Introduction
The superficial peroneal nerve (superficial fibular nerve) is a mixed nerve that carries sensory information from the anterolateral aspect of the leg and the greater part of the dorsum of the foot (except for the first web space). Entrapment of the superficial peroneal nerve is not uncommon and can present with pain in the sensory distribution of the nerve with or without paresthesia. Block of the superficial peroneal nerve provides relief of symptoms of the entrapment and also provides anesthesia for surgical procedures involving the dorsum of the foot. It is better to perform the block under ultrasound guidance to avoid collateral damage of the neurovascular structures and get a more effective block.[1][2]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The superficial peroneal nerve arises as 1 of the 2 terminal branches of the common peroneal nerve at the level of the neck of the fibula in 81%. It originates between the fibular neck and the knee joint in about 9%. In the remaining 10%, it originates above the knee joint line.[3] The nerve runs over the upper part of fibula deep to the peroneus longus muscle; then it passes through peroneus longus to run between it and the peroneus brevis muscles. It descends between the peroneus brevis and the extensor digitorum longus muscles being more superficial. The nerve pierces the deep (crural) fascia becoming superficial through the peroneal tunnel at the junction of upper two-thirds and lower one-third (approximately 12 cm above the ankle). The nerve gives motor innervation to the peroneus longus and brevis muscles and sensory branches that carry sensory information from the anterolateral aspect of the leg and the greater part of the dorsum of the foot (except for the first web space).[4]
Indications
Superficial Peroneal Nerve Pain
Entrapment
- Running, football playing, and ballet dancing. They cause peroneal muscles hypertrophy that entraps the nerve while passing through the muscles[5]
- Tight boots and stocks
Trauma
- Accidental: Blunt trauma to the leg during playing, ankle sprains (stretch neuropathy, the trauma might pull on the nerve) and fibular fractures
- Surgical: Fasciotomy for compartment syndrome
Complex Regional Pain Syndrome of the Ankle and Foot[6]
Anesthesia for Surgical Procedures
Contraindications
- Patient refusal
- Allergy to the injectant
- Local infection
- Local Malignancies
- Coagulopathy
- Superficial peroneal neuropathy because of systemic illness as diabetes mellitus[9]
Equipment
- Povidone iodine solution or chlorhexidine.
- Sterile towels and gauze
- Sterile gloves
- A gown is required for catheter placement in cases of the continuous block
- In cases of an ultrasound-guided block, a high-frequency ultrasound probe with a sterile probe cover and gel are necessary
- Control syringe to aspirate before injection of local anesthetic in the land-mark based technique.
- Needles for drawing up the local anesthetic and for injection
- Local anesthetic with or without epinephrine and/or other additives, such as dexamethasone
Personnel
Well-trained physicians in landmark-based and ultrasound-guided nerve blocks can perform the procedure (including anesthesiologists and physiatrists).
Preparation
- Explain to the patient the need to receive a local injection, steps, injectants, adverse events, and prognosis.
- Get informed consent following the hospital protocol.
- Good illumination
- Good positioning for the patient; the patient usually lies supine. A lateral decubitus position allows better access in catheter block technique.
- Good positioning for the operator to avoid position related neck or back pain
- Good exposure of the leg
- Sterilization
- Preparation of the injectant: Local anesthetic alone or combined with epinephrine or steroids
- In cases of an ultrasound-guided block, adjustment of the machine settings is mandatory for getting a clear image of the nerve.
Technique or Treatment
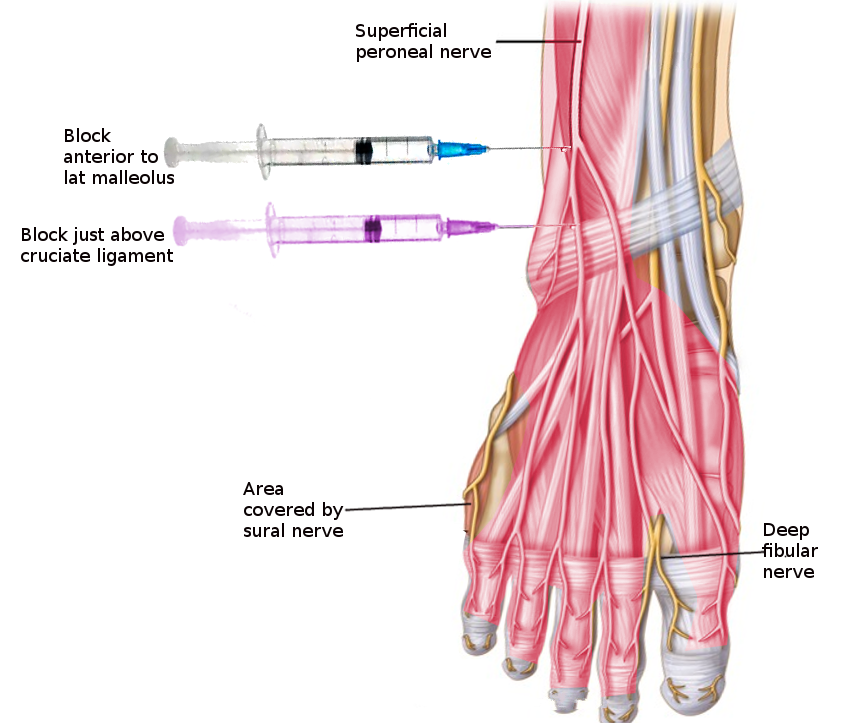
Landmark-Guided Technique
High-Level Block
Inject 6 to 10 ml of the injectant to ensure satisfactory block at the site of the maximal tenderness which is 10 to 15 cm proximal to the lateral malleolus at the anterolateral aspect of the leg.
Low-Level Block
Inject 6 ml of the injectant to ensure satisfactory block just anterior to the lateral malleolus.
In both techniques, operators introduce the needle from inferior to superior targeting the long axis of the nerve or from lateral to the medial targeting the short axis of the nerve.
Ultrasound-Guided Technique
- Place the probe transversely and scan the short axis of the nerve from its origin down to the lateral malleolus. The scanning will help recognition of the site of the entrapment, any anatomic variations and localize the accompanying small vein.
- Target the nerve at the site of the entrapment according to the ultrasound scanning or the desired level of the anesthesia:
- Between fibula and peroneus longus muscle
- Within the peroneus longus muscle
- Between peroneus brevis and extensor digitorum longus muscles
- At the peroneal tunnel
- Superficial to the lateral malleolus
The operator introduces the needle from the lateral to the medial using "in-plane approach" to inject 3 to 5 ml of the injectate targeting the short axis of the nerve.
Ultrasound-Guided Catheter Technique
The operator places the linear transducer posterolaterally about 12 cm distal to the knee to visualize the nerve. Low amplitude peripheral nerve stimulation (0.5 mA [0.1 ms] stimulus) applied to reproduce the patient’s pain and insert the catheter under the ultrasound guidance through the "in-plane approach" to target the short axis of the nerve. The operator injects a bolus of 15 mL of the injectate (containing 0.25% bupivacaine with epinephrine 1:200,000 and clonidine 25 mcg) via the catheter.
Benefits of Ultrasound Guidance
- Ultrasound guidance avoids collateral damage of the nearby vessels and extremely lowers the risk of procedure-related nerve injury.
- It helps the accurate placement of the injectate around the target nerve leading to better pain control.
- Ultrasound guidance needs smaller amounts of local anesthetics to achieve the target pain control.
Complications
- Allergy to the injectate
- Infection
- Bleeding
- Injury of the accompanying vein
- Injury of the superficial peroneal nerve
- Systemic toxicity of the local anesthetics:
- Neurological: Metallic taste, auditory changes, circumoral numbness, blurred vision, agitation, and seizures.
- Cardiovascular: hypotension, abnormal cardiac contractility, dysrhythmias, complete heart block, and cardiovascular collapse.
Clinical Significance
Superficial peroneal nerve carries sensations from the anterolateral aspect of the leg and the greater part of the dorsum of the foot (except for the first web space). Entrapment of the superficial peroneal nerve is not uncommon. Because of its long course, the entrapment can occur between the fibula and peroneus longus, within peroneus longus, between peroneus brevis and extensor digitorum longus muscles, at the fascial tunnel where it emerges through the deep fascia to become superficial, the lower third of the fibula and in front of the lateral malleolus. Patients having entrapment of the nerve suffer from pain, tingling, and paresthesia along anterolateral aspect of the leg and most of the dorsum of the foot. The differential diagnosis includes L5 radiculopathy, lumbosacral plexopathy, Sciatic mononeuropathy, common peroneal neuropathy, arterial insufficiency, and anterior compartment syndrome. Blocking of the nerve eases the symptoms of the entrapment and allows for painless surgical procedures for pathologies over the dorsum of the foot in the area supplied by the superficial peroneal nerve. The ultrasound-guided block provides better results and lower complications than the landmark-guided block.[10][11][12]
Enhancing Healthcare Team Outcomes
Physicians performing superficial peroneal nerve block should master the ultrasound scanning of the superficial peroneal nerve in people with a classic origin and anatomic course and those with anatomic variations of the origin and the course. Also, They should master excellent clear needle tip visualization under ultrasound guidance to avoid nerve injury or intra-neural injection. Assisting staff as nurses should be ready to deal with complications and use medications to manage systemic complications of the used local anesthetics. (Level V)
Media
References
Ribak S, Fonseca JR, Tietzmann A, Gama SA, Hirata HH. The Anatomy and Morphology of the Superficial Peroneal Nerve. Journal of reconstructive microsurgery. 2016 May:32(4):271-5. doi: 10.1055/s-0035-1568881. Epub 2015 Dec 16 [PubMed PMID: 26676677]
Allam AE, Khalil AAF, Eltawab BA, Wu WT, Chang KV. Ultrasound-Guided Intervention for Treatment of Trigeminal Neuralgia: An Updated Review of Anatomy and Techniques. Pain research & management. 2018:2018():5480728. doi: 10.1155/2018/5480728. Epub 2018 Apr 2 [PubMed PMID: 29808105]
Van den Bergh FR, Vanhoenacker FM, De Smet E, Huysse W, Verstraete KL. Peroneal nerve: Normal anatomy and pathologic findings on routine MRI of the knee. Insights into imaging. 2013 Jun:4(3):287-99. doi: 10.1007/s13244-013-0255-7. Epub 2013 May 25 [PubMed PMID: 23709403]
Agthong S, Huanmanop T, Sasivongsbhakdi T, Ruenkhwan K, Piyawacharapun A, Chentanez V. Anatomy of the superficial peroneal nerve related to the harvesting for nerve graft. Surgical and radiologic anatomy : SRA. 2008 Mar:30(2):145-8. doi: 10.1007/s00276-007-0296-z. Epub 2008 Jan 9 [PubMed PMID: 18183347]
Schon LC, Baxter DE. Neuropathies of the foot and ankle in athletes. Clinics in sports medicine. 1990 Apr:9(2):489-509 [PubMed PMID: 2183956]
Level 3 (low-level) evidenceJaffe JD, Henshaw DS, Nagle PC. Ultrasound-guided continuous superficial peroneal nerve block below the knee for the treatment of nerve injury. Pain practice : the official journal of World Institute of Pain. 2013 Sep:13(7):572-5. doi: 10.1111/papr.12021. Epub 2012 Dec 13 [PubMed PMID: 23241230]
Level 3 (low-level) evidenceWiederhold BD, Garmon EH, Peterson E, Stevens JB, O'Rourke MC. Nerve Block Anesthesia. StatPearls. 2023 Jan:(): [PubMed PMID: 28613761]
Snaith R, Dolan J. Ultrasound-guided superficial peroneal nerve block for foot surgery. AJR. American journal of roentgenology. 2010 Jun:194(6):W538; author reply W542. doi: 10.2214/AJR.09.3975. Epub [PubMed PMID: 20489075]
Level 3 (low-level) evidenceRodziewicz TL, Patel S, Garmon EH. Lower Extremity Blocks. StatPearls. 2023 Jan:(): [PubMed PMID: 29261945]
Canella C, Demondion X, Guillin R, Boutry N, Peltier J, Cotten A. Anatomic study of the superficial peroneal nerve using sonography. AJR. American journal of roentgenology. 2009 Jul:193(1):174-9. doi: 10.2214/AJR.08.1898. Epub [PubMed PMID: 19542411]
Beltran LS, Bencardino J, Ghazikhanian V, Beltran J. Entrapment neuropathies III: lower limb. Seminars in musculoskeletal radiology. 2010 Nov:14(5):501-11. doi: 10.1055/s-0030-1268070. Epub 2010 Nov 11 [PubMed PMID: 21072728]
Allam AE, Al-Ashkar DS, Negm AA, Eltawab BA, Wu WT, Chang KV. Ultrasound-guided methotrexate injection for De Quervain disease of the wrist: what lies beyond the horizon? Journal of pain research. 2017:10():2299-2302. doi: 10.2147/JPR.S143256. Epub 2017 Sep 26 [PubMed PMID: 29026332]