Introduction
The genus Nocardia is an aerobic actinomycete, catalase-positive, gram-positive bacillus, with a branching filamentous form first described in 1888 by Edmond Nocard.[1][2] Nocardia sp. is found worldwide in a myriad of environments.[3] Disease resulting from Nocardia infection results in a variety of symptoms based upon the location of the infection. The classic sites of infection include pulmonary infection (most common) and primary cutaneous infection; however, dissemination to other sites and CNS involvement often occurs.[2][4] Typically, Nocardia is an opportunistic pathogen that primarily affects immunosuppressed patients.[2][3] However, Nocardia can also infect immunocompetent individuals, especially the cutaneous form of the disease.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Nocardia has been reported to be found ubiquitously in the environment and has been cultured from both fresh and saltwater, dust, soil, decaying vegetation, and decaying organic matter.[2][5][6] The majority of Nocardia infections are thought to be due to inhalation of bacteria via environmental sources (i.e., dust), leading to the most common form of the infection, pulmonary nocardiosis.[5]
Contrastingly, cutaneous nocardiosis arises via the inoculation of traumatic skin lesions. Other methods of infection that have been implicated include hospitalized acquired infections where clusters of nocardiosis have been described, and infection is transmitted from central venous catheters.[7][8] Once a patient has a Nocardia infection, whether symptomatic or asymptomatic, it can spread hematogenously or by local extensions. Overall, immunocompromised individuals are more susceptible to nocardiosis and disseminated spread.
Epidemiology
The CDC reports the incidence of nocardiosis in the US as 500-1000 cases per year. Globally, the incidence of Nocardia infection is not well known. The incidence of nocardiosis is thought to be increasing due to an increasing population and an increased number of immunocompromised individuals worldwide.[1][9][10] Nocardiosis affects all ages and races but is more common in males than females in a 3 to 1 ratio. Nocardia typically manifests as an opportunistic infection in immunocompromised patients, with 60% of patients with nocardiosis having immunosuppressive conditions.[2][6][11] However, up to 33% of patients are immunocompetent; this is especially true of cutaneous infections where immunocompetent individuals are the majority of cases.[3][5][12] Dissemination of both cutaneous and pulmonary nocardiosis is more likely in immunocompromised hosts.
Immunocompromised conditions associated with Nocardia infections include:
- HIV (most common underlying condition)[13][14]
- Cancer
- Chemotherapy treatment
- Corticosteroid treatment (present in more than half of patients with Nocardia infection according to one report)[13][14]
- Solid organ transplant recipients (especially lung transplant)[15]
- Allogenic hematopoietic stem cell transplant recipients[16]
- Diabetes
- Autoimmune diseases
- Chronic lung diseases such as COPD (many patients on corticosteroid therapy)[17]
- Any condition that results in deficient cell-mediated immunity
Pathophysiology
Found commonly in soil, presentations of Nocardia are:
- Primary cutaneous nocardiosis
- Cellulitic and sporotrichoid forms
- Actinomycetoma
- Disseminated disease (most common secondary to pulmonary involvement)
The most common form of Nocardia infection is pulmonary, and most common causing human infection are:
- N. asteroides
- N. brasiliensis
- N. caviae
Nocardia sp. is a member of the family Nocardiaceae (along with the genus Rhodococcus), belonging to the “aerobic actinomycetes” suborder. Currently, the genus Nocardia contains 80-100 species, of these, more than fifty have been implicated as human or animal pathogens.[3][18] Historically, Nocardia asteroides was implicated as the most common cause of numerous Nocardial human infections. However, it was later found to be a group of bacteria that have been further classified into separate species.[3][5] Various Nocardia species have been shown to be more prevalent in specific geographic locations. For example, Nocardia brasiliensis, a species associated with cutaneous infections (80% of all cutaneous Nocardia infection), is found more frequently in tropical and sub-tropical climates.[2] Nocardia infections vary significantly in symptomatology based on the site of infection. However, Nocardia typically produces suppurative necrosis with frequent abscess formation at most sites of infection, including pulmonary, cutaneous, and CNS. That being said, Nocardia also can form cavitary lesions, skin nodules, and cellulitis making diagnosis difficult as it is similar to many other bacterial and fungal infections.
Primary cutaneous nocardiosis is most commonly caused by N. brasiliensis. Cutaneous nocardiosis from N. asteroides is usually secondary to hematogenous dissemination. Primary cutaneous nocardiosis is divided into three entities:
- Lymphocutaneous infection (often misdiagnosed for sporotrichosis)
- Mycetoma
- Superficial skin infection (ulceration, abscess, cellulitis)
Histopathology
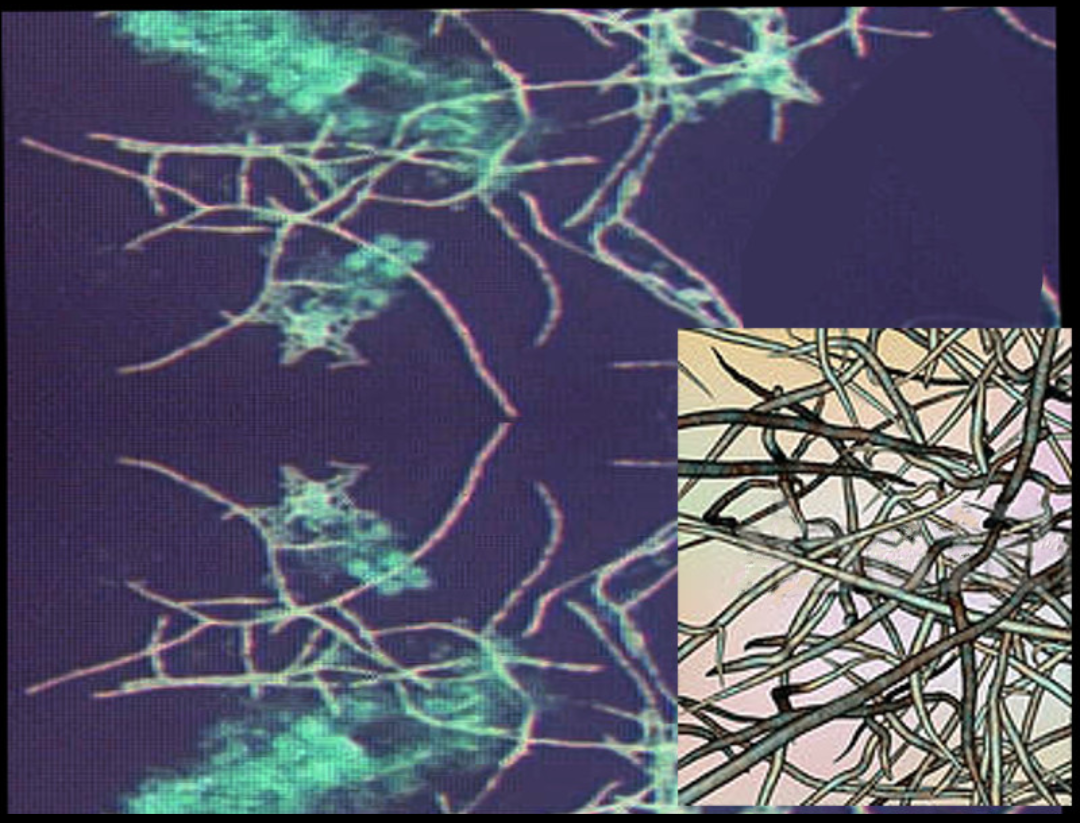
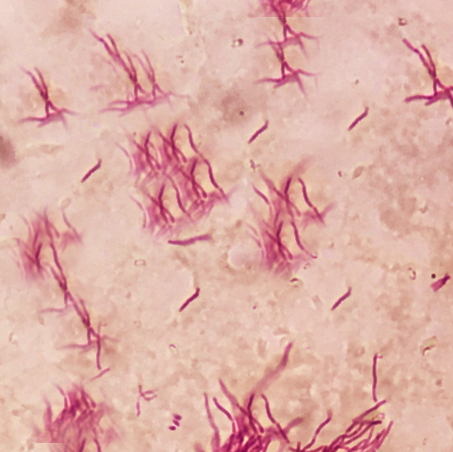
The characteristic morphology of Nocardia is a branching, filamentous, gram-positive rod when observed under the microscope. Nocardia can resemble Actinomyces species on gram stain. However, Nocardia is an obligate aerobe that stains weakly positive on acid-fast staining.[1]
Nocardia is typically weakly acid-fast after traditional carbol-fuchsin staining and positive on modified acid-fast staining due to the presence of mycolic acid in the cell wall. Unlike mycobacteria (also acid-fast positive), Nocardia has a “beaded” appearance on acid-fast staining.[3] Nocardia is catalase-positive and urease positive.
Toxicokinetics
Nocardia has low virulence, and so clinically significant disease occurs in patients with immunosuppression or weak immune systems. The virulence factors of Nocardia are the enzymes catalase and superoxide dismutase, which inactivates reactive oxygen species toxic to the bacteria produced by neutrophils.[2] Thus, patients with chronic granulomatous disease are susceptible to Nocardia infections. Nocardia also has “cord factor” similar to Mycobacterium tuberculosis preventing the fusion of phagosomes with lysosomes.[19][20]
History and Physical
The symptoms of nocardiosis vary depending on where the site of infection is. Patients with pulmonary nocardiosis can present with fever, weight loss, night sweats, cough, and chest pain. If the infection spreads to the CNS, symptoms can include headache, weakness, confusion, and seizures. Cutaneous nocardiosis can present with skin ulcers, nodules that are sometimes draining, and the infection can spread to the lymph nodes.
Delay in the diagnosis of an immunosuppressed patient with nocardiosis has been implicated in treatment failure and poor prognosis. Therefore, if there is suspicion for infection with Nocardia, it is imperative to notify the laboratory of this suspicion so that steps can be taken by the laboratory to identify the species and antibiotic sensitivity pattern.
Evaluation
Nocardiosis is a challenge to diagnose due to its non-specific findings and imaging that can suggest many different diagnoses (see DDX section). The diagnosis of nocardiosis is established with a culture of the causative organism from the infection site. Common culture samples include sputum, skin biopsy, abscess aspirates, or a sample from bronchoalveolar lavage. It can take several days (3-5 days) to isolate Nocardia in culture. Blood cultures for Nocardemia should be drawn in instances of pulmonary or disseminated disease, although Nocardia bacteremia is very rare.[21]
Imaging via computed tomography (CT) or chest radiograph is a valuable diagnostic tool, especially in evaluating pulmonary nocardiosis. However, findings vary significantly and can include irregular nodules (can be cavitary), diffuse pulmonary infiltrates, lung abscesses, or pleural effusion. Imaging findings help support a history and physical exam that may be concerning for nocardiosis.
All patients with nocardiosis (except those with mycetoma) should undergo brain CT or magnetic resonance imaging (MRI). If the primary infection spreads, the CNS is the most common location (44% of the time).[6] An intracranial abscess is the most common abnormality found on imaging. If concerned for nocardial meningitis, a lumbar puncture should be performed, and CNS analysis conducted. Nocardial meningitis is rare but presents similar to other bacterial meningitis.[22][23]
It is important to notify the laboratory when suspecting Nocardia as a possible infection. This will allow for gram staining and modified acid-fast staining helping to confirm diagnosis as soon as possible. This is especially important as it can take several days to culture Nocardia species. Similarly, this will help aid in initial treatment prior to obtaining antibiotic susceptibility patterns. The recent development of more rapid and precise PCR and 16S rDNA sequencing to identify Nocardia species may allow for faster diagnosis and treatment of nocardiosis.[24]
Treatment / Management
Since the 1940s, the mainstay treatment for Nocardia infections has been sulfonamides, the most common of which in the U.S. is trimethoprim-sulfamethoxazole (TMP-SMX).[2][5][25][26] Resistance to TMP-SMX as a single agent has been shown to be species-dependent with N. farcinica, N. nova, and N. otitidiscaviarum showing increased multi-drug resistance.[3][26] Due to this resistance, most clinicians now administer combination drug therapy, especially for patients with a serious infection, disseminated disease, or CNS involvement. The most common regiment includes TMP-SMX, amikacin, and imipenem. However, if the patient has CNS involvement, it is important to pick agents with good CNS penetration, such as TMP-SMX and ceftriaxone.[3][27] More recently, the oxazolidinone, linezolid, has been shown to have excellent coverage against all known pathogenic Nocardia species.[3][5](B3)
Other agents to consider include:
- Carbapenems: imipenem, meropenem, or ertapenem, with imipenem having the best efficacy
- Quinolones: especially moxifloxacin
- Tetracyclines: minocycline
The duration of treatment is dependent on the location of infection and the immune status of the affected individual. For patients with pulmonary or multifocal disease that does not involve the CNS, a treatment regimen for 6-12 months is indicated. If the patient is immunosuppressed or has CNS involvement, they should be treated for a minimum of 12 months.[3](B3)
Prophylaxis: Patients shown to be at greatest risk for Nocardia infection have been documented to be patients that are HIV positive.[13][14] Commonly, TMP-SMX is used as prophylaxis in HIV patients for coverage against Pneumocystis jiroveci pneumonia (PJP) or Toxoplasma gondii. Fortunately, this prophylaxis also has been shown to help reduce Nocardia infections.(B2)
Differential Diagnosis
Nocardia is extremely difficult to differentiate from other infectious etiologies. The differential diagnosis for primary sites of infection are outlined below:[3][10]
Pulmonary disease
- Fungal infections – aspergillosis, mucormycosis, histoplasmosis, blastomycosis, and cryptococcosis
- Actinomyces infection
- Mycobacterial infections – including Mycobacterium tuberculosis
- Lung malignancy
Cutaneous disease
- Superficial cellulitis – group A strep (GAS), staph aureus
- Lymphocutaneous – sporotrichosis, Mycobacterium marinum
- Mycetoma (late-stage) – actinomycosis, fungal infections
- Other: cutaneous leishmaniasis, Cryptococcus
CNS disease
- Malignancy
- Bacterial abscess
- Vascular infarction
- Other: toxoplasmosis, mycobacterial tuberculosis, fungal infection, cysticercosis
Prognosis
The morbidity and mortality of Nocardia depend on the site and extent of infection as well as underlying host factors. Prognosis varies based on the site of infection.[28]
- Skin and soft tissue infections: approximately 100% cured
- Pleuropulmonary infections: approximately 80% cured
- Disseminated nocardiosis: 3% cured
- CNS involvement: 50% to 85% cure rate[29]
Complications
Complications can arise due to the spread from the primary site of infection. This is especially true of pulmonary nocardiosis that has spread locally. This can result in pericarditis and superior vena cava (SVC) syndrome depending upon the location and extent of spread. Additionally, the risk of spread to the CNS results in a multitude of possible complications, including focal neurologic deficits and meningitis. Delay in the diagnosis of an immunosuppressed patient with nocardiosis has been implicated in treatment failure and poor prognosis.[30] Therefore, if there is suspicion for infection with Nocardia, it is imperative to notify the laboratory so that steps can be taken by the laboratory to identify the species and antibiotic sensitivity pattern as quickly as possible. Additionally, the advent of PCR and 16S rDNA sequencing to identify Nocardia species may allow for faster identification and sequencing.[24]
Deterrence and Patient Education
Overall, Nocardia is a ubiquitous bacteria that can result in many forms of infection. Infection is more likely in immunocompromised individuals, especially the pulmonary and CNS forms of nocardiosis. Patient's diagnosed with HIV should be aware of the various presentations of Nocardia. TMP-SMX prophylaxis can be given for individuals that are at increased risk for nocardial infection, although there are many strains that are resistant to TMP-SMX as a single agent.
While immunocompromised individuals are at greatest risk, immunocompetent individuals are also at risk for infection, particularly the cutaneous form of the infection. The main etiology of infection in these patients is due to a skin lesion that was contaminated with organic matter or soil. Therefore, a key way to lower the risk of cutaneous nocardiosis is to wear closed shoes and gloves when working in hazardous areas (construction sites, gardens, etc.). If a skin lesion is sustained, it is important to clean the wound thoroughly. If the area becomes red, swollen, and warm or if there is purulent drainage, a primary care clinician should be consulted.
In general, Nocardia infections are very rare but should be considered if the workup is negative for other common causes of the presenting symptoms.
Enhancing Healthcare Team Outcomes
Nocardial infection often poses a diagnostic dilemma. Nocardiosis exhibits signs and symptoms that vary greatly based upon the location of the infection (cutaneous, pulmonary, CNS, disseminated). Additionally, there is a myriad of differential diagnoses that present similarly to nocardial infection and are often more commonly occurring, including fungal and other bacterial etiologies. The history and physical exam are important in assessing a patient's risk for nocardiosis. Imaging may allow the clinician to rule down their differential diagnosis honing in on Nocardia as a potential source of the infection. The most important diagnostic step is obtaining a sample of the infection (skin biopsy, sputum sample, abscess aspirate) in order to run a gram-stain, acid-fast stain, and culture of the organism. Finally, newer PCR and DNA sequencing methods may allow for a faster species-specific diagnosis.[24]
If the diagnosis of nocardiosis is confirmed, it is important to look for dissemination from the primary source of infection. Patients with Nocardia infections are best managed by an interprofessional team. Radiology should be consulted for further workup, which includes brain imaging. Radiologists play an important role as 44% of the time disseminated pulmonary infections are found to have CNS involvement. Brain imaging may reveal one or more cerebral abscesses consistent with CNS nocardiosis.[6] Finally, infectious disease should be consulted. Due to the increasing resistance of Nocardia to TMP-SMX and other sulfonamides, it is important to consult infectious disease specialists for the best combination of antibiotics for the patient.
Since Nocardia infections are very rare, there is limited knowledge regarding the outcomes of Nocardia treatment. The outcomes of nocardial infections depend on the site of infection and the immune status of the host. However, to improve outcomes, prompt consultation with an interprofessional group of specialists is recommended so that appropriate treatment can be started.
Media
(Click Image to Enlarge)

This image depicts the feet, ankles, and lower legs of a patient, who had presented with an infection known as nocardiosis, a form of actinomycosis, due to the bacterium, Nocardia somaliensis, which had affected the left foot and ankle, causing severe swelling and deformation of the normal structural contours. Contributed by the CDC/ Dr. Hardin
References
Fatahi-Bafghi M. Nocardiosis from 1888 to 2017. Microbial pathogenesis. 2018 Jan:114():369-384. doi: 10.1016/j.micpath.2017.11.012. Epub 2017 Nov 13 [PubMed PMID: 29146497]
Lerner PI. Nocardiosis. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1996 Jun:22(6):891-903; quiz 904-5 [PubMed PMID: 8783685]
Level 3 (low-level) evidenceWilson JW. Nocardiosis: updates and clinical overview. Mayo Clinic proceedings. 2012 Apr:87(4):403-7. doi: 10.1016/j.mayocp.2011.11.016. Epub [PubMed PMID: 22469352]
Level 3 (low-level) evidenceCastro JG, Espinoza L. Nocardia species infections in a large county hospital in Miami: 6 years experience. The Journal of infection. 2007 Apr:54(4):358-61 [PubMed PMID: 16979760]
Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clinical microbiology reviews. 2006 Apr:19(2):259-82 [PubMed PMID: 16614249]
Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clinical microbiology reviews. 1994 Apr:7(2):213-64 [PubMed PMID: 8055469]
Level 3 (low-level) evidenceSahathevan M, Harvey FA, Forbes G, O'Grady J, Gimson A, Bragman S, Jensen R, Philpott-Howard J, Williams R, Casewell MW. Epidemiology, bacteriology and control of an outbreak of Nocardia asteroides infection on a liver unit. The Journal of hospital infection. 1991 Jun:18 Suppl A():473-80 [PubMed PMID: 1679818]
Level 3 (low-level) evidenceAl Akhrass F, Hachem R, Mohamed JA, Tarrand J, Kontoyiannis DP, Chandra J, Ghannoum M, Haydoura S, Chaftari AM, Raad I. Central venous catheter-associated Nocardia bacteremia in cancer patients. Emerging infectious diseases. 2011 Sep:17(9):1651-8. doi: 10.3201/eid1709.101810. Epub [PubMed PMID: 21888790]
Ambrosioni J, Lew D, Garbino J. Nocardiosis: updated clinical review and experience at a tertiary center. Infection. 2010 Apr:38(2):89-97. doi: 10.1007/s15010-009-9193-9. Epub 2010 Mar 20 [PubMed PMID: 20306281]
Gomes F, La Feria P, Costa C, Texeira H. Nocardia cyriacigeorgica and Aspergillus Co-infection in a Patient with Giant-cell Arteritis. European journal of case reports in internal medicine. 2019:6(1):000997. doi: 10.12890/2019_000997. Epub 2019 Jan 3 [PubMed PMID: 30756072]
Level 3 (low-level) evidenceSaubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. Journal of clinical microbiology. 2003 Oct:41(10):4497-501 [PubMed PMID: 14532173]
Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the United States, 1972-1974. The Journal of infectious diseases. 1976 Sep:134(3):286-9 [PubMed PMID: 789786]
Minero MV, Marín M, Cercenado E, Rabadán PM, Bouza E, Muñoz P. Nocardiosis at the turn of the century. Medicine. 2009 Jul:88(4):250-261. doi: 10.1097/MD.0b013e3181afa1c8. Epub [PubMed PMID: 19593231]
Level 2 (mid-level) evidenceLong PF. A retrospective study of Nocardia infections associated with the acquired immune deficiency syndrome (AIDS). Infection. 1994 Sep-Oct:22(5):362-4 [PubMed PMID: 7843819]
Level 3 (low-level) evidencePeleg AY, Husain S, Qureshi ZA, Silveira FP, Sarumi M, Shutt KA, Kwak EJ, Paterson DL. Risk factors, clinical characteristics, and outcome of Nocardia infection in organ transplant recipients: a matched case-control study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2007 May 15:44(10):1307-14 [PubMed PMID: 17443467]
Level 2 (mid-level) evidenceChouciño C,Goodman SA,Greer JP,Stein RS,Wolff SN,Dummer JS, Nocardial infections in bone marrow transplant recipients. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1996 Nov; [PubMed PMID: 8922795]
Level 3 (low-level) evidenceMartínez Tomás R, Menéndez Villanueva R, Reyes Calzada S, Santos Durantez M, Vallés Tarazona JM, Modesto Alapont M, Gobernado Serrano M. Pulmonary nocardiosis: risk factors and outcomes. Respirology (Carlton, Vic.). 2007 May:12(3):394-400 [PubMed PMID: 17539844]
Level 2 (mid-level) evidenceConville PS, Brown-Elliott BA, Smith T, Zelazny AM. The Complexities of Nocardia Taxonomy and Identification. Journal of clinical microbiology. 2018 Jan:56(1):. doi: 10.1128/JCM.01419-17. Epub 2017 Dec 26 [PubMed PMID: 29118169]
Bafghi MF, Eshraghi SS, Heidarieh P, Habibnia S, Nasab MR. Nocardiosis in immune disorder disease. The Malaysian journal of medical sciences : MJMS. 2014 Jan:21(1):75-6 [PubMed PMID: 24639618]
Singh S, Samant R, Rodrigues C. Nocardiosis in a patient with common variable immunodeficiency. The Journal of the Association of Physicians of India. 2006 Jun:54():495-6 [PubMed PMID: 16909702]
Level 3 (low-level) evidenceBoell K, Gotoff R, Foltzer M, Storm R, Bourbeau PP. Implantable defibrillator pocket infection and bacteremia caused by Nocardia nova complex isolate. Journal of clinical microbiology. 2003 Nov:41(11):5325-6 [PubMed PMID: 14605196]
Level 3 (low-level) evidenceChow E, Moore T, Deville J, Nielsen K. Nocardia asteroides brain abscesses and meningitis in an immunocompromized 10-year-old child. Scandinavian journal of infectious diseases. 2005:37(6-7):511-3 [PubMed PMID: 16012015]
Davis J, Kreppel AJ, Brady RC, Jones B, Stevenson CB, Fouladi M, Hummel TR. Nocardia farcinica Meningitis Masquerading as Central Nervous System Metastasis in a Child With Cerebellar Pilocytic Astrocytoma. Journal of pediatric hematology/oncology. 2015 Aug:37(6):482-5. doi: 10.1097/MPH.0000000000000360. Epub [PubMed PMID: 26181420]
Sonesson A, Oqvist B, Hagstam P, Björkman-Burtscher IM, Miörner H, Petersson AC. An immunosuppressed patient with systemic vasculitis suffering from cerebral abscesses due to Nocardia farcinica identified by 16S rRNA gene universal PCR. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2004 Nov:19(11):2896-900 [PubMed PMID: 15496565]
Level 3 (low-level) evidenceWallace RJ Jr, Septimus EJ, Musher DM, Berger MB, Martin RR. Treatment of experimental nocardiosis in mice: comparison of amikacin and sulfonamide. The Journal of infectious diseases. 1979 Aug:140(2):244-8 [PubMed PMID: 383855]
Level 3 (low-level) evidenceLerner PI, Baum GL. Antimicrobial susceptibility of Nocardia species. Antimicrobial agents and chemotherapy. 1973 Aug:4(2):85-93 [PubMed PMID: 4790942]
Gombert ME, Aulicino TM, duBouchet L, Silverman GE, Sheinbaum WM. Therapy of experimental cerebral nocardiosis with imipenem, amikacin, trimethoprim-sulfamethoxazole, and minocycline. Antimicrobial agents and chemotherapy. 1986 Aug:30(2):270-3 [PubMed PMID: 3532945]
Level 3 (low-level) evidenceSmego RA Jr, Moeller MB, Gallis HA. Trimethoprim-sulfamethoxazole therapy for Nocardia infections. Archives of internal medicine. 1983 Apr:143(4):711-8 [PubMed PMID: 6340623]
Level 2 (mid-level) evidenceLavalard E, Guillard T, Baumard S, Grillon A, Brasme L, Rodríguez-Nava V, Litré F, Delmer A, Boiron P, de Champs C. [Brain abscess due to Nocardia cyriacigeorgica simulating an ischemic stroke]. Annales de biologie clinique. 2013 May-Jun:71(3):345-8. doi: 10.1684/abc.2013.0816. Epub [PubMed PMID: 23747674]
Level 3 (low-level) evidenceOzgenç O, Avcı M, Arı A, Celebi IY, Coşkuner SA. Long-term treatment of persistent disseminated Nocardia cyriacigeorgica infection. The Brazilian journal of infectious diseases : an official publication of the Brazilian Society of Infectious Diseases. 2014 Sep-Oct:18(5):556-60. doi: 10.1016/j.bjid.2014.03.007. Epub 2014 May 13 [PubMed PMID: 24833199]
Level 3 (low-level) evidence