Introduction
Nasolacrimal duct obstruction (NLDO) or dacryostenosis is the most common disorder of the lacrimal system.[1] Approximately 6% to 20% of newborns patients present with some symptoms.[2] Typically, NLDO presents more often in the first weeks or months of life with symptoms beginning when normal tear production occurs, presenting as excessive tearing and ocular discharge. Erythema of the periorbital skin, upper and lower eyelids may result from irritation and rubbing produced by dripping of tears and discharge due to inadequate drainage. As a result, the condition may be apparent as chronic unilateral conjunctivitis. Most the cases resolved spontaneously or with minimal intervention by the first year of life; however, unresolved cases need to be referred to the pediatric ophthalmologist for probing and may require surgical intervention. In children younger than 6 months of age, a conservative approach is a typical management. Massaging the lacrimal sac, eye drops, and topical antibiotics are commonly used, and surgical treatment is considered for patients whose symptoms persist after 12 months of age.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The lacrimal drainage structures form during the fifth week of gestation as a crease between the frontons and maxillary processes, known as the nasolacrimal groove or naso-optic fissure 10. A cord of ectodermal tissues separates from the surface and enters this groove. This tissue eventually canalizes and forms the lacrimal sac and nasolacrimal duct. This process of canalization usually begins by week 8 and is completed by birth. Tears are produced by the main and accessory lacrimal glands and drain medially into the puncta, then flow through the canaliculi to the lacrimal sac, and then through the nasolacrimal duct into the nose. Incomplete canalization is the most common cause of congenital nasolacrimal duct obstruction (NLDO) and occurs at the distal end resulting in an imperforate membrane at the valve of Hasner.[4]
Epidemiology
The prevalence of this condition is approximately 6% to 20% in infants. There is a high rate of spontaneous resolution of congenital nasolacrimal duct obstruction with approximately 70% of affected children being free of the symptoms by 3 months of age, and over 90% recovering by their first birthday. In one study, 20% of healthy infants showed evidence of defective lacrimal drainage during the first year of life. Spontaneous resolution occurs by 6 months of age in approximately 90% of infants with congenital nasolacrimal duct obstruction (NLDO). From those infants with persistent symptoms at 6 to 10 months of age, approximately two-thirds have a resolution within 6 months. The cases that persist beyond 12 months of age are likely to require probing of the lacrimal duct. A study showed that those patients with significant nasolacrimal obstruction, meaning nonresponsive to two or more probing procedures, with or without intubation, 35% have nasolacrimal duct obstruction, 15% have punctal agenesis, 10% have congenital fistulas, and 5% have craniofacial defects.[5] The condition affects males and females equally. It has reported no difference in the racial incidence of congenital nasolacrimal system abnormalities.
Infants at increased risk for this condition include those with trisomy 21, ectrodactyly-ectodermal dysplasia-cleft lip/palate (EEC) syndrome, branchiooculofacial syndrome, CHARGE (coloboma, heart anomaly, choanal atresia, and retardation, genital and ear anomalies) syndrome, and Goldenhar syndrome.
History and Physical
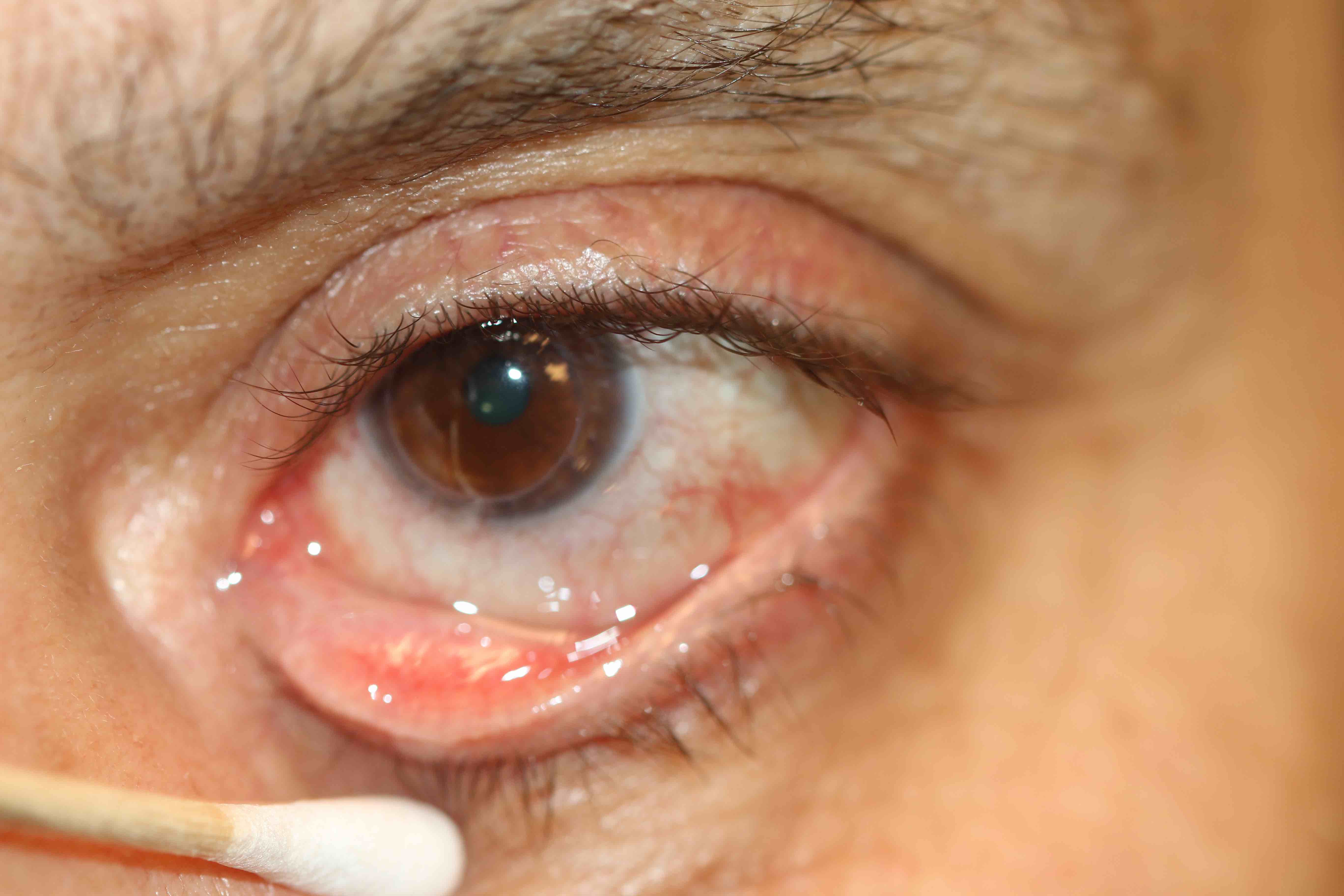
Infants with congenital nasolacrimal duct obstruction (NLDO) present with a history of chronic or intermittent tearing and debris on the eyelashes. Conjunctival erythema is not characteristic although irritation from overflow tearing and chronic rubbing of the eyes may cause mild redness of the lower and upper eyelid. On physical examination, there is usually an increase in the size of the tear meniscus. Palpation of the lacrimal sac may cause reflux of tears and/or mucoid discharge onto the eye through the puncta.
Congenital nasolacrimal anomalies, particularly obstruction, can lead to various clinical manifestations including infection due to stasis of fluid within the lacrimal system. Obstruction can partially allow the duct to drain the tears produced, except in situations where increased tear production is present (wind, cold weather) and tear overflow results. The normal flora bacteria usually present within the tears do not cause problems because they are flushed readily into the nares. In NLDO, the stasis of fluid within the lacrimal sac creates a moist, warm environment favorable to bacterial growth.
A few infants with NLDO present within the first few weeks of life with a more severe infection: acute dacryocystitis. Clinical findings include edema and erythema with distension of the lacrimal sac below the medial canthal tendon, and patients may have systemic signs of infection such as fever and irritability. This is a rare complication of isolated congenital NLDO. Acute dacryocystitis can be complicated by preseptal or orbital cellulitis, sepsis, or meningitis and should be treated promptly with systemic antibiotics. Although antibiotic therapy is frequently prescribed for dacryocystitis, the definitive treatment of dacryocystitis is usually surgical.
Evaluation
Diagnosis is typically made by history and physical examination alone. If symptoms are intermittent and signs of abnormal tearing or "mattering" are not present at the time of examination, the dye disappearance test can be performed to help confirm the diagnosis. Begin by placing one drop of fluorescein-stained saline in the inferior cul-de-sac of the patient's eyes and wipe away excess tears from the eyelids. Wait 5 minutes and inspect the eyes. The fluorescein should drain completely into the nose within 5 minutes if the lacrimal drainage system has no obstruction.
Treatment / Management
The primary treatment of uncomplicated nasolacrimal duct obstruction (NLDO) is a regimen of nasolacrimal massage, usually 2 to 3 times per day, accompanied by a cleansing of the lids with warm water and topical antibiotics; this will resolve the infection in 76% to 89% of cases.[6][7][8] Topical antibiotics are used for control of mucopurulent drainage, and a bland ophthalmic ointment may be used on the eyelids if the skin is macerated. In cases that do not resolve by age 6 to 10 months, lacrimal duct probing is performed by pediatric ophthalmology in the office (Bowman probe) or in the operating room (intranasal cysts or infection), depending on the age of the child.[9] During the procedure the physician inserts a probe or irrigation cannula and advances it through the lacrimal drainage system until it touches the obstruction; the probe is then pushed through the obstruction into the nose. Irrigation with fluorescein-stained saline is often achieved to warrant patency. If concomitant infection or cellulitis is present, systemic antibiotics should be used first, then probing is done. The advantages of early probing in the office setting are avoidance of general anesthesia, speedy resolution of symptoms, fewer physician visits, fewer antibiotic prescriptions, and less costly procedures.(A1)
Differential Diagnosis
The differential diagnosis is broad and includes conjunctivitis, corneal abrasion, uveitis hemangiomas, dermoids, nasal gliomas, and infantile glaucoma. The absence of associated signs and symptoms distinguishes congenital nasolacrimal duct obstruction (NLDO) from other causes of persistent tearing.
Most infants with congenital NLDO can be diagnosed and managed by the primary care practitioner. Referral to an ophthalmologist is warranted if the diagnosis is uncertain, particularly if there is any concern of glaucoma or signs or symptoms of dacryocystitis or dacryocystocele.
Enhancing Healthcare Team Outcomes
Infants with nasolacrimal duct obstruction initially present to the pediatrician, nurse practitioner or the primary care provider. It is important to refer these patients to an ophthalmologist for further workup because there are many causes. The ophthalmic nurse should educate the caregiver on home care management; the primary treatment of uncomplicated nasolacrimal duct obstruction (NLDO) is a regimen of nasolacrimal massage, usually 2 to 3 times per day, accompanied by a cleansing of the lids with warm water and topical antibiotics; this will resolve the infection in 76% to 89% of cases. When the conservative methods fail to relieve the obstruction, some type of surgery procedure is performed to relieve the blockage. The advantages of early probing in the office setting are avoidance of general anesthesia, speedy resolution of symptoms, fewer physician visits, fewer antibiotic prescriptions, and less costly procedures.
Media
(Click Image to Enlarge)
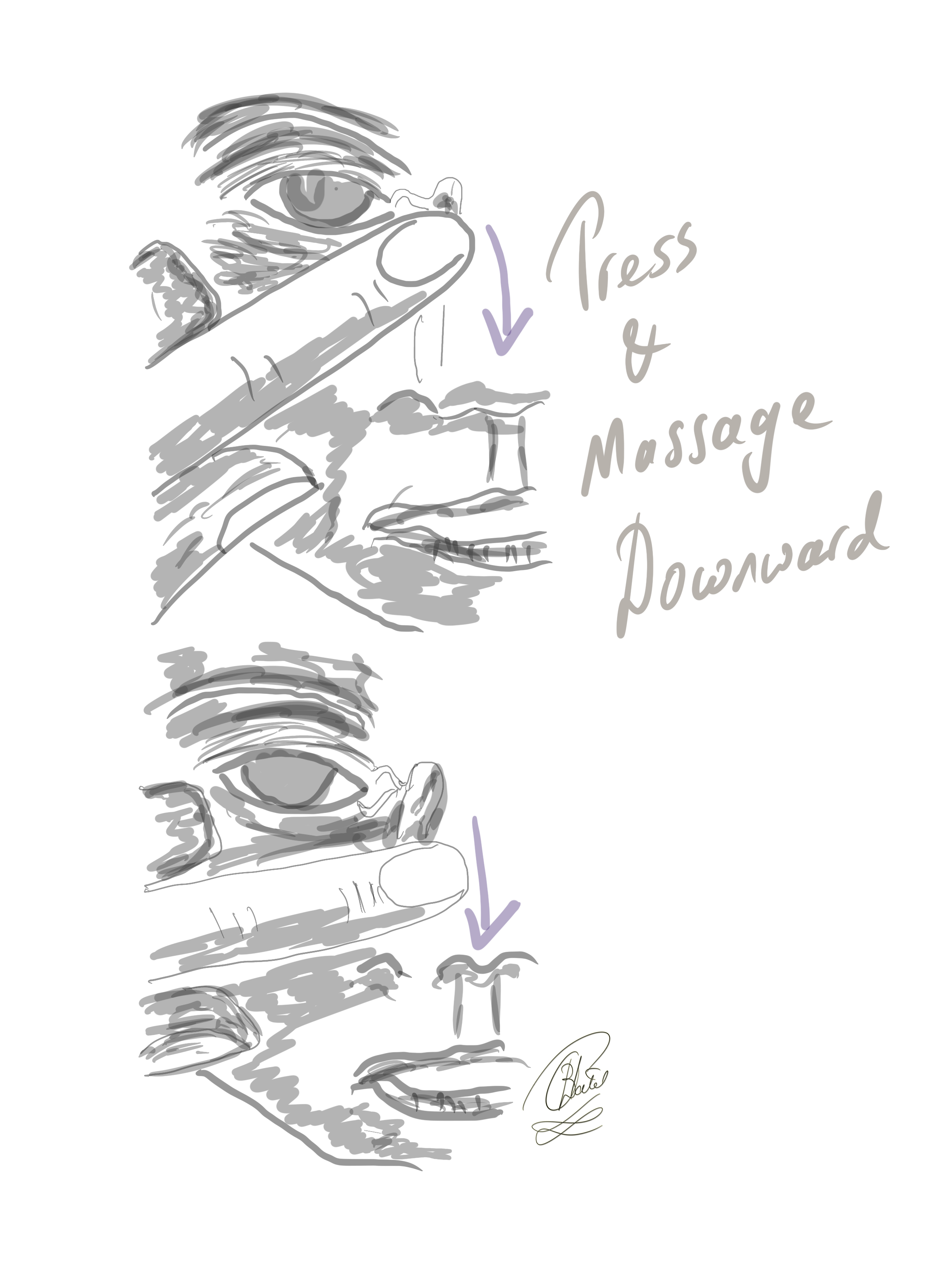
The Crigler Maneuver for Congenital Nasolacrimal Duct Obstruction. In this technique, the finger is inwardly pressed against the lacrimal sac, and the massaging movement is directed downward to elevate hydrostatic pressure within the lacrimal sac and the nasolacrimal duct.
Contributed by BCK Patel, MD, FRCS
(Click Video to Play)
(Click Image to Enlarge)
References
Ffooks OO. DACRYOCYSTITIS IN INFANCY. The British journal of ophthalmology. 1962 Jul:46(7):422-34 [PubMed PMID: 18170798]
GUERRY D 3rd, KENDIG EL Jr. Congenital impatency of the nasolacrimal duct. Archives of ophthalmology (Chicago, Ill. : 1929). 1948 Feb:39(2):193-204 [PubMed PMID: 18868825]
Paul TO. Medical management of congenital nasolacrimal duct obstruction. Journal of pediatric ophthalmology and strabismus. 1985 Mar-Apr:22(2):68-70 [PubMed PMID: 3989643]
Sevel D, Development and congenital abnormalities of the nasolacrimal apparatus. Journal of pediatric ophthalmology and strabismus. 1981 Sep-Oct [PubMed PMID: 7299606]
Pediatric Eye Disease Investigator Group, Repka MX, Melia BM, Beck RW, Chandler DL, Fishman DR, Goldblum TA, Holmes JM, Perla BD, Quinn GE, Silbert DI, Wallace DK. Primary treatment of nasolacrimal duct obstruction with balloon catheter dilation in children younger than 4 years of age. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2008 Oct:12(5):451-5. doi: 10.1016/j.jaapos.2008.07.001. Epub [PubMed PMID: 18929305]
Harris GJ, DiClementi D. Congenital dacryocystocele. Archives of ophthalmology (Chicago, Ill. : 1960). 1982 Nov:100(11):1763-5 [PubMed PMID: 7138344]
Level 3 (low-level) evidenceSchnall BM, Christian CJ. Conservative treatment of congenital dacryocele. Journal of pediatric ophthalmology and strabismus. 1996 Sep-Oct:33(5):219-22 [PubMed PMID: 8880613]
Petersen RA, Robb RM. The natural course of congenital obstruction of the nasolacrimal duct. Journal of pediatric ophthalmology and strabismus. 1978 Jul-Aug:15(4):246-50 [PubMed PMID: 739359]
Level 3 (low-level) evidenceMiller AM, Chandler DL, Repka MX, Hoover DL, Lee KA, Melia M, Rychwalski PJ, Silbert DI, Pediatric Eye Disease Investigator Group, Beck RW, Crouch ER 3rd, Donahue S, Holmes JM, Quinn GE, Sala NA, Schloff S, Wallace DK, Foster NC, Frick KD, Golden RP, Lambert SR, Tien DR, Weakley DR Jr. Office probing for treatment of nasolacrimal duct obstruction in infants. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2014 Feb:18(1):26-30. doi: 10.1016/j.jaapos.2013.10.016. Epub [PubMed PMID: 24568978]
Level 1 (high-level) evidence