Introduction
Mitral regurgitation (MR) is the most common valvular abnormality worldwide, affecting over 2% of the total population, and has a prevalence that increases with age.[1][2][3] MR is the retrograde flow of blood from the left ventricle (LV) into the left atrium (LA) through the mitral valve (MV), causing a systolic murmur heard best at the apex of the heart with the sound radiating to the left axilla (see Image. Mitral Regurgitation During Systole).
Anatomy of Mitral Valve
The mitral valve consists of 2 leaflets (anterior and posterior) sitting within the annulus. The posterior mitral leaflet originates from the LA endocardium. The leaflets are supported by a subvalvular apparatus comprising 2 papillary muscles (anterolateral and posteromedial) that arise from the LV myocardium and the chordae tendineae.[4][5]
Types of Mitral Regurgitation
Mitral regurgitation is subdivided into primary and secondary.[6]
Primary mitral regurgitation
- Also called degenerative or organic
- Resulting from the structural deformity of or damage to the leaflets, chordae, or papillary muscles, causing leaflets to close insufficiently during systole
- Common causes: papillary muscle rupture, mitral valve prolapse (MVP), or leaflet perforation [5]
Secondary mitral regurgitation
- Also called functional or ischemic
- Due to left ventricular wall motion abnormalities (ie, ischemic cardiomyopathy) or left ventricular remodeling (ie, dilated cardiomyopathy)[7]
- No structural problems with the valve itself [8]
- Leads to mitral annular dilatation or displacement of papillary muscles, causing retrograde flow from improperly closed mitral valve leaflets
The Carpentier Classification divides mitral regurgitation into 3 types based on the leaflet motion:
- Type 1: Normal leaflet motion
- Caused by annular dilation or leaflet perforation
- Regurgitation jet directed centrally
- Type 2: Excessive leaflet motion
- Caused by papillary muscle rupture, chordal rupture, or redundant chordae
- Eccentric jet directed away from the involved leaflet
- Type 3: Restricted leaflet motion
- IIIa: Leaflet motion restricted in both systole and diastole
- Caused by rheumatic heart disease
- Normal papillary muscles
- Jet may be centrally or eccentrically directed
- IIIb: Leaflet motion restricted in systole
- IIIa: Leaflet motion restricted in both systole and diastole
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Primary Mitral Regurgitation
Degenerative: The underlying pathophysiologic basis for degenerative mitral regurgitation is most commonly related to myxomatous degeneration of the mitral valve, resulting in mitral valve prolapse (MVP). MVP can occur either as a primary, non-syndromic, or a secondary, syndromic process. In primary MVP, advancing age is the driving factor responsible for disease progression. Connective tissue diseases such as Marfan syndrome, Ehlers-Danlos syndrome, MASS phenotype, systemic lupus erythematosus, osteogenesis imperfecta, and pseudoxanthoma elasticum lead to secondary MVP, causing MR.[11]
Congenital: Conditions like isolated cleft of the mitral valve,[12] double orifice mitral valve, and parachute mitral valve (PMV), which is a congenital valvular anomaly where the chordae tendineae are attached to a single papillary muscle, have been linked to causing MR.[13] While extremely rare, these congenital conditions are well-defined in the literature as causing primary MR.
Infectious/rheumatic: With an estimation of over 15 million cases worldwide, rheumatic heart disease is prevalent in developing countries due to a lack of medical resources and vaccinations.[14] Chronic rheumatic heart disease is associated with pancarditis and has mitral valve involvement, causing regurgitation in almost 100% of cases due to scarring of the valve and valve apparatus.[15][16]
Secondary Mitral Regurgitation
Left ventricular dilation due to ischemic or nonischemic cardiomyopathy secondarily impairs leaflet coaptation of a structurally normal MV, resulting in secondary MR. Dysfunction and remodeling can lead to apical and lateral papillary muscle displacement, resulting in leaflet tethering, dilation, a flattening of the mitral annulus, and lower valve closing forces.[4] Reduced closing forces include LV contractility, altered systolic annular contraction, reduced synchronicity between the 2 papillary muscles, and global LV desynchrony, especially in basal segments.
Papillary muscle rupture: Papillary muscle rupture is a rare condition seen in 1% to 2% of patients after myocardial infarction (MI) or infective endocarditis that leads to severe mitral regurgitation due to dysfunction of the papillary muscles.[17][18]
Ischemic mitral regurgitation: Ischemic mitral regurgitation results from prior MI associated with normal mitral valve leaflets and chordae. Ischemia of the segments underlying the papillary muscles results in remodeling. This phenomenon causes papillary muscle displacement, which results in a more apical position of the leaflets, known as a "seagull sign."[19] Under Carpentier classification, the leaflet dysfunction resulting in the most common form of ischemic mitral regurgitation is type IIIb due to restricted motions of the leaflet(s) in systole. The degree of exercise-induced increase or decrease in MR relates to changes in LV remodeling, valvular deformation, and LV and papillary muscle synchronicity.
Congestive heart failure-associated: In a heart failure clinical study of 558 patients with severe congestive heart failure, defined as ejection fraction (EF) less than or equal to 35%, MR was severe in 4.3% of the patients, moderate to severe in 12.5%, moderate in 21.9%, mild to moderate in 11.8%, mild in 39.1%, and absent or present in 10.4%.[20] This study identified the correlation between severe congestive heart failure and MR.
Atrial fibrillation associated: Results from a retrospective cohort study found atrial fibrillation to cause increased atrial and valve annular size, resulting in functional MR. Of the patients studied, controlling atrial fibrillation and restoring sinus rhythm resulted in an increased reduction of functional MR.[21] A randomized trial also showed that AF had an association with worsening valvular disease.[22]
Hypertrophic cardiomyopathy: Hypertrophic cardiomyopathy (HCM) can also lead to MR. HCM is defined by severe left ventricular hypertrophy, which causes increased papillary muscle mass, bringing them closer together. This phenomenon causes the mitral valve leaflets to become elongated and floppy and pulls the leaflets closer to the left ventricular outflow tract, causing regurgitant retrograde flow.[5][23]
Epidemiology
Mitral regurgitation is a common valvular abnormality occurring in about 10% of the population.[1] Mitral valve prolapse, which is related to myxomatous degeneration of the mitral valve, is the most common cause of primary mitral regurgitation. Accounting for 2% to 3% of the total population, mitral valve prolapse has been cited as the most common cardiac mitral valvular pathology worldwide.[24] In developing countries, rheumatic heart disease remains prevalent and is the most common cause of mitral valvular pathology that results in hospital admissions.[25][26]
Pathophysiology
The definition of MR is a retrograde flow of blood from the LV into the left atrium LA through the MV, causing a systolic murmur heard best at the apex of the heart, with the sound radiating to the left axilla. Mitral regurgitation leads to left ventricular volume overload due to increased stroke volume, caused by increased blood volume within the left atrium and an increased preload delivered to the left ventricle during diastole.
In chronic progressive MR, ventricular remodeling occurs, allowing maintenance of cardiac output, and an initial increase in EF is usually observed. However, the effective EF can be considerably lower depending on the regurgitant fraction. Over time, there is a positive feedback loop by which volume overload from MR causes dilation of the ventricle, widening of the mitral annulus, and diminishing coaptation of leaflets, leading to progressive worsening of the MR.
Eventually, volume overload becomes so severe that excitation-contraction coupling of the muscle membrane becomes impaired, and wall stress-related afterload on the left ventricle leads to dilation with decreased contractility, resulting in a reduction of EF. In addition, the regurgitant blood from the left ventricle during systole can eventually cause left atrial enlargement, impairment of left atrial contraction, and subsequent atrial fibrillation, leading to a thrombus in the left atrial appendage.[3][27][28]
History and Physical
Mitral valve regurgitation causes a holosystolic murmur that is heard best at the apex of the heart, with the sound radiating to the left axilla (see Video. Murmur of Mitral Regurgitation). Differentiating the murmur of mitral regurgitation from other systolic murmurs is essential.[29]
- Mitral valve prolapse: an early systolic murmur heard best at the cardiac apex but with a mid-systolic click
- Tricuspid regurgitation: a high-pitched, blowing, holosystolic murmur heard best at the lower left sternal border, with radiation to the right lower sternal border; increases with inspiration
- Ventral septal defect: a holosystolic murmur (The more significant the ventral septal defect, the quieter the murmur.)
- Aortic stenosis: a mid-systolic, crescendo-decrescendo murmur with radiation toward the neck; gets quieter with Valsalva maneuver or standing
- Pulmonic stenosis: mid-systolic, crescendo-decrescendo murmur, increases in intensity during inspiration (In severe pulmonic stenosis, the S2 heart sound is widely split.)
- Atrial septal defect: mid-systolic murmur with a fixed split S2 heart sound; does not change with inspiration
- Hypertrophic cardiomyopathy: mid-systolic murmur, heard best medial to the cardiac apex; radiates to the left sternal border; murmur is louder with Valsalva and standing
Clinical findings related to MR are divided into 2 categories: those related to the MR itself and those associated with the underlying cause. Maintaining a broad differential diagnosis is important; with an initially focused history and physical examination, one can establish whether the MR is acute or chronic and thus significantly narrow the possible etiologies.
Acute Mitral Regurgitation
The clinical assessment of the acute onset of mitral regurgitation will elicit findings associated with a precipitous decline in cardiac output and possibly cardiogenic shock. The patient will usually complain of significant dyspnea at rest, exacerbated in the supine position, as well as cough with clear or pink, frothy sputum. They may also endorse symptoms associated with myocardial ischemia, such as chest pain radiating to the neck, jaw, shoulders, or upper extremities accompanied by nausea and diaphoresis. Physical examination may reveal altered mental status, tachycardia (or bradycardia if there is ischemic involvement of the conduction system), hypotension, tachypnea, hypoxemia, and cyanosis. Additionally, jugular venous distension, diffuse crackles on lung auscultation, and an apical holosystolic murmur with radiation to the axilla on a precordial exam may be present.
Acute MR is typically related to either papillary muscle rupture from acute coronary syndrome or fulminant destruction of the valvular apparatus secondary to acute bacterial endocarditis. Thus, further clinical assessment should focus on confirming these potentially devastating conditions.
In the case of acute bacterial endocarditis, there will be signs and symptoms of sepsis, such as fevers and chills. A history of intravenous drug abuse is highly prevalent, and patients may also have comorbid conditions that predispose them to immunocompromise, such as diabetes mellitus and alcohol use disorder. Due to the embolization of vegetative material, there may be a variety of additional clinical findings depending on the ultimate fate of the emboli. Brain involvement of the emboli will produce focal neurologic deficits; renal involvement will result in hematuria or oliguria; and cutaneous involvement will result in Janeway lesions or widespread petechiae. In contrast to subacute bacterial endocarditis, acute infections typically occur in patients with structurally normal heart valves, and, as such, rheumatic heart disease and prosthetic valves are less common in this population. Furthermore, because the route of bacterial delivery to the mitral valve passes through the right side of the heart, concomitant lesions of the tricuspid and pulmonic valves are not uncommon, and these can often be appreciated by auscultation of murmurs on physical examination.[27][30]
Chronic Mitral Regurgitation
Patients with chronic mitral regurgitation often remain asymptomatic until late in the course of the disease. Clinical findings common to all etiologies include fatigue, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, dependent edema, weight gain, jugular venous distension, widening of pulse pressure, displaced apical impulse and apical holosystolic murmur with radiation to the axilla. In more advanced cases, there may also be syncope or near syncope, cyanosis, clubbing of digits, hepatomegaly, evidence of ascites with a fluid wave or shifting dullness, gross anasarca, and evidence of pleural or pericardial effusions. These latter findings are reflective of the development of pulmonary hypertension and resultant right ventricular systolic dysfunction from chronic pressure overload. The differential diagnosis is also considerably broader, with specific clinical findings dependent on the etiology.[27]
Evaluation
Several tools are used to evaluate mitral regurgitation; the patient’s history and physical examination should guide the ordering of diagnostic tests.
Echocardiogram
Echocardiography is the primary and essential diagnostic test for diagnosing and assessing mitral regurgitation.[31] Transthoracic echocardiography and transesophageal echocardiography provide qualitative and quantitative analysis.
Various methods are available to quantify MR. One such method involves measuring the vena contracta, which represents the width of the regurgitant jet as it exits the regurgitant orifice. This provides insight into the regurgitant orifice area (eg, vena contracta greater than 7 mm is consistent with severe MR).
The Doppler volumetric method is also an option for quantifying MR. This method measures the regurgitant volume as the difference between the mitral and aortic stroke volumes. Regurgitant volume can be calculated as the product of effective regurgitant orifice area (EROA) and MR velocity time integral. Severe MR is quantified as:
- EROA greater than or equal to 0.2 cm2
- Regurgitant volume greater than or equal to 30 mL
- Regurgitant fraction of 50% or higher [32][33]
After the initial echocardiographic evaluation, repeat echocardiography is indicated for patients with moderate or greater MR with or without symptoms every:
- Severe: 6 to 12 months
- Moderate: 1 to 2 years
- Mild: 3 to 5 years
Repeat echocardiography is also a recommendation for patients with any degree of MR and a change in clinical status or physical examination findings.[31][34]
Following MV repair, successful mitigation of MR can be quantified via several tools. One method is measuring tenting height, which is the greatest mid-systolic distance from leaflet tips to the annular plane of the mitral valve. The tenting area is defined as the area bounded by the mitral annular plane and the anterior and posterior leaflets at mid-systole. In the healthy heart, normal values are:
- Tenting height of less than 0.5 cm
- Tenting area of 0 cm2
- Angles of the anterior and posterior mitral leaflet are less than 3 degrees
Poor outcomes after MV repair are defined as:
- Tenting height of greater than or equal to 1 cm
- Tenting area of greater than 2.5 to 3 cm2
- Complex jets
- Posterolateral angle of over 45 degrees [19][35]
The sphericity index can also quantify the successful mitigation of MR following MV repair. The sphericity index is the ratio between the LV end-diastolic volume and the volume of an imaginary sphere, with its diameter extending from the midpoint of the annular plane to the apex. End-diastolic diameter exceeding 65 mm, end-systolic diameter over 51 mm, and systolic sphericity index greater than 0.7 predict unfavorable outcomes of MV repair.[35]
Successful MV repair can also be quantified by assessing distance and wall motion. An interpapillary distance of over 20 mm, posterior papillary fibrosis distance of more than 40 mm, and lateral wall motion abnormality are associated with poor outcomes after MV repair surgery.
Electrocardiogram
Atrial fibrillation is the most common electrocardiogram finding in patients with MR.[27] Patients with atrial fibrillation can also present with more severe MR than patients without arrhythmia.[22]
Chest Radiography
In patients with chronic MR, cardiomegaly due to left-atrial or right-sided heart enlargement is visible on anterior-posterior x-ray views.[27]
Exercise Stress Testing
In patients with severe, asymptomatic, primary MR, exercise treadmill testing may provide information regarding the patient’s symptom status and exercise tolerance. Exercise echocardiography is useful to assess changes in MR severity and pulmonary artery pressure in those symptomatic with non-severe MR at rest.[27]
Cardiac Catheterization
Cardiac catheterization can quantify MR volume with high accuracy when clinical findings are inconsistent with noninvasive test results.
Cardiac Magnetic Resonance Imaging
Cardiac magnetic resonance imaging (MRI) is an important and complementary tool to other modalities for assessing the severity of MR. Cardiac MRI accurately assesses quantitative measurements, including regurgitant volume and regurgitant fraction. Cardiac MRI determination of severe MR demonstrates a stronger correlation with left ventricular remodeling (specifically, smaller left ventricular end-diastolic volume following the elimination of MR) than echocardiography. Clinically, cardiac MRI should help differentiate severe from non-severe MR in patients whose echocardiographic evaluation is inconclusive, particularly if contemplating surgery.[36][37]
Biomarkers
In response to heightened wall stress, ventricular myocytes release the biomarker B-type natriuretic peptide (BNP), which correlates with symptom severity and offers prognostic insights for individuals with MR. A BNP level may be normal in severe, compensated MR without symptoms or adverse hemodynamic effects. An elevated BNP level is associated with the composite endpoint of the New York Heart Association (NYHA) class III or IV heart failure symptoms, LV dysfunction (ejection fraction less than 60%), or death during follow-up of patients with asymptomatic, severe MR.[38]
Treatment / Management
The choice of medical versus surgical management of mitral regurgitation depends on the condition’s severity, chronicity, comorbidities, and etiology. While some pharmacologic agents can be used in MR, the evidence for their use is not strong, and they do not have a recommendation from the American College of Cardiology (ACC) or the American Heart Association (AHA).[31] Primary severe MR and ischemic severe MR usually receive treatment with valve surgery.[31][39] (A1)
Medical Management of Mitral Regurgitation
Angiotensin-converting enzyme inhibitors (ACE) and angiotensin II receptor blockers (ARBs) have been used in those who are asymptomatic to delay the progression of MR.[40] The belief is that ACE inhibitors and ARBs can decrease regurgitant volume and LV size in patients with chronic primary MR.[41][42] However, there are limited supporting results from studies, and their overall role in treating MR is discouraged.[31][39][43] Some study results have concluded no improvement or survival benefit in patients with MR using ACE inhibitors or ARBs and have even shown worsening outcomes for some.[44][45] In the setting of hypertrophic cardiomyopathy or mitral valve prolapse, vasodilators have demonstrated an increase in the severity of MR.[46](A1)
Beta-blockers for the treatment of MR have also been studied, with results revealing little to no benefit with beta-blocking agents in primary MR; some results have shown increased survival benefit with these agents in secondary MR.[47] One study evaluating the beta blocker carvedilol supported its use after demonstrating the preservation of LV function, remodeling, and decreased regurgitant volume.[48] The ACC/AHA does not have specific recommendations regarding using beta-blockers in patients with MR.[31] (A1)
Loop diuretics are believed to be helpful in conjunction with other pharmacologic agents to further decrease afterload and regurgitant volume, but further studies are necessary to support this association properly.[41] (A1)
Surgical Management of Mitral Regurgitation
The decision whether to operate is dependent on the underlying cause of MR. Patients with valvular damage due to chordal or papillary muscle rupture or infective endocarditis require surgery. Patients with functional causes of MR, such as ischemia, generally require coronary artery bypass grafting.[2][49] Patients with acute, symptomatic MR or an EROA of at least 4 cm2 require surgical intervention.[28] Surgery for MR is indicated in patients with LV function deterioration or an end-systolic diameter of 45 mm.[50] Patients diagnosed with primary severe MR require surgery when symptomatic with an ejection fraction over 30% or asymptomatic with an EF of 30% to 60%.[51] (B3)
Mitral valve repair has 2 aims:
- An acceptable surface area of mitral valve leaflet coaptation
- Essential annular dilatation of 5 to 8 mm [50]
The ACC and AHA generally recommend mitral valve repair over replacement due to decreased recurrence of MR after repair.[31][52] Available data reveal decreased morbidity and mortality after surgical repair over replacement.[53] However, mitral valve replacement is favorable over repair when there is extensive tissue destruction, which can occur in some cases of infective endocarditis.[49] Nevertheless, the newest AHA guidelines clearly state that “mitral valve replacement is preferable to a poor repair.”(A1)
With respect to surgical replacement of the mitral valve, mechanical prostheses are usually preferable to bioprosthetics due to increased durability and less complicated insertion. Postoperatively, both types require anticoagulation, with bioprosthetic valve replacement requiring only temporary anticoagulation and lifelong anticoagulation with warfarin for mechanical valves.[54]
Mitraclip is another surgical procedure proven to be effective and has low morbidity and mortality in patients considered to be at high risk for repair or replacement.[54] Mitraclip can decrease the mitral valve area, leading to stenosis, and therefore, an area of under 4 cm2 is a contraindication for this procedure.[55]
Differential Diagnosis
Clinical findings related to MR can be divided into 2 categories: those related to the MR itself and those associated with the underlying cause. Maintaining a broad differential diagnosis is crucial. In general, with an initially focused history and physical examination, one can establish whether the MR is acute or chronic and significantly narrow the possible etiologies that can include the following:
- Congestive heart failure exacerbation
- Acute coronary syndrome
- Hemodynamically unstable dysrhythmia
- Cardiac tamponade
- Pneumothorax
- Pulmonary embolism
- Septic shock
- Thyrotoxicosis or thyroid storm
The differential diagnosis of chronic mitral regurgitation is also considerably broader, and specific clinical findings depend on the etiology.
Staging
The following staging data for MR is from the 2020 AHA/ACC updated guidelines for managing heart valve disease, including mitral regurgitation:
Stage A
- At risk of mitral regurgitation (ie, infective endocarditis, mitral valve prolapse)
- Normal valve leaflets, chords, and annulus in patients with coronary disease or cardiomyopathy
- Hemodynamics: no MR jet or a small central jet area less than 20% LA on Doppler; small vena contracta less than 3 mm; MR grade can be described as trace or trivial
- Cardiac consequences: none or those that are unrelated to the valvular changes
- Patients at this stage remain asymptomatic [7][31]
Stage B
- Progressive mitral regurgitation occurs in this stage.
- ECG assessment of mitral valve anatomy demonstrates mild tethering of mitral leaflets and annular dilation with a normal to slight loss of central coaptation that may be associated with prior infective endocarditis (IE.)
- Hemodynamics: EROA is less than 0.4 cm2, regurgitant volume below 60 mL, and regurgitant fraction below 50%. There might be a central regurgitant jet that is only 20% to 40% in magnitude or a late systolic eccentric jet. The venta contracta should not exceed 7 mm in width in all cases. MR grade is 1+ to 2+.
- Cardiac consequences: Left atrial enlargement begins at this stage. Left ventricular dimensions and pulmonary pressures are usually not affected.
- Patients at this stage remain asymptomatic.
Stage C
- Asymptomatic severe mitral regurgitation occurs in this stage.
- ECG assessment of mitral valve anatomy shows a flail leaflet or severe mitral valve prolapse (MVP) and loss of central coaptation due to leaflet restriction. Causes can be prior IE or a history of chest irradiation.
- Hemodynamics: EROA is greater than or equal to 0.4 cm2, regurgitant volume is greater than or equal to 60 mL, regurgitant fraction is greater than or equal to 50%, central regurgitant jet that is greater than 40%, or there is a pansystolic eccentric jet. MR grade is 2+ to 3+.
- Cardiac consequences: patients at this stage are categorized as C1 (preserved ejection fraction greater than 60%, LV end-systolic diameter is less than 40 mm, or C2 (reduced ejection fraction less than or equal to 60% or LV end-systolic diameter is greater than 40 mm). Both categories exhibit moderate to severe LA enlargement with some LV distension.
- Patients at this stage remain largely asymptomatic. Some patients may experience symptoms upon severe physical exertion.
Stage D
- Symptomatic severe mitral regurgitation defines this stage.
- ECG assessment of mitral valve anatomy is similar to stage C with increased severity and extent.
- Hemodynamics: EROA is greater than 0.4 cm2, regurgitant volume greater than or equal to 60 mL, regurgitant fraction greater than or equal to 50%, vena contracta greater than or equal to 7 mm, central regurgitant jet that is greater than 40%, or a pansystolic eccentric jet. MR grade is 3+ to 4+.
- Cardiac changes as described in grade C with evidence of pulmonary hypertension
- Heart failure symptoms due to mitral regurgitation persist even after revascularization and optimization of medical therapy, decreased exercise tolerance, and exertional dyspnea.
Prognosis
Mitral regurgitation is a common yet debilitating condition that leads to increased morbidity and mortality, and research is valuable for finding new techniques for managing this condition.[56] Mitral valve repair and replacement surgeries have been extensively studied and have shown significant improvement in symptoms and mortality.
Several pertinent studies follow:
- A study of 144 patients with mitral regurgitation found that the 5-year mortality was a remarkable 30% compared to 13% of the age-matched control group. The study also determined that patients with functional mitral regurgitation had an overall increase in morbidity and mortality than those with structural MR.[57]
- Another study of patients 50 and older with medical treatment alone for mitral regurgitation calculated a yearly mortality rate for moderate and severe organic mitral regurgitation as 3% and 6%, respectively.[6]
- A study of 83 patients (asymptomatic, mean age of 56, and undergoing early mitral valve surgery) found residual mitral regurgitation requiring re-repair in 1%, and 4% required a permanent pacemaker. The 10-year survival rate after surgery was 91.5%.[58]
- Patients with degenerative or rheumatic heart disease and a mean age of 57 years undergoing mitral valve repair had comparable survival rates with individuals in the general population. A study of 125 mitral valve repairs determined postoperative early mortality in 2.4% of the patients and a 10-year survival rate of 84.3%.[59]
- A systematic review and meta-analysis of patients with severe MR with a reduced ejection fraction (under 40%) compared mitral valve repair surgery versus mitral valve replacement surgery regarding operative mortality. In one study of patients undergoing mitral valve repair, the operative mortality was determined to be 5%. However, the mortality rate following mitral valve replacement was estimated to be 10%.[53]
The greatest predictor of survival and improvement of symptoms after MV surgery was shown to be a pre-operative ejection fraction over 60%.[60] Mitral valve repair is associated with increased survival and decreased morbidity and mortality compared to mitral valve replacement.[54][61]
Complications
Complications of mitral regurgitation include:
- Heart failure and related symptoms (ie, shortness of breath)
- Atrial fibrillation
- Stroke due to arrhythmias
- Pulmonary artery hypertension
- Dilation of the heart and cardiomegaly
Complications of mitral valve surgery or replacement include:
- Infections (including infective endocarditis)
- Bleeding
- Clotting and stenosis of new valve
- Valve dysfunction
- Arrhythmias
- Stroke
- Death
Postoperative and Rehabilitation Care
Most patients can be discharged postoperatively if no complications (ie, infection or bleeding) arise during the procedure or hospitalization.
Postoperative guidelines have undergone study, and the following are the recommendations:
- A postoperative ECG should be performed soon after the procedure before discharge and is periodically necessary to assess left ventricular function, especially if symptoms arise.
- Lifelong anticoagulation, typically with warfarin, is indicated for mechanical or prosthetic valve replacements.
- Clinicians should initiate antibiotic prophylaxis for infective endocarditis before dental, oral, or upper respiratory tract procedures in patients with a mechanical or prosthetic valve or a history of endocarditis.[27][62][63]
Exercise therapy and cardiac rehabilitation after heart valve surgery have been extensively studied and are generally recommended. Some data supports improved exercise capacity and ejection fraction; however, further studies are needed to develop a definite correlation.[64][65][66][67]
In a retrospective study of 105 patients who underwent heart valve surgery, the mean time for them to return to work was about 5 months. These patients also showed improved ejection fraction, with 78.4% of patients studied categorized in NYHA stage I or II compared with 38.1% before heart valve surgery.[68]
Consultations
A cardiologist is necessary for the diagnosis and medical management of MR, and a cardiothoracic surgeon consult would be necessary if surgery is indicated.
Deterrence and Patient Education
Patients could benefit from understanding the symptoms indicative of severe MR and recognizing when to seek medical assistance. Additionally, it is valuable for patients with MR to understand the criteria for surgery and available treatment options. While patients diagnosed with moderate or severe secondary mitral regurgitation may benefit from surgery, with an improvement in symptoms and quality of life, there has been no proven survival benefit from surgery. In most cases, it is not indicated or performed.[31]
- In the older adult population (eg, 60+), study results have shown that surgeons opt not to perform this surgery due to no survival benefit. Several factors affect treatment decisions. In a study of 1741 patients with mitral regurgitation, only 60.31% received surgical treatment. This number decreased to 54.71% in the age group greater than 60.[69]
- In another study of 396 patients diagnosed with severe mitral regurgitation, 49% were not operated on due to comorbid conditions.[70]
- Surgical decision-making should consider impaired left-ventricular ejection fraction, older age, and comorbid conditions.
Consult with a cardiologist regarding the management of mitral regurgitation, as patient treatment options can vary depending on several factors.
Enhancing Healthcare Team Outcomes
Mitral valve regurgitation is an increasingly common valvular heart disease associated with a wide range of causes and symptoms. Due to comorbidities, MR has a significant mortality rate, especially in the population older than 60, and the only definitive treatment is surgery.[6] MR is universally under-diagnosed and under-treated, leading to its increased prevalence.[56] The ACC and AHA have developed evidence-based guidelines for evaluating, diagnosing, and managing valvular diseases.[31]
Interprofessional healthcare team members should recognize that early diagnosis and management have proven to be lifesaving, and advancements in medicine and valvular studies have contributed to a significant decrease in morbidity and mortality of this disease. Developing a team of specialized healthcare professionals, such as cardiologists and cardiac surgeons, has significantly improved patient care due to efficiency and efficacy in managing the patient and the decision-making process.[71]
Nurses trained in cardiology monitor patients, provide education, and facilitate team communication, reporting all observations to the appropriate clinical staff. Pharmacists review the dosing and potential interactions of medications and educate patients and the healthcare team. Patient care does not end in the operating room; postoperative care and cardiac rehabilitation require a team of healthcare professionals who are crucial for improved patient outcomes and morale.
Media
(Click Image to Enlarge)
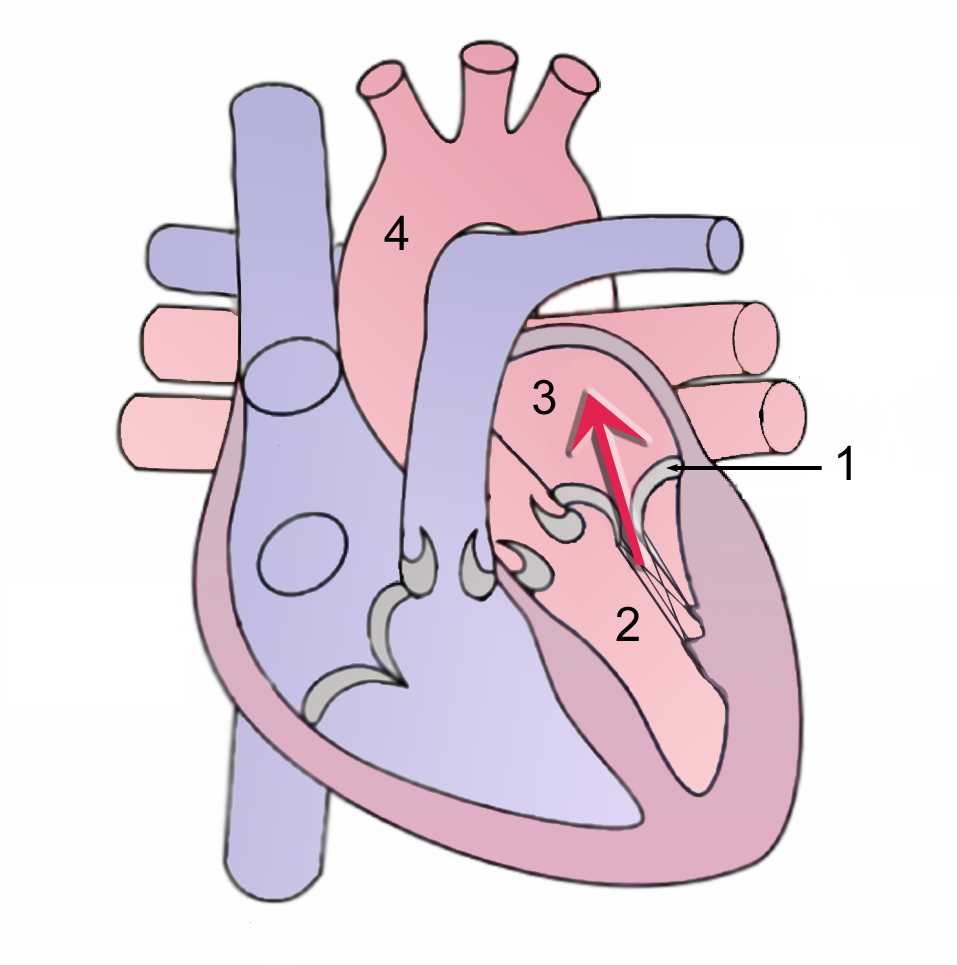
Mitral Regurgitation During Systole. Retrograde flow of blood through the mitral valve from the left ventricle to the left atrium. (1) Mitral valve (2) Left Ventricle (3) Left Atrium (4) Aorta.
J Heuser, Public Domain, via Wikimedia Commons
(Click Video to Play)
Murmur of Mitral Regurgitation. Murmur of mitral regurgitation as heard on auscultation of the heart.
Contributed by K Humphreys
References
Wu S, Chai A, Arimie S, Mehra A, Clavijo L, Matthews RV, Shavelle DM. Incidence and treatment of severe primary mitral regurgitation in contemporary clinical practice. Cardiovascular revascularization medicine : including molecular interventions. 2018 Dec:19(8):960-963. doi: 10.1016/j.carrev.2018.07.021. Epub 2018 Jul 24 [PubMed PMID: 30060923]
Coleman W, Weidman-Evans E, Clawson R. Diagnosing and managing mitral regurgitation. JAAPA : official journal of the American Academy of Physician Assistants. 2017 Jun:30(6):11-14. doi: 10.1097/01.JAA.0000516342.41351.6d. Epub [PubMed PMID: 28452853]
Apostolidou E, Maslow AD, Poppas A. Primary mitral valve regurgitation: Update and review. Global cardiology science & practice. 2017 Mar 31:2017(1):e201703. doi: 10.21542/gcsp.2017.3. Epub 2017 Mar 31 [PubMed PMID: 31139637]
Asgar AW, Mack MJ, Stone GW. Secondary mitral regurgitation in heart failure: pathophysiology, prognosis, and therapeutic considerations. Journal of the American College of Cardiology. 2015 Mar 31:65(12):1231-1248. doi: 10.1016/j.jacc.2015.02.009. Epub [PubMed PMID: 25814231]
Dal-Bianco JP, Beaudoin J, Handschumacher MD, Levine RA. Basic mechanisms of mitral regurgitation. The Canadian journal of cardiology. 2014 Sep:30(9):971-81. doi: 10.1016/j.cjca.2014.06.022. Epub 2014 Jul 2 [PubMed PMID: 25151282]
Enriquez-Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet (London, England). 2009 Apr 18:373(9672):1382-94. doi: 10.1016/S0140-6736(09)60692-9. Epub 2009 Apr 6 [PubMed PMID: 19356795]
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jun 10:63(22):2438-88. doi: 10.1016/j.jacc.2014.02.537. Epub 2014 Mar 3 [PubMed PMID: 24603192]
Level 1 (high-level) evidenceSchmitto JD, Lee LS, Mokashi SA, Bolman RM 3rd, Cohn LH, Chen FY. Functional mitral regurgitation. Cardiology in review. 2010 Nov-Dec:18(6):285-91. doi: 10.1097/CRD.0b013e3181e8e648. Epub [PubMed PMID: 20926937]
Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL, European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2010 May:11(4):307-32. doi: 10.1093/ejechocard/jeq031. Epub [PubMed PMID: 20435783]
Ginghină C, Vlădaia A, Ghiorghiu I, Serban M, Popescu BA, Jurcuţ R. Echocardiography in congenital mitral valve regurgitation--the liaison between cardiologist and surgeon. Journal of medicine and life. 2009 Oct-Dec:2(4):407-13 [PubMed PMID: 20108755]
Spartalis M, Tzatzaki E, Spartalis E, Athanasiou A, Moris D, Damaskos C, Garmpis N, Voudris V. Mitral valve prolapse: an underestimated cause of sudden cardiac death-a current review of the literature. Journal of thoracic disease. 2017 Dec:9(12):5390-5398. doi: 10.21037/jtd.2017.11.14. Epub [PubMed PMID: 29312750]
Zhu D, Bryant R, Heinle J, Nihill MR. Isolated cleft of the mitral valve: clinical spectrum and course. Texas Heart Institute journal. 2009:36(6):553-6 [PubMed PMID: 20069080]
Rouskas P, Giannakoulas G, Kallifatidis A, Karvounis H. Parachute-like mitral valve as a cause of mitral regurgitation. Hippokratia. 2016 Jul-Sep:20(3):238-240 [PubMed PMID: 29097893]
Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clinical epidemiology. 2011 Feb 22:3():67-84. doi: 10.2147/CLEP.S12977. Epub 2011 Feb 22 [PubMed PMID: 21386976]
Chockalingam A, Gnanavelu G, Elangovan S, Chockalingam V. Clinical spectrum of chronic rheumatic heart disease in India. The Journal of heart valve disease. 2003 Sep:12(5):577-81 [PubMed PMID: 14565709]
Level 2 (mid-level) evidenceFerretti JJ, Stevens DL, Fischetti VA, Sika-Paotonu D, Beaton A, Raghu A, Steer A, Carapetis J. Acute Rheumatic Fever and Rheumatic Heart Disease. Streptococcus pyogenes: Basic Biology to Clinical Manifestations. 2016:(): [PubMed PMID: 28379675]
Harari R, Bansal P, Yatskar L, Rubinstein D, Silbiger JJ. Papillary muscle rupture following acute myocardial infarction: Anatomic, echocardiographic, and surgical insights. Echocardiography (Mount Kisco, N.Y.). 2017 Nov:34(11):1702-1707. doi: 10.1111/echo.13739. Epub 2017 Oct 29 [PubMed PMID: 29082549]
Burton LV, Beier K. Papillary Muscle Rupture. StatPearls. 2024 Jan:(): [PubMed PMID: 29763151]
Varma PK, Krishna N, Jose RL, Madkaiker AN. Ischemic mitral regurgitation. Annals of cardiac anaesthesia. 2017 Oct-Dec:20(4):432-439. doi: 10.4103/aca.ACA_58_17. Epub [PubMed PMID: 28994679]
Patel JB, Borgeson DD, Barnes ME, Rihal CS, Daly RC, Redfield MM. Mitral regurgitation in patients with advanced systolic heart failure. Journal of cardiac failure. 2004 Aug:10(4):285-91 [PubMed PMID: 15309693]
Gertz ZM, Raina A, Saghy L, Zado ES, Callans DJ, Marchlinski FE, Keane MG, Silvestry FE. Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control. Journal of the American College of Cardiology. 2011 Sep 27:58(14):1474-81. doi: 10.1016/j.jacc.2011.06.032. Epub [PubMed PMID: 21939832]
Level 2 (mid-level) evidenceHerrmann HC, Gertz ZM, Silvestry FE, Wiegers SE, Woo YJ, Hermiller J, Segar D, Heimansohn D, Gray W, Homma S, Argenziano M, Wang A, Jollis J, Lampert MB, Alexander J, Mauri L, Foster E, Glower D, Feldman T. Effects of atrial fibrillation on treatment of mitral regurgitation in the EVEREST II (Endovascular Valve Edge-to-Edge Repair Study) randomized trial. Journal of the American College of Cardiology. 2012 Apr 3:59(14):1312-9. doi: 10.1016/j.jacc.2011.12.023. Epub [PubMed PMID: 22464260]
Level 1 (high-level) evidenceHwang HJ, Choi EY, Kwan J, Kim SA, Shim CY, Ha JW, Rim SJ, Chung N, Kim SS. Dynamic change of mitral apparatus as potential cause of left ventricular outflow tract obstruction in hypertrophic cardiomyopathy. European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2011 Jan:12(1):19-25. doi: 10.1093/ejechocard/jeq092. Epub 2010 Aug 7 [PubMed PMID: 20693545]
Freed LA, Levy D, Levine RA, Larson MG, Evans JC, Fuller DL, Lehman B, Benjamin EJ. Prevalence and clinical outcome of mitral-valve prolapse. The New England journal of medicine. 1999 Jul 1:341(1):1-7 [PubMed PMID: 10387935]
Level 2 (mid-level) evidenceMoraes RC, Katz M, Tarasoutchi F. Clinical and epidemiological profile of patients with valvular heart disease admitted to the emergency department. Einstein (Sao Paulo, Brazil). 2014 Apr:12(2):154-8 [PubMed PMID: 25003918]
Level 2 (mid-level) evidenceNkomo VT. Epidemiology and prevention of valvular heart diseases and infective endocarditis in Africa. Heart (British Cardiac Society). 2007 Dec:93(12):1510-9 [PubMed PMID: 18003682]
Maganti K, Rigolin VH, Sarano ME, Bonow RO. Valvular heart disease: diagnosis and management. Mayo Clinic proceedings. 2010 May:85(5):483-500. doi: 10.4065/mcp.2009.0706. Epub [PubMed PMID: 20435842]
Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. The New England journal of medicine. 2005 Mar 3:352(9):875-83 [PubMed PMID: 15745978]
Thomas SL, Heaton J, Makaryus AN. Physiology, Cardiovascular Murmurs. StatPearls. 2024 Jan:(): [PubMed PMID: 30247833]
DePace NL, Nestico PF, Morganroth J. Acute severe mitral regurgitation. Pathophysiology, clinical recognition, and management. The American journal of medicine. 1985 Feb:78(2):293-306 [PubMed PMID: 3881945]
Level 3 (low-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017 Jun 20:135(25):e1159-e1195. doi: 10.1161/CIR.0000000000000503. Epub 2017 Mar 15 [PubMed PMID: 28298458]
Level 1 (high-level) evidenceGrayburn PA, Carabello B, Hung J, Gillam LD, Liang D, Mack MJ, McCarthy PM, Miller DC, Trento A, Siegel RJ. Defining "severe" secondary mitral regurgitation: emphasizing an integrated approach. Journal of the American College of Cardiology. 2014 Dec 30:64(25):2792-801. doi: 10.1016/j.jacc.2014.10.016. Epub [PubMed PMID: 25541133]
Zeng X, Levine RA, Hua L, Morris EL, Kang Y, Flaherty M, Morgan NV, Hung J. Diagnostic value of vena contracta area in the quantification of mitral regurgitation severity by color Doppler 3D echocardiography. Circulation. Cardiovascular imaging. 2011 Sep:4(5):506-13. doi: 10.1161/CIRCIMAGING.110.961649. Epub 2011 Jul 5 [PubMed PMID: 21730026]
Level 2 (mid-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, ACC/AHA Task Force Members. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 10:129(23):2440-92. doi: 10.1161/CIR.0000000000000029. Epub 2014 Mar 3 [PubMed PMID: 24589852]
Level 1 (high-level) evidenceDudzinski DM, Hung J. Echocardiographic assessment of ischemic mitral regurgitation. Cardiovascular ultrasound. 2014 Nov 21:12():46. doi: 10.1186/1476-7120-12-46. Epub 2014 Nov 21 [PubMed PMID: 25416497]
Uretsky S, Argulian E, Narula J, Wolff SD. Use of Cardiac Magnetic Resonance Imaging in Assessing Mitral Regurgitation: Current Evidence. Journal of the American College of Cardiology. 2018 Feb 6:71(5):547-563. doi: 10.1016/j.jacc.2017.12.009. Epub [PubMed PMID: 29406861]
Mehta NK, Kim J, Siden JY, Rodriguez-Diego S, Alakbarli J, Di Franco A, Weinsaft JW. Utility of cardiac magnetic resonance for evaluation of mitral regurgitation prior to mitral valve surgery. Journal of thoracic disease. 2017 Apr:9(Suppl 4):S246-S256. doi: 10.21037/jtd.2017.03.54. Epub [PubMed PMID: 28540067]
Abdel Fattah EM, Girgis HY, El Khashab K, Ashour ZA, Ezzat GM. B-type Natriuretic Peptide as an Index of Symptoms and Severity of Chronic Rheumatic Mitral Regurgitation. Heart views : the official journal of the Gulf Heart Association. 2016 Jan-Mar:17(1):7-12. doi: 10.4103/1995-705X.182648. Epub [PubMed PMID: 27293523]
Borer JS, Sharma A. Drug Therapy for Heart Valve Diseases. Circulation. 2015 Sep 15:132(11):1038-45. doi: 10.1161/CIRCULATIONAHA.115.016006. Epub [PubMed PMID: 26371236]
Harris KM, Pastorius CA, Duval S, Harwood E, Henry TD, Carabello BA, Hirsch AT. Practice variation among cardiovascular physicians in management of patients with mitral regurgitation. The American journal of cardiology. 2009 Jan 15:103(2):255-61. doi: 10.1016/j.amjcard.2008.09.065. Epub 2008 Nov 12 [PubMed PMID: 19121447]
WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15:128(16):e240-327. doi: 10.1161/CIR.0b013e31829e8776. Epub 2013 Jun 5 [PubMed PMID: 23741058]
Level 3 (low-level) evidenceStrauss CE, Duval S, Pastorius D, Harris KM. Pharmacotherapy in the treatment of mitral regurgitation: a systematic review. The Journal of heart valve disease. 2012 May:21(3):275-85 [PubMed PMID: 22808826]
Level 1 (high-level) evidenceBonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS, 2006 Writing Committee Members, American College of Cardiology/American Heart Association Task Force. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008 Oct 7:118(15):e523-661. doi: 10.1161/CIRCULATIONAHA.108.190748. Epub 2008 Sep 26 [PubMed PMID: 18820172]
Level 1 (high-level) evidenceSampaio RO, Grinberg M, Leite JJ, Tarasoutchi F, Chalela WA, Izaki M, Spina GS, Rossi EG, Mady C. Effect of enalapril on left ventricular diameters and exercise capacity in asymptomatic or mildly symptomatic patients with regurgitation secondary to mitral valve prolapse or rheumatic heart disease. The American journal of cardiology. 2005 Jul 1:96(1):117-21 [PubMed PMID: 15979448]
Level 1 (high-level) evidenceSupino PG, Khan N, Hai O, Herrold EM, Hochreiter C, Borer JS. Relation of indirect vasodilator use to prognosis in patients with chronic severe mitral regurgitation. Cardiology. 2014:129(4):262-6. doi: 10.1159/000368797. Epub 2014 Nov 15 [PubMed PMID: 25402846]
Level 2 (mid-level) evidenceSlipczuk L, Rafique AM, Davila CD, Beigel R, Pressman GS, Siegel RJ. The Role of Medical Therapy in Moderate to Severe Degenerative Mitral Regurgitation. Reviews in cardiovascular medicine. 2016:17(1-2):28-39. doi: 10.3909/ricm0835. Epub [PubMed PMID: 27667378]
Varadarajan P, Joshi N, Appel D, Duvvuri L, Pai RG. Effect of Beta-blocker therapy on survival in patients with severe mitral regurgitation and normal left ventricular ejection fraction. The American journal of cardiology. 2008 Sep 1:102(5):611-5. doi: 10.1016/j.amjcard.2008.04.029. Epub 2008 Jun 17 [PubMed PMID: 18721522]
Level 2 (mid-level) evidenceComin-Colet J, Sánchez-Corral MA, Manito N, Gómez-Hospital JA, Roca J, Fernández-Nofrerias E, Valdovinos P, Esplugas E. Effect of carvedilol therapy on functional mitral regurgitation, ventricular remodeling, and contractility in patients with heart failure due to left ventricular systolic dysfunction. Transplantation proceedings. 2002 Feb:34(1):177-8 [PubMed PMID: 11959238]
Stout KK, Verrier ED. Acute valvular regurgitation. Circulation. 2009 Jun 30:119(25):3232-41. doi: 10.1161/CIRCULATIONAHA.108.782292. Epub [PubMed PMID: 19564568]
Madesis A, Tsakiridis K, Zarogoulidis P, Katsikogiannis N, Machairiotis N, Kougioumtzi I, Kesisis G, Tsiouda T, Beleveslis T, Koletas A, Zarogoulidis K. Review of mitral valve insufficiency: repair or replacement. Journal of thoracic disease. 2014 Mar:6 Suppl 1(Suppl 1):S39-51. doi: 10.3978/j.issn.2072-1439.2013.10.20. Epub [PubMed PMID: 24672698]
O'Gara PT, Grayburn PA, Badhwar V, Afonso LC, Carroll JD, Elmariah S, Kithcart AP, Nishimura RA, Ryan TJ, Schwartz A, Stevenson LW. 2017 ACC Expert Consensus Decision Pathway on the Management of Mitral Regurgitation: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. Journal of the American College of Cardiology. 2017 Nov 7:70(19):2421-2449. doi: 10.1016/j.jacc.2017.09.019. Epub 2017 Oct 18 [PubMed PMID: 29055505]
Level 3 (low-level) evidenceSharma A, Agrawal S, Goel S, Borer JS. Surgical Treatment of Ischemic Mitral Regurgitation: Valve Repair Versus Replacement. Current cardiology reports. 2017 Jan:19(1):3. doi: 10.1007/s11886-017-0813-6. Epub [PubMed PMID: 28101839]
Andalib A, Chetrit M, Eberg M, Filion KB, Thériault-Lauzier P, Lange R, Buithieu J, Martucci G, Eisenberg M, Bolling SF, Piazza N. A Systematic Review and Meta-Analysis of Outcomes Following Mitral Valve Surgery in Patients with Significant Functional Mitral Regurgitation and Left Ventricular Dysfunction. The Journal of heart valve disease. 2016 Nov:25(6):696-707 [PubMed PMID: 28290169]
Level 1 (high-level) evidenceAlegria-Barrero E, Franzen OW. Mitral Regurgitation - A Multidisciplinary Challenge. European cardiology. 2014 Jul:9(1):49-53. doi: 10.15420/ecr.2014.9.1.49. Epub [PubMed PMID: 30310485]
Katz WE, Conrad Smith AJ, Crock FW, Cavalcante JL. Echocardiographic evaluation and guidance for MitraClip procedure. Cardiovascular diagnosis and therapy. 2017 Dec:7(6):616-632. doi: 10.21037/cdt.2017.07.04. Epub [PubMed PMID: 29302467]
Dziadzko V, Clavel MA, Dziadzko M, Medina-Inojosa JR, Michelena H, Maalouf J, Nkomo V, Thapa P, Enriquez-Sarano M. Outcome and undertreatment of mitral regurgitation: a community cohort study. Lancet (London, England). 2018 Mar 10:391(10124):960-969. doi: 10.1016/S0140-6736(18)30473-2. Epub [PubMed PMID: 29536860]
Lindmark K, Söderberg S, Teien D, Näslund U. Long-term follow-up of mitral valve regurgitation--importance of mitral valve pathology and left ventricular function on survival. International journal of cardiology. 2009 Oct 2:137(2):145-50. doi: 10.1016/j.ijcard.2008.06.037. Epub 2008 Aug 15 [PubMed PMID: 18707770]
Tomšič A, Hiemstra YL, van Hout FMA, van Brakel TJ, Versteegh MIM, Marsan NA, Klautz RJM, Palmen M. Long-term results of mitral valve repair for severe mitral regurgitation in asymptomatic patients. Journal of cardiology. 2018 Dec:72(6):473-479. doi: 10.1016/j.jjcc.2018.04.016. Epub 2018 May 31 [PubMed PMID: 29861131]
Costa FDAD, Colatusso DFF, Martin GLDS, Parra KCS, Botta MC, Balbi Filho EM, Veloso M, Miotto G, Ferreira ADA, Colatusso C. Long-Term Results of Mitral Valve Repair. Brazilian journal of cardiovascular surgery. 2018 Jan-Feb:33(1):23-31. doi: 10.21470/1678-9741-2017-0145. Epub [PubMed PMID: 29617498]
Toledano K, Rudski LG, Huynh T, Béïque F, Sampalis J, Morin JF. Mitral regurgitation: determinants of referral for cardiac surgery by Canadian cardiologists. The Canadian journal of cardiology. 2007 Mar 1:23(3):209-14 [PubMed PMID: 17347692]
Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). European heart journal. 2012 Oct:33(19):2451-96. doi: 10.1093/eurheartj/ehs109. Epub 2012 Aug 24 [PubMed PMID: 22922415]
Butchart EG, Gohlke-Bärwolf C, Antunes MJ, Tornos P, De Caterina R, Cormier B, Prendergast B, Iung B, Bjornstad H, Leport C, Hall RJ, Vahanian A, Working Groups on Valvular Heart Disease, Thrombosis, and Cardiac Rehabilitation and Exercise Physiology, European Society of Cardiology. Recommendations for the management of patients after heart valve surgery. European heart journal. 2005 Nov:26(22):2463-71 [PubMed PMID: 16103039]
Seiler C. Management and follow up of prosthetic heart valves. Heart (British Cardiac Society). 2004 Jul:90(7):818-24 [PubMed PMID: 15201262]
Sibilitz KL, Berg SK, Rasmussen TB, Risom SS, Thygesen LC, Tang L, Hansen TB, Johansen PP, Gluud C, Lindschou J, Schmid JP, Hassager C, Køber L, Taylor RS, Zwisler AD. Cardiac rehabilitation increases physical capacity but not mental health after heart valve surgery: a randomised clinical trial. Heart (British Cardiac Society). 2016 Dec 15:102(24):1995-2003. doi: 10.1136/heartjnl-2016-309414. Epub 2016 Aug 4 [PubMed PMID: 27492941]
Level 1 (high-level) evidenceMeurin P, Iliou MC, Ben Driss A, Pierre B, Corone S, Cristofini P, Tabet JY, Working Group of Cardiac Rehabilitation of the French Society of Cardiology. Early exercise training after mitral valve repair: a multicentric prospective French study. Chest. 2005 Sep:128(3):1638-44 [PubMed PMID: 16162769]
Pollmann AGE, Frederiksen M, Prescott E. Cardiac Rehabilitation After Heart Valve Surgery: IMPROVEMENT IN EXERCISE CAPACITY AND MORBIDITY. Journal of cardiopulmonary rehabilitation and prevention. 2017 May:37(3):191-198. doi: 10.1097/HCR.0000000000000208. Epub [PubMed PMID: 27755256]
Sibilitz KL, Berg SK, Tang LH, Risom SS, Gluud C, Lindschou J, Kober L, Hassager C, Taylor RS, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. The Cochrane database of systematic reviews. 2016 Mar 21:3():CD010876. doi: 10.1002/14651858.CD010876.pub2. Epub 2016 Mar 21 [PubMed PMID: 26998683]
Level 1 (high-level) evidenceLunel C, Laurent M, Corbineau H, Boulmier D, Chaperon J, Guillo P, Dewitte JD, Leguerrier A. [Return to work after cardiac valvular surgery. Retrospective study of a series of 105 patients]. Archives des maladies du coeur et des vaisseaux. 2003 Jan:96(1):15-22 [PubMed PMID: 12613145]
Level 2 (mid-level) evidenceZhuge RQ, Hou XP, Qi XL, Wu YJ, Zhang MZ. Clinical features and treatment options for mitral regurgitation in elderly inpatients. Journal of geriatric cardiology : JGC. 2018 Jun:15(6):428-433. doi: 10.11909/j.issn.1671-5411.2018.06.005. Epub [PubMed PMID: 30108615]
Level 2 (mid-level) evidenceMirabel M, Iung B, Baron G, Messika-Zeitoun D, Détaint D, Vanoverschelde JL, Butchart EG, Ravaud P, Vahanian A. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? European heart journal. 2007 Jun:28(11):1358-65 [PubMed PMID: 17350971]
Heuts S, Olsthoorn JR, Hermans SMM, Streukens SAF, Vainer J, Cheriex EC, Segers P, Maessen JG, Sardari Nia P. Multidisciplinary decision-making in mitral valve disease: the mitral valve heart team. Netherlands heart journal : monthly journal of the Netherlands Society of Cardiology and the Netherlands Heart Foundation. 2019 Apr:27(4):176-184. doi: 10.1007/s12471-019-1238-1. Epub [PubMed PMID: 30742250]