Introduction
The oral cavity, or more commonly known as the mouth or buccal cavity, serves as the first portion of the digestive system. It consists of several different anatomically different aspects that work together effectively and efficiently to perform several functions. These aspects include the lips, tongue, palate, and teeth. Although a small compartment, the oral cavity is a unique and complex structure with several different nerves and blood vessels inside it. This intricate network is necessary for its unique and diverse role in human life.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
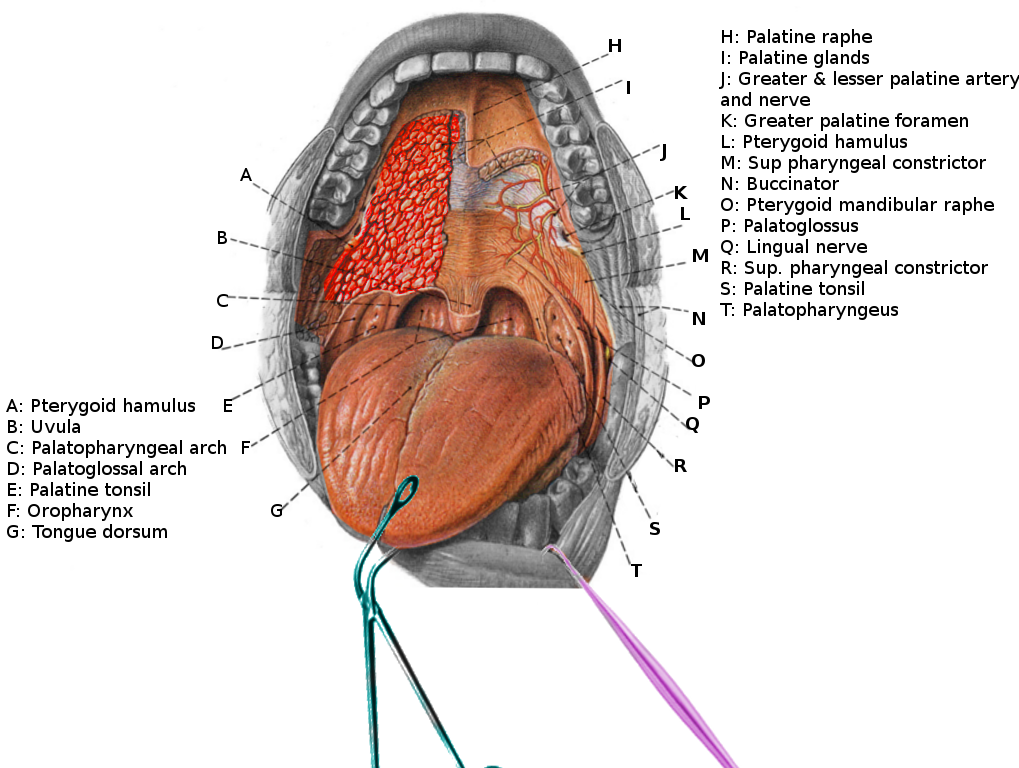
The oral cavity is surrounded by the lips and is composed of two separate regions, the vestibule, the area between the cheeks, teeth, and lips, and the oral cavity proper. The oral cavity proper is mostly filled with the tongue and bounded anteriorly and on the sides by the alveolar processes containing the teeth and posteriorly by the isthmus of the fauces. Anteriorly, the roof forms by the hard palate and posteriorly by the soft palate. The uvula hangs downwards from the soft palate. The mylohyoid muscles constitute the floor of the oral cavity proper. A mucous membrane known as the oral mucosa is composed of stratified squamous epithelium and forms the inner lining of the mouth. Several submandibular and sublingual salivary glands secrete viscous and mucoid fluid to lubricate and keep the oral cavity moist.
The mouth not only plays a vital role in the initial intake and digestion of food and water but also is essential for the formation of speech and normal respiration. The teeth, which are the chief structures of the oral cavity, tear and grind ingested food into pieces small enough for digestion. The tongue enables the digestion of food through compressing and pressing food against the palates; this leads to the formation of the food bolus subsequently swallowed down the esophagus.[1] The tongue also functions to provide the perception of taste to humans as it contains various papillae on its dorsal surface that serve as taste buds. Moreover, the tongue is the most important articulator of speech, as it manipulates itself against the teeth and palate to form words. The palate serves as a mechanical barrier separating the oral cavity from the nasal respiratory tract, also enabling simultaneous breathing and food intake.
Embryology
The oral cavity is a unique structure in that it forms from both ectodermal and endodermal structures.[2]
The tongue's embryological component derives from several different pharyngeal arches, each contributing towards the development of a different region of the tongue. In the fifth week of development, swellings, known as "lingual swellings," develop on the right and left sides of the first pharyngeal arch. These grow and develop to become the anterior two-thirds of the tongue. The groove which marks the area of fusion between the two lingual swellings is known as the median sulcus. The posterior one-third of the tongue forms by the copula, a swelling that forms from the second pharyngeal arch, the second and third pharyngeal arches, and a small portion of the fourth pharyngeal arch. The boundary between the anterior and posterior portions of the tongue is a V-shaped groove known as the terminal sulcus.
The palate consists of primary and secondary embryological origins and forms between the sixth and twelfth week. The primary palate arises from the embryonic frontonasal prominences and contains the philtrum, upper incisors region, and anterior upper jaw. The secondary palate forms from the paired maxillary prominences fusion and contains the rest of the hard and soft palate. These palatal outgrowths then expand vertically to become palatal shelves. These shelves elevate horizontally above the dorsum of the tongue and fuse with the primary palate and nasal septum to form the intact roof of the oral cavity.[3]
The upper lip form during early embryogenesis from the maxillary, lateral nasal, and medial nasal facial prominences. These facial prominences develop from anteriorly migrating neural crest cells in combination with mesoderm and the head ectoderm. They then undergo growth and expansion, eventually leading to their fusion and the formation of facial structures.[4] The mandibular processes fuse to form the lower lip.
Blood Supply and Lymphatics
Different branches of the external carotid artery provide blood supply to the oral cavity. The lingual artery provides significant vascular supply to the oral tongue.[5] The hard palate receives supply by the greater palatine and superior alveolar arteries.[6] The alveolar arteries arise from the terminal branches of the maxillary artery and also provide blood supply to the gingiva and upper dentition. The vascular supply to the lips are the labial arteries that come off of the facial artery. Finally, the lower dentition and mandible are supplied by the inferior alveolar artery, which enters the mandibular foramen along the medial aspect of the ramus of the mandible along with the inferior alveolar nerve.[7]
Nerves
The innervation of the oral cavity is distinct and comes primarily from the maxillary and mandibular divisions of the trigeminal nerve.
The oral mucosa, teeth, and supporting structures receive their innervation from the maxillary and mandibular divisions of the trigeminal nerve.
The greater palatine and nasopalatine nerves both branches of the maxillary nerve innervate the hard palate, whereas the lesser palatine branch of the maxillary nerve supplies the soft palate.
The innervation of the tongue is complex. Motor innervation of all intrinsic and extrinsic muscles, except for the palatoglossus comes from the hypoglossal nerve. The palatoglossus receives innervation from the vagus nerve. The anterior and posterior portions of the tongue have different taste and sensory innervation due to their different embryological origins. The anterior two-thirds of the tongue receives taste sensation by a branch of the facial nerve called the chorda tympani nerve whereas the general sensation of the anterior two-third tongue is by the lingual nerve, which is a branch of the mandibular branch of trigeminal. The posterior one-third of the tongue gets both its sensory and taste sensations from the glossopharyngeal nerve.[1]
The buccal nerve, also a branch of the mandibular division of the trigeminal nerve innervates the cheek.
Muscles
There are several muscles inside the oral cavity. The floor of the oral cavity is made up of the mylohyoid and geniohyoid, which act in the elevation of the hyoid-laryngeal complex during swallowing.[8] The superior border of the oral cavity includes the soft palate that is made up of five different muscles: tensor veli palatini, musculus uvulae, levator veli palatini, palatopharyngeus, palatoglossus. All these muscles receive innervation from the pharyngeal branch of the vagus nerve except tensor veli palatini, which is innervated by the mandibular branch of the trigeminal nerve.[9]
Clinical Significance
Squamous Cell Carcinoma of the Oral Cavity (SCCOC)
Squamous cell carcinoma constitutes more than 90% of all oral cancers. Tobacco smoking and alcohol are the main etiological factors in SCC of the mouth. Tobacco contains carcinogenic molecules, and research has shown a directly proportional effect between pack-years of tobacco and the risk of SCCOC. Patients typically present in late stage. Standard of care is primary surgical resection with or without postoperative adjuvant therapy depending on how invasive the lesion is. Primary and secondary prevention requires early education about lifestyle risk in factors and improved awareness for early diagnosis.[10] It can initially present as leukoplakia, a white patch on the buccal mucosa that will not rub off; this is precancerous and should undergo biopsy.[11] The anatomy of the oral cavity plays a huge role in the surgical management of oral cancers. For premalignant lesions or small superficial cancers, a transoral approach is an option for removal of tumors of the anterior floor of mouth, alveolus, and tongue. Posteriorly located tumors must be treated invasively due to inadequate surgical field exposure. Lip splitting paramedial mandibulotomy approach is in which an incision is made through the lips and mandible, exposing the posterior lateral aspect of the oral cavity. Upper cheek flaps and midfacial degloving may also be options for maxillary lesions.[10]
Media
References
Dotiwala AK, Samra NS. Anatomy, Head and Neck, Tongue. StatPearls. 2023 Jan:(): [PubMed PMID: 29939559]
Chen J, Jacox LA, Saldanha F, Sive H. Mouth development. Wiley interdisciplinary reviews. Developmental biology. 2017 Sep:6(5):. doi: 10.1002/wdev.275. Epub 2017 May 17 [PubMed PMID: 28514120]
Li C, Lan Y, Jiang R. Molecular and Cellular Mechanisms of Palate Development. Journal of dental research. 2017 Oct:96(11):1184-1191. doi: 10.1177/0022034517703580. Epub 2017 Jul 26 [PubMed PMID: 28745929]
Jiang R, Bush JO, Lidral AC. Development of the upper lip: morphogenetic and molecular mechanisms. Developmental dynamics : an official publication of the American Association of Anatomists. 2006 May:235(5):1152-66 [PubMed PMID: 16292776]
Level 3 (low-level) evidenceMun MJ, Lee CH, Lee BJ, Lee JC, Jang JY, Jung SH, Wang SG. Histopathologic Evaluations of the Lingual Artery in Healthy Tongue of Adult Cadaver. Clinical and experimental otorhinolaryngology. 2016 Sep:9(3):257-62. doi: 10.21053/ceo.2015.01137. Epub 2016 Jun 18 [PubMed PMID: 27334510]
Shahbazi A, Grimm A, Feigl G, Gerber G, Székely AD, Molnár B, Windisch P. Analysis of blood supply in the hard palate and maxillary tuberosity-clinical implications for flap design and soft tissue graft harvesting (a human cadaver study). Clinical oral investigations. 2019 Mar:23(3):1153-1160. doi: 10.1007/s00784-018-2538-3. Epub 2018 Jul 1 [PubMed PMID: 29961140]
Jergenson MA, Norton NS, Opack JM, Barritt LC. Unique origin of the inferior alveolar artery. Clinical anatomy (New York, N.Y.). 2005 Nov:18(8):597-601 [PubMed PMID: 16187317]
Level 3 (low-level) evidenceCosta MMB. NEURAL CONTROL OF SWALLOWING. Arquivos de gastroenterologia. 2018 Nov:55Suppl 1(Suppl 1):61-75. doi: 10.1590/S0004-2803.201800000-45. Epub 2018 Aug 23 [PubMed PMID: 30156597]
Logjes RJ, Bleys RL, Breugem CC. The innervation of the soft palate muscles involved in cleft palate: a review of the literature. Clinical oral investigations. 2016 Jun:20(5):895-901. doi: 10.1007/s00784-016-1791-6. Epub 2016 Mar 29 [PubMed PMID: 27020913]
Montero PH, Patel SG. Cancer of the oral cavity. Surgical oncology clinics of North America. 2015 Jul:24(3):491-508. doi: 10.1016/j.soc.2015.03.006. Epub 2015 Apr 15 [PubMed PMID: 25979396]
Walker HK, Hall WD, Hurst JW, Walker WB. The Oral Cavity and Associated Structures. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250078]