Introduction
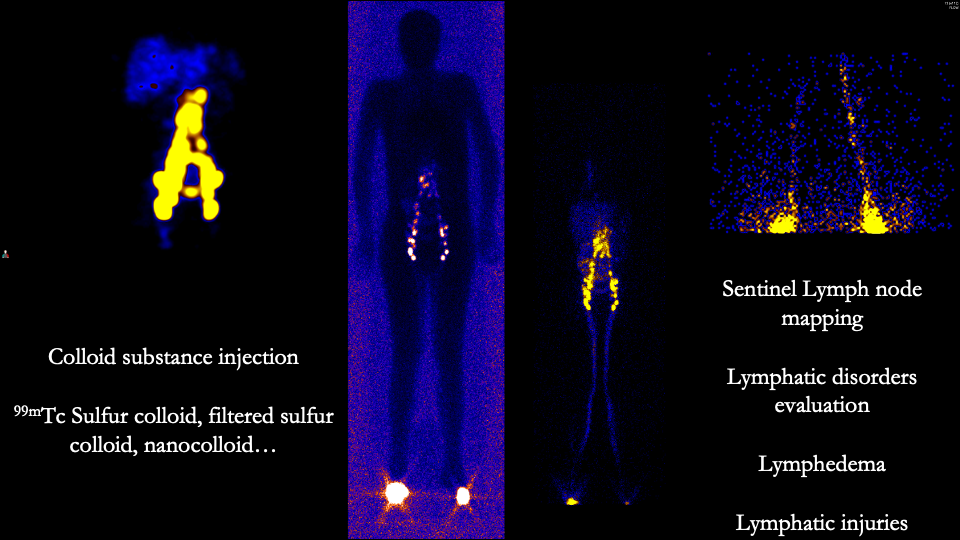
Lymphoscintigraphy is a nuclear medicine imaging study for mapping the lymphatic system with scintigraphy. Attempts at understanding and mapping the lymphatic system began in the 1600s with the discovery of the cisterna chyli and thoracic duct.[1] The lymphatic drainage of the breast was first described in 1786 and identified 2 dominant drainage pathways of the breast: the axillary lymphatic basin and the internal mammary nodes.[2] Subsequently, intradermal or parenchymal injection of scintigraphic agents was found to be equivalent to an intralymphatic injection. In the late 20th century, protocols employing radiopaque contrast agents to visualize the first lymph node to receive the contrast agent, also termed the “sentinel lymph node,” were developed.[3] Several radioisotopes have been used for lymphoscintigraphy; current lymphoscintigraphic techniques utilize Technetium Tc 99m sulfur colloid.[4] The ideal radiotracer for lymphoscintigraphy will demonstrate rapid transfer to and prolonged stay within the lymph node.
Understanding the map of lymphatic drainage patterns of anatomical structures defines the clinical application of lymphoscintigraphy. A sentinel lymph node is the first node that accepts lymphatic drainage from an anatomical site. In cases of malignancy, such as malignant melanoma or breast cancer, the sentinel lymph node is most likely to harbor occult metastases. Sentinel lymph node histopathologic analysis, in the absence of overt metastases, can potentially preclude the need for adjuvant therapies, including lymphadenectomy, radiotherapy, chemotherapy, or more invasive surgical procedures. Lymphoscintigraphy has become the standard of care when managing select breast cancer and melanoma cases; other applications include the evaluation of lymphedema.[4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The lymphatic system drains lymph, which is water and other constitutive elements of the interstitial space with a composition similar to plasma, to the vascular system (see Image. Lymphoscintigraphy).[5][6] From descriptions as early as those of Sappey in 1874 and through ongoing lymphatic mapping, the predominant conceptual understanding of the lymphatic zones draining the skin are:
- Four zones of skin on the trunk drain to the axillary or groin lymphatic basins [7]
- Any region of skin along the borders of these zones has a less predictable drainage pattern [7]
- Postsurgical changes can often result in significant variability in lymphatic drainage patterns [8]
Under normal circumstances, most breast lymphatics drain to the ipsilateral axillary lymph nodes. Approximately 3% of breast lymphatics drain to the internal mammary chain nodes, and a smaller proportion drains to the posterior intercostal lymph nodes.[9] Given the infrequent and unlikely nodal basin of the posterior intercostal lymph nodes, this drainage pattern is considered less clinically relevant. The Sappey areolar plexus constitutes a complex network of lymphatics in and around the nipple-areolar complex. This plexus is clinically relevant; subareolar or periareolar radiotracer injection utilizes this lymphatic network to identify a sentinel lymph node.[10]
Malignant melanoma frequently presents on the skin of the lower extremities and torso.[11] The ipsilateral axillary lymph nodes drain the upper extremities, and the inguinal lymph nodes drain the lower extremities. While the drainage of torso cutaneous melanomas is relatively predictable, aberrant drainage basins are frequently encountered, most notably from the longitudinal and horizontal midlines of the torso. Additional sites of potentially aberrant drainage include the long head of the triceps muscle and the triangular intermuscular space formed by the borders of the teres major and minor muscles. [12]
Indications
Lymphoscintigraphy is typically performed in the following circumstances:
- As an adjunct to clinical staging and preoperative planning in patients with breast cancer
- To identify sentinel lymph node drainage in patients with malignant melanoma as an adjunct to staging and treatment planning
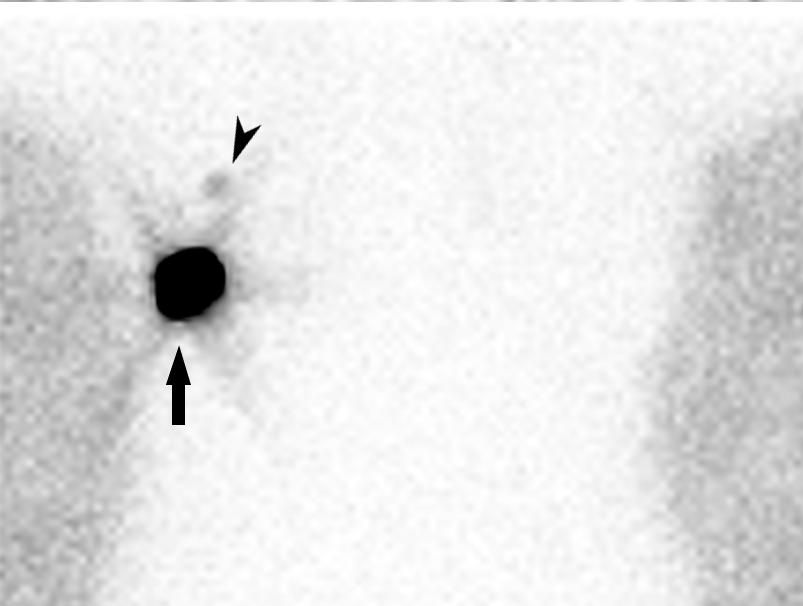
- When diagnosing and evaluating lymphatic flow disorders such as chronic lymphedema (see Image. Lymphoscintigraphy, Lymphedema) [13]
- When evaluating chylous ascites or chylothorax [14]
- When evaluating patients with specific gynecologic cancers.[15][16][11]
Contraindications
Absolute contraindications to lymphoscintigraphy include but are not limited to clinically positive nodal disease. Relative contraindications to the procedure include allergies to radioisotopes or components of the radiotracer preparation, pregnancy, and significant alterations to normal anatomy, including those encountered after prior therapeutic interventions.
Equipment
The equipment to perform lymphoscintigraphy typically includes:
- Collimator: low-energy, all-purpose, parallel (LEAP) collimator
- Gamma camera
- Gamma probe; an instrument typically utilized in the operating room
- Radiotracer: the most commonly utilized radiotracer is filtered or unfiltered technetium Tc 99m sulfur colloid; other radiotracers are available
- Filtered tracer typically requires a 22-μ millipore filter
- A pH-balanced 1% lidocaine additive can be considered based on institutional preference.
Preparation
In preparation for lymphoscintigraphy, a comprehensive medical history should be obtained, prior imaging studies should be thoroughly reviewed, and pregnancy status should be definitively identified and adequately documented. The indications, risks, benefits, and alternatives to the procedure should be thoroughly explained to the patient before informed consent to proceed is obtained. The possibility of pain during injection of the radiotracer should be explicitly discussed. Jewelry or overlying objects that may result in photo attenuation should be removed; this includes necklaces that may obscure visualization of the internal mammary lymph nodes. The injection site should be examined, marked, and cleansed.
Lymphoscintigraphy is typically performed with the patient either supine or prone. Patients undergoing lymphoscintigraphy for the evaluation of breast cancer should position their arms in a position mimicking that held intraoperatively.
Technique or Treatment
Radiotracer activities vary and depend on the institution. The activity typically utilized for lymphoscintigraphy ranges from 0.1 to 10 mCi; doses are often adjusted depending on the timing of the injection with planned surgery. The injection technique and the number of injections will vary among institutions and may include peritumoral, intradermal, periareolar, and subareolar techniques; the chosen technique has demonstrated little effect on sentinel lymph node identification.
Considerable institutional variation exists for lymphoscintigraphy procedures. However, the following generalities typically persist:
- When evaluating melanoma or other cutaneous lesions, radiotracer can be injected intradermally around the lesion using a fine-gauge needle tangential to the skin.
- A combination of deep and superficial radiotracer injections may decrease the number of false-positive lymphoscintigraphic results in patients being evaluated for breast malignancies.[17]
- A synchronous injection of the affected and contralateral extremities is preferred when evaluating patients with lymphedema.
Following radiotracer injection, sequential or continuous imaging is performed for 30 to 60 minutes; the routine field of view includes the expected drainage direction. Intense activity at the site of radiotracer administration may need to be attenuated with lead. Massaging the injection area may improve radiotracer distribution. Transmission images with a Cobalt-57 source are often utilized, and oblique views may also be useful in node identification.
Complications
Lymphoscintigraphy is relatively noninvasive and has few adverse effects. One of the most common complications associated with lymphoscintigraphy is radiopharmaceutical extravasation into perivascular tissues; no long-term adverse effects have been reported. Another common complication of lymphoscintigraphy is an allergic reaction to the radiotracer or its preparation. Allergic reactions to radiotracers are rare; reactions to the preparation contents, such as lidocaine, are more common.
Clinical Significance
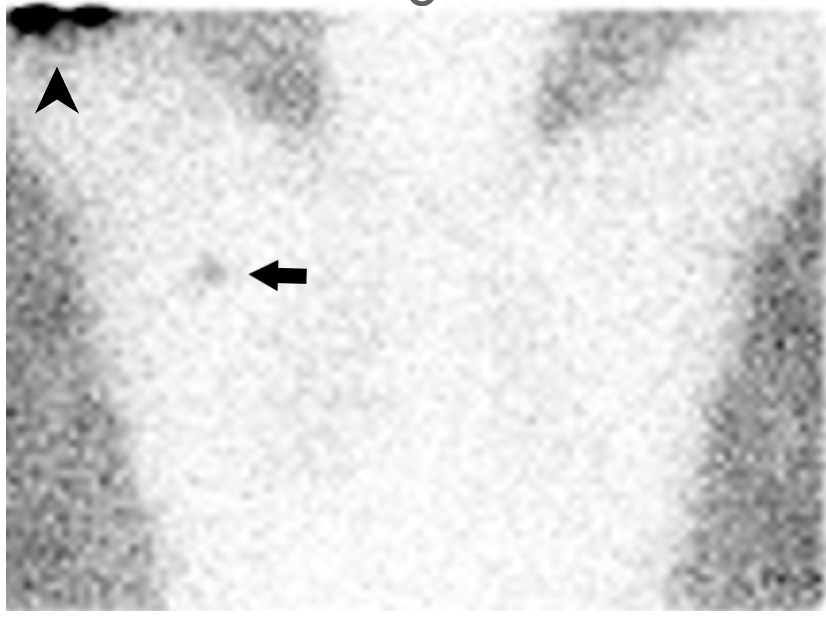
The identification of a sentinel lymph node in patients undergoing evaluation for breast cancer or melanoma has a critical role in guiding treatment strategies. A sentinel lymph node provides diagnostic information regarding the presence or absence of metastases and predicts the metastatic potential for the evaluated malignancy. The decision to employ surgical techniques that include more extensive interventions is also guided by the presence or absence of metastases in a sentinel lymph node (see Image. Lymphoscintigraphy, Breast Cancer).
The morbidity associated with axillary lymph node dissection, namely lymphedema, has furthered the role of lymphoscintigraphy. The added advantage of histopathologic sectioning of a single lymph node and the ability to use staining in a more targeted manner can promote better detection of isolated tumor cells.[18] Observations on the limitations of lymph node dissection, its effect on overall survival, and the lack of survival benefit of lymphadenectomy following the identification of a positive sentinel lymph node underscore the need for effective lymphoscintigraphic methods.[19][20][21]
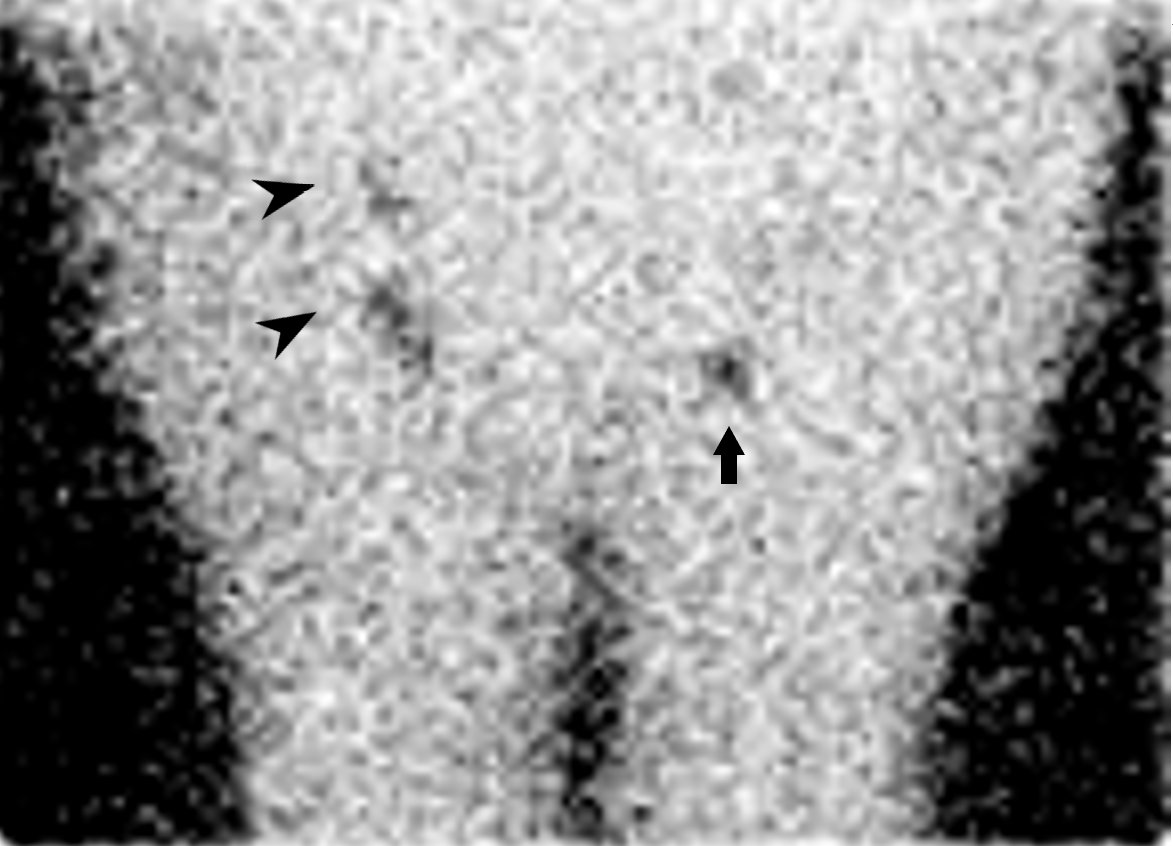
Sentinel lymph node identification and biopsy as a staging tool in intermediate-thickness melanoma has similarly precluded the need for lymph node dissection in patients for whom such a surgical intervention would yield little benefit (see Image. Lymphoscintigraphy, Melanoma).[22] Lymphadenectomy following positive sentinel lymph node identification in patients with melanoma offers little benefit.[23]
Enhancing Healthcare Team Outcomes
Lymphoscintigraphy is a diagnostic nuclear medicine imaging modality that employs radiotracers to identify neoplastic lymph node involvement and lymphatic system flow issues. The most effective way to enhance patient outcomes is through coordination of care to smoothly execute the examination, interpret the results, and relay those results to the pertinent parties. This coordination of care begins before the patient arrives at the imaging facility. Accurate and timely scheduling of the examination facilitates patient satisfaction. Once the study is scheduled, the ordering physician should be informed; some patients must proceed immediately to sentinel lymph node biopsy.
A comprehensive preimaging questionnaire should be completed with the assistance of clinical nursing or scheduling staff. This questionnaire should include inquiries about recent surgical procedures, imaging studies with radiopharmaceuticals, and a general medical history. Particular attention must be paid to any history of allergic reactions, particularly to radiopharmaceuticals; while rare, such an allergy may require modifications to the radiotracer preparation or alternate imaging methods.
The nuclear medicine technician must perform scintillation camera quality control measures according to the general guidelines of the Society of Nuclear Medicine. The chosen radiotracers should be prepared and shipped when necessary within an appropriate timeframe to avoid radioactive decay.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
Lymphoscintigraphy, Melanoma. Transmission imaging 30 minutes following Technitium Tc 99m sulfur colloid injection in the right upper extremity (arrowhead) of a patient with right upper arm melanoma. A sentinel lymph node is identified within the right axillary lymph node basin (arrow).
Contributed by D Tafti, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
Lymphoscintigraphy, Breast Cancer. Transmission images acquired 30 minutes following injection of radiotracer into the breast. Intense activity (arrow) is demonstrated at the injection site and a star artifact is seen secondary to septal penetration. A sentinel right axillary lymph node is identified (arrowhead).
Contributed by D Tafti, MD
References
Suy R, Thomis S, Fourneau I. The discovery of the lymphatic system in the seventeenth century. Part II: the discovery of Chyle vessels. Acta chirurgica Belgica. 2016 Oct:116(5):329-335. doi: 10.1080/00015458.2016.1195587. Epub 2016 Aug 26 [PubMed PMID: 27563735]
Suami H, Pan WR, Taylor GI. Historical review of breast lymphatic studies. Clinical anatomy (New York, N.Y.). 2009 Jul:22(5):531-6. doi: 10.1002/ca.20812. Epub [PubMed PMID: 19484798]
Tanis PJ, Nieweg OE, Valdés Olmos RA, Th Rutgers EJ, Kroon BB. History of sentinel node and validation of the technique. Breast cancer research : BCR. 2001:3(2):109-12 [PubMed PMID: 11250756]
Level 1 (high-level) evidenceKazem I, Antoniades J, Brady LW, Faust DS, Croll MN, Lightfoot D. Clinical evaluation of lymph node scanning utilizing colloidal gold 198. Radiology. 1968 May:90(5):905-11 [PubMed PMID: 5643593]
Moore JE Jr, Bertram CD. Lymphatic System Flows. Annual review of fluid mechanics. 2018 Jan:50():459-482. doi: 10.1146/annurev-fluid-122316-045259. Epub [PubMed PMID: 29713107]
Cirocchi R, Metaj G, Cicoletti M, Arcangeli F, De Sol A, Poli G, Bruzzone P, Gioia S, Anagnostou C, Loreti F, Francesconi S, Ricci L, Laurenti ME, Capotorti A, Artico M, D'Andrea V, Henry BM, Fedeli P, Carlini L. Analysis of the Different Lymphatic Drainage Patterns during Sentinel Lymph Node Biopsy for Skin Melanoma. Journal of clinical medicine. 2021 Nov 26:10(23):. doi: 10.3390/jcm10235544. Epub 2021 Nov 26 [PubMed PMID: 34884243]
Reynolds HM, Walker CG, Dunbar PR, O'Sullivan MJ, Uren RF, Thompson JF, Smith NP. Functional anatomy of the lymphatics draining the skin: a detailed statistical analysis. Journal of anatomy. 2010 Mar:216(3):344-55. doi: 10.1111/j.1469-7580.2009.01183.x. Epub 2010 Jan 7 [PubMed PMID: 20070428]
Suami H, Koelmeyer L, Mackie H, Boyages J. Patterns of lymphatic drainage after axillary node dissection impact arm lymphoedema severity: A review of animal and clinical imaging studies. Surgical oncology. 2018 Dec:27(4):743-750. doi: 10.1016/j.suronc.2018.10.006. Epub 2018 Oct 12 [PubMed PMID: 30449502]
Level 3 (low-level) evidenceZhou Y, Hou J, Meng N, Daniel S, Chen J, Xu L. Case Report: Intercostal Lymph Node Metastasis: A Case Report and Review of the Literature. Frontiers in oncology. 2021:11():638948. doi: 10.3389/fonc.2021.638948. Epub 2021 Mar 4 [PubMed PMID: 33747962]
Level 3 (low-level) evidenceRinaldi RM, Sapra A, Bellin LS. Breast Lymphatics. StatPearls. 2023 Jan:(): [PubMed PMID: 31971733]
Burke TW, Levenback C, Tornos C, Morris M, Wharton JT, Gershenson DM. Intraabdominal lymphatic mapping to direct selective pelvic and paraaortic lymphadenectomy in women with high-risk endometrial cancer: results of a pilot study. Gynecologic oncology. 1996 Aug:62(2):169-73 [PubMed PMID: 8751545]
Level 3 (low-level) evidenceHerbert GS, Beshlian KM. The triangular intermuscular space as a site of lymph node metastasis in melanoma of the back. Annals of plastic surgery. 2010 Jan:64(1):52-4. doi: 10.1097/SAP.0b013e31819b6c87. Epub [PubMed PMID: 20023455]
Kalawat TC, Chittoria RK, Reddy PK, Suneetha B, Narayan R, Ravi P. Role of lymphoscintigraphy in diagnosis and management of patients with leg swelling of unclear etiology. Indian journal of nuclear medicine : IJNM : the official journal of the Society of Nuclear Medicine, India. 2012 Oct:27(4):226-30. doi: 10.4103/0972-3919.115392. Epub [PubMed PMID: 24019651]
Zhang L, Zhang X, Wen Z, Tong G, Hao K, Qiu Y, Kang L. Lymphoscintigraphy findings in patients with chylothorax: influence of biochemical parameters. EJNMMI research. 2023 Aug 3:13(1):72. doi: 10.1186/s13550-023-01014-0. Epub 2023 Aug 3 [PubMed PMID: 37535169]
Level 2 (mid-level) evidenceSlomovitz BM, Coleman RL, Oonk MH, van der Zee A, Levenback C. Update on sentinel lymph node biopsy for early-stage vulvar cancer. Gynecologic oncology. 2015 Aug:138(2):472-7. doi: 10.1016/j.ygyno.2015.05.017. Epub 2015 May 27 [PubMed PMID: 26022527]
Lécuru F, Mathevet P, Querleu D, Leblanc E, Morice P, Daraï E, Marret H, Magaud L, Gillaizeau F, Chatellier G, Dargent D. Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: results of the SENTICOL study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011 May 1:29(13):1686-91. doi: 10.1200/JCO.2010.32.0432. Epub 2011 Mar 28 [PubMed PMID: 21444878]
Giammarile F, Alazraki N, Aarsvold JN, Audisio RA, Glass E, Grant SF, Kunikowska J, Leidenius M, Moncayo VM, Uren RF, Oyen WJ, Valdés Olmos RA, Vidal Sicart S. The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. European journal of nuclear medicine and molecular imaging. 2013 Dec:40(12):1932-47. doi: 10.1007/s00259-013-2544-2. Epub 2013 Oct 2 [PubMed PMID: 24085499]
Level 1 (high-level) evidenceChen SL, Iddings DM, Scheri RP, Bilchik AJ. Lymphatic mapping and sentinel node analysis: current concepts and applications. CA: a cancer journal for clinicians. 2006 Sep-Oct:56(5):292-309; quiz 316-7 [PubMed PMID: 17005598]
Fisher B, Anderson S. Conservative surgery for the management of invasive and noninvasive carcinoma of the breast: NSABP trials. National Surgical Adjuvant Breast and Bowel Project. World journal of surgery. 1994 Jan-Feb:18(1):63-9 [PubMed PMID: 8197778]
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, Saha S, Hunt KK, Morrow M, Ballman K. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Annals of surgery. 2010 Sep:252(3):426-32; discussion 432-3. doi: 10.1097/SLA.0b013e3181f08f32. Epub [PubMed PMID: 20739842]
Level 1 (high-level) evidenceGiuliano AE, Ballman K, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, Saha S, Morrow M, Hunt KK. Locoregional Recurrence After Sentinel Lymph Node Dissection With or Without Axillary Dissection in Patients With Sentinel Lymph Node Metastases: Long-term Follow-up From the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 Randomized Trial. Annals of surgery. 2016 Sep:264(3):413-20. doi: 10.1097/SLA.0000000000001863. Epub [PubMed PMID: 27513155]
Level 1 (high-level) evidenceFaries MB, Cochran AJ, Elashoff RM, Thompson JF. Multicenter Selective Lymphadenectomy Trial-I confirms the central role of sentinel node biopsy in contemporary melanoma management: response to 'No survival benefit for patients with melanoma undergoing sentinel lymph node biopsy: critical appraisal of the Multicenter Selective Lymphadenectomy Trial-I final report'. The British journal of dermatology. 2015 Mar:172(3):571-3. doi: 10.1111/bjd.13676. Epub [PubMed PMID: 25776247]
Faries MB, Thompson JF, Cochran AJ, Andtbacka RH, Mozzillo N, Zager JS, Jahkola T, Bowles TL, Testori A, Beitsch PD, Hoekstra HJ, Moncrieff M, Ingvar C, Wouters MWJM, Sabel MS, Levine EA, Agnese D, Henderson M, Dummer R, Rossi CR, Neves RI, Trocha SD, Wright F, Byrd DR, Matter M, Hsueh E, MacKenzie-Ross A, Johnson DB, Terheyden P, Berger AC, Huston TL, Wayne JD, Smithers BM, Neuman HB, Schneebaum S, Gershenwald JE, Ariyan CE, Desai DC, Jacobs L, McMasters KM, Gesierich A, Hersey P, Bines SD, Kane JM, Barth RJ, McKinnon G, Farma JM, Schultz E, Vidal-Sicart S, Hoefer RA, Lewis JM, Scheri R, Kelley MC, Nieweg OE, Noyes RD, Hoon DSB, Wang HJ, Elashoff DA, Elashoff RM. Completion Dissection or Observation for Sentinel-Node Metastasis in Melanoma. The New England journal of medicine. 2017 Jun 8:376(23):2211-2222. doi: 10.1056/NEJMoa1613210. Epub [PubMed PMID: 28591523]