMed PMID: 16327427]
Level 2 (mid-level) evidenceGeorge TI. Malignant or benign leukocytosis. Hematology. American Society of Hematology. Education Program. 2012:2012():475-84. doi: 10.1182/asheducation-2012.1.475. Epub [PubMed PMID: 23233622]
Matutes E, Parry-Jones N, Brito-Babapulle V, Wotherspoon A, Morilla R, Atkinson S, Elnenaei MO, Jain P, Giustolisi GM, A'Hern RP, Catovsky D. The leukemic presentation of mantle-cell lymphoma: disease features and prognostic factors in 58 patients. Leukemia & lymphoma. 2004 Oct:45(10):2007-15 [PubMed PMID: 15370245]
Level 2 (mid-level) evidenceWoyach JA, Smucker K, Smith LL, Lozanski A, Zhong Y, Ruppert AS, Lucas D, Williams K, Zhao W, Rassenti L, Ghia E, Kipps TJ, Mantel R, Jones J, Flynn J, Maddocks K, O'Brien S, Furman RR, James DF, Clow F, Lozanski G, Johnson AJ, Byrd JC. Prolonged lymphocytosis during ibrutinib therapy is associated with distinct molecular characteristics and does not indicate a suboptimal response to therapy. Blood. 2014 Mar 20:123(12):1810-7. doi: 10.1182/blood-2013-09-527853. Epub 2014 Jan 10 [PubMed PMID: 24415539]
Snow AL, Xiao W, Stinson JR, Lu W, Chaigne-Delalande B, Zheng L, Pittaluga S, Matthews HF, Schmitz R, Jhavar S, Kuchen S, Kardava L, Wang W, Lamborn IT, Jing H, Raffeld M, Moir S, Fleisher TA, Staudt LM, Su HC, Lenardo MJ. Congenital B cell lymphocytosis explained by novel germline CARD11 mutations. The Journal of experimental medicine. 2012 Nov 19:209(12):2247-61. doi: 10.1084/jem.20120831. Epub 2012 Nov 5 [PubMed PMID: 23129749]
Level 3 (low-level) evidenceTroussard X, Cornet E, Lesesve JF, Kourel C, Mossafa H. Polyclonal B-cell lymphocytosis with binucleated lymphocytes (PPBL). OncoTargets and therapy. 2008 Oct 1:1():59-66 [PubMed PMID: 21127753]
Teggatz JR, Parkin J, Peterson L. Transient atypical lymphocytosis in patients with emergency medical conditions. Archives of pathology & laboratory medicine. 1987 Aug:111(8):712-4 [PubMed PMID: 3632284]
Heath CW Jr, Brodsky AL, Potolsky AI. Infectious mononucleosis in a general population. American journal of epidemiology. 1972 Jan:95(1):46-52 [PubMed PMID: 5007364]
Nye FJ. Social class and infectious mononucleosis. The Journal of hygiene. 1973 Mar:71(1):145-9 [PubMed PMID: 4348454]
Skoff TH, Hadler S, Hariri S. The Epidemiology of Nationally Reported Pertussis in the United States, 2000-2016. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019 May 2:68(10):1634-1640. doi: 10.1093/cid/ciy757. Epub [PubMed PMID: 30169627]
Rawstron AC, Green MJ, Kuzmicki A, Kennedy B, Fenton JA, Evans PA, O'Connor SJ, Richards SJ, Morgan GJ, Jack AS, Hillmen P. Monoclonal B lymphocytes with the characteristics of "indolent" chronic lymphocytic leukemia are present in 3.5% of adults with normal blood counts. Blood. 2002 Jul 15:100(2):635-9 [PubMed PMID: 12091358]
Thorley-Lawson DA, Gross A. Persistence of the Epstein-Barr virus and the origins of associated lymphomas. The New England journal of medicine. 2004 Mar 25:350(13):1328-37 [PubMed PMID: 15044644]
Kubic VL, Kubic PT, Brunning RD. The morphologic and immunophenotypic assessment of the lymphocytosis accompanying Bordetella pertussis infection. American journal of clinical pathology. 1991 Jun:95(6):809-15 [PubMed PMID: 2042590]
Rezk E, Nofal YH, Hamzeh A, Aboujaib MF, AlKheder MA, Al Hammad MF. Steroids for symptom control in infectious mononucleosis. The Cochrane database of systematic reviews. 2015 Nov 8:2015(11):CD004402. doi: 10.1002/14651858.CD004402.pub3. Epub 2015 Nov 8 [PubMed PMID: 26558642]
Level 1 (high-level) evidenceShanafelt TD, Wang XV, Kay NE, Hanson CA, O'Brien S, Barrientos J, Jelinek DF, Braggio E, Leis JF, Zhang CC, Coutre SE, Barr PM, Cashen AF, Mato AR, Singh AK, Mullane MP, Little RF, Erba H, Stone RM, Litzow M, Tallman M. Ibrutinib-Rituximab or Chemoimmunotherapy for Chronic Lymphocytic Leukemia. The New England journal of medicine. 2019 Aug 1:381(5):432-443. doi: 10.1056/NEJMoa1817073. Epub [PubMed PMID: 31365801]
Buchwald DS, Rea TD, Katon WJ, Russo JE, Ashley RL. Acute infectious mononucleosis: characteristics of patients who report failure to recover. The American journal of medicine. 2000 Nov:109(7):531-7 [PubMed PMID: 11063953]
Teepe J, Broekhuizen BD, Ieven M, Loens K, Huygen K, Kretzschmar M, de Melker H, Butler CC, Little P, Stuart B, Coenen S, Goossens H, Verheij TJ, GRACE consortium. Prevalence, diagnosis, and disease course of pertussis in adults with acute cough: a prospective, observational study in primary care. The British journal of general practice : the journal of the Royal College of General Practitioners. 2015 Oct:65(639):e662-7. doi: 10.3399/bjgp15X686917. Epub [PubMed PMID: 26412843]
Level 2 (mid-level) evidenceCacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, Roujeau JC. The DRESS syndrome: a literature review. The American journal of medicine. 2011 Jul:124(7):588-97. doi: 10.1016/j.amjmed.2011.01.017. Epub 2011 May 17 [PubMed PMID: 21592453]
Röllig C, Ehninger G. How I treat hyperleukocytosis in acute myeloid leukemia. Blood. 2015 May 21:125(21):3246-52. doi: 10.1182/blood-2014-10-551507. Epub 2015 Mar 16 [PubMed PMID: 25778528]
Level 3 (low-level) evidenceNeparidze N, Lacy J. Malignancies associated with epstein-barr virus: pathobiology, clinical features, and evolving treatments. Clinical advances in hematology & oncology : H&O. 2014 Jun:12(6):358-71 [PubMed PMID: 25003566]
Level 3 (low-level) evidenceTsimberidou AM, Wen S, McLaughlin P, O'Brien S, Wierda WG, Lerner S, Strom S, Freireich EJ, Medeiros LJ, Kantarjian HM, Keating MJ. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009 Feb 20:27(6):904-10. doi: 10.1200/JCO.2008.17.5398. Epub 2008 Dec 29 [PubMed PMID: 19114699]
Level 2 (mid-level) evidence