Introduction
Noroviruses are nonenveloped, positive-sense, single-stranded RNA viruses belonging to the Caliciviridae viral family. The virus was first identified and named “Norwalk virus” when it was discovered as the cause of a 1968 outbreak of gastroenteritis in Norwalk, Ohio. Norovirus is a common cause of acute gastrointestinal illness worldwide. In developed countries with rotavirus vaccine programs, norovirus surpasses rotavirus as the most common cause of gastroenteritis in children. Common symptoms of norovirus infection include nausea, vomiting, and diarrhea. These could lead to clinically significant dehydration, requiring hospitalizations. In addition to clinical effects, norovirus also has a major financial impact in developed nations.[1][2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
There are seven known genogroups of norovirus, but only genogroups I and II are responsible for the vast majority of human cases. An extremely small number of cases are attributed to norovirus GIV. While both genogroups I and II are both clinically relevant, a specific strain from genogroup II, norovirus GII.4, is responsible for the majority of human outbreaks. Additionally, illness produced by GII.4 strains tends to be more severe and is associated with higher mortality than illness from other strains. Studies have shown that waterborne outbreaks tend to be associated with genogroup I strains, while healthcare-related and winter outbreaks are more likely to have genogroup II strains as a causative agent. Noroviruses are classified into genogroups and genotypes based on amino acid diversity in VP1 and ORF1 proteins. The primary mode of transmission is fecal-oral. Sources include ingestion of contaminated water or food or direct transmission from a contaminated surface or infected person. The virus is resistant and can stay on surfaces even after disinfecting. The virus also has a low viral inoculum to cause infection. As few as ten viral particles are needed to cause infection.[3]
Epidemiology
Norovirus is responsible for an estimated 21 million cases of gastrointestinal illness in the United States each year. Because patients with mild disease may not seek medical treatment, the number of cases may exceed the estimate. Norovirus is believed to cause approximately 60% of cases of acute gastroenteritis in the United States, and the CDC attributes 400,000 emergency department visits and 71,000 hospitalizations each year to norovirus infection. In a review of reported norovirus outbreaks, a food-related transmission was the most common source of widespread disease. Food-related transmission may be due to the ingestion of food that is contaminated during production or the ingestion of food that was contaminated by food service workers during preparation. High-risk food for norovirus contamination include foods that are served raw, like fruits and vegetables, as well as oysters and fish.
Outbreaks are common in a number of different settings. Norovirus is known to cause outbreaks of gastroenteritis in hospitals and other healthcare facilities. In addition to healthcare settings, outbreaks may occur in schools, military barracks, cruise ships, and resorts. Person-to-person transmission is the most common form of transmission, but contaminated surfaces also contribute to disease propagation. Surfaces may be contaminated with viral particles by splashing of emesis or stool or by aerosolized viral particles. The importance of good hand hygiene and effective surface cleaning should be stressed during norovirus outbreaks. Studies suggest that washing hands with soap and running water for at least 20 seconds is the most effective form of hand hygiene for eliminating norovirus. Studies on the effectiveness of alcohol-based hand rubs are inconclusive. Some studies suggest that high-concentration ethanol-based hand sanitizers decrease viral concentration on the hands, but these types of cleaners should be used as a supplement to hand-washing with soap and water. Surfaces such as sinks, toilets, tables, chairs, and beds should be cleaned with a hypochlorite (bleach) solution, and adequate contact time should be ensured. Furthermore, items that have been contaminated with infected emesis or stool that cannot be properly disinfected should be discarded.
Although people of all age groups are at risk of contracting norovirus, those at the extremes of age and the immunocompromised are at highest risk of poor outcomes. Elderly patients are at increased risk of fatal outcomes, with some studies showing a 30-day mortality rate of 7% for patients with community-acquired norovirus infection. Similarly, neonates have an increased rate of serious complications, such as necrotizing enterocolitis. Of all age groups, young children have the highest incidence of norovirus. Estimates suggest an annual incidence of norovirus to be 21,400 per 100,000 for children under 5 years of age. Norovirus infections are also more prevalent in developing nations. Nguyen et al. estimated that 17% of reported gastroenteritis cases in developing countries are due to norovirus. Also notable is norovirus’s effects on immunocompromised patients. Patients with compromised immune systems have a higher risk of infection of norovirus, higher rates of complications, and increased potential for prolonged asymptomatic viral shedding.[4][5]
Pathophysiology
Noroviruses are difficult to culture in a lab setting. Because of this, it has been difficult to predict exactly how norovirus infects and replicates in humans. Studies suggest that norovirus infection is multi-faceted, with the involvement of multiple cell types in the human gut. The predominant cell type lining the human gut is a single layer of intestinal epithelial cells called enterocytes. Lying deep to the enterocytes are numerous immune cells. Several studies have confirmed that norovirus infects and replicates in immune cells including macrophages, dendritic cells, and B cells. It is postulated that noroviruses have a way of bypassing enterocytes to enter the human hosts. Proposed mechanisms include entering through M cells, a specialized type of cell in the gut that overlies the Peyer patches and lymphoid follicles in the gut. M cells lack microvilli and do not secrete mucus, making it easier for the norovirus to enter the host and invade immune cells. However, although definitive data are lacking, other studies suggest norovirus may directly invade enterocytes lining the gut lumen. Furthermore, the role of the host’s pre-existing gut microflora in norovirus infection is being investigated. It has been proposed that norovirus interacts with bacteria in the gut to enhance infection and replication. The average time period from inoculation with the virus until clinical symptoms develop is 1.2 days, and symptoms of norovirus usually resolve within 1 to 3 days. Although symptoms may resolve, humans can continue to shed the virus in their stool for extended periods of time, up to 60 days in some cases. Immunocompromised patients can continue to shed the virus for months or years.[6]
History and Physical
The history and physical exam are important in the evaluation of all patients with abdominal pain and gastrointestinal symptoms. Patients infected with norovirus typically have symptoms consistent with gastroenteritis. Common symptoms include nausea, vomiting, abdominal pain and cramping, diarrhea, myalgias, headache, and chills. Some patients report a predominance of diarrhea while others report nausea and vomiting as primary symptoms. Symptoms may develop with or without prodrome and typically persist for 1 to 3 days. Physical exam findings are usually consistent with gastroenteritis. The abdominal exam may reveal nonspecific, non-focal tenderness, but significant tenderness or peritoneal signs on the abdominal exam should prompt further investigation for other pathology. Likewise, the grossly bloody stool is not consistent with norovirus infection and warrants further investigation. Depending on their hydration status, patients may show signs of dehydration such as tachycardia, orthostatic hypotension, decreased skin turgor, and dry mucous membranes. Rarely, patients may present with significant neurologic symptoms such as a seizure or encephalopathy.
Important historical elements to elicit include the patient’s living quarters (e.g., nursing home, military barracks), the source of water (e.g., river, city, well), recent travel, recent antibiotic use, ingestions of undercooked or raw food, or recent sick contacts (e.g., school). It is also important to screen for immunocompromised states which could predict a longer course of symptoms and greater risk for morbidity and mortality.
Evaluation
Many cases of norovirus go undiagnosed, as many patients do not seek medical attention for treatment. For patients seeking evaluation by a healthcare provider, the diagnostic evaluation will be similar to most patients with gastroenteritis. Usually, diagnostic testing is not indicated. For certain patients, a metabolic panel may be warranted to assess for electrolyte abnormalities and hydration status. Stool studies such as stool culture, Clostridium difficile toxin, and ova and parasite testing are not usually indicated unless symptoms are prolonged or an alternative pathogen is suspected. In cases where norovirus is suspected, a number of enzyme immunoassays and reverse transcription polymerase chain reaction (RT-PCR) are available for the detection of norovirus. Although not usually indicated for individual cases of gastroenteritis, these assays may be useful in detecting norovirus outbreaks. While enzyme immunoassays are the most readily available test, RT-PCR remains the gold standard for detection of norovirus. Both types of tests use stool or emesis samples to detect GI and GII noroviruses. However, limitations do exist for norovirus testing. Many healthcare facilities do not have access to enzyme immunoassays or RT-PCR, and sensitivity and specificity of testing are variable. The accuracy of results is dependent upon the number of samples tested as well as the timing of stool collection and proper handling of the sample. Because laboratory testing for norovirus is not uniformly available, clinical evaluation can be useful in detecting norovirus outbreaks. The Kaplan clinical and epidemiological criteria for norovirus were developed before the development of laboratory testing and are still considered useful when definitive testing is unavailable. [7][8][9]
The Kaplan Criteria
- Vomiting in more than half of symptomatic cases
- Mean (or median) incubation period of 24 to 48 hours
- Mean (or median) duration of illness of 12 to 60 hours
- No bacterial pathogen isolated on stool culture
If all of the Kaplan criteria are positive, there is a high probability of a norovirus outbreak.
Treatment / Management
The management of norovirus infection involves treating the patient’s symptoms and mitigating the risk of a norovirus outbreak. The primary clinical focus should be on the patient’s hydration status with an emphasis on infection control to prevent the spread of disease to healthcare workers and patient contacts. The mainstay of treatment is oral rehydration therapy. The World Health Organization and the American Academy of Pediatrics recommend oral rehydration solutions with electrolytes and glucose. Oral rehydration solutions are preferred over sports drinks and juices for pediatric patients because the latter contain a high carbohydrate and osmotic load that may exacerbate diarrhea. Patients with intractable vomiting or severe dehydration require intravenous hydration and, possibly, hospital admission. Antibiotics generally are not indicated unless there is a concern for bacterial infection. Anti-motility agents have been beneficial in adults, and antiemetics may provide symptomatic relief. Studies support the use of ondansetron in vomiting children, but anti-motility agents are not recommended in pediatric patients. Infection control is a priority in preventing norovirus outbreaks. While efforts at vaccine development are underway, hand hygiene, surface cleaning, and prevention of body fluid exposure are the mainstays of infection control. Norovirus vaccine development remains a priority for both the perceived public health benefits as well as the economic benefits. There has been difficulty developing a vaccine because of the complex nature of norovirus, human immune responses, difficulty culturing the virus, and limited animal models for vaccine testing. A number of vaccines are currently in pre-clinical development, and one has completed Phase II adult clinical trials. Due to viral evolution, development efforts have focused on multivalent vaccines which are similar to influenza vaccines.[10][11][12](B3)
Differential Diagnosis
Differential diagnosis includes rotavirus, cholera, Clostridium difficile, Salmonella, Cryptosporidium, Enterovirus, Escherichia coli, Shigella, Campylobacter, and Vibrio infections. Patients presenting with abdominal pain should have the following differentials considered: mesenteric ischemia, abdominal aortic aneurysm, bowel perforation, ectopic pregnancy, appendicitis, cholecystitis, bowel obstruction, diverticulitis, pancreatitis, pyelonephritis, urinary tract infection testicular or ovarian torsion, myocardial infarction, and pelvic inflammatory disease.
Prognosis
While the vast majority of patients experience no major complications from norovirus infection, over 70,000 hospitalizations and 800 deaths in the United States are attributed to the effects of norovirus each year. Patients at the extremes of age and immunocompromised patients are at the highest risk of adverse outcomes, including death. Specifically, neonatal patients with norovirus infection are at risk for necrotizing enterocolitis, and studies show increased mortality in elderly patients with norovirus infection. Furthermore, immunocompromised patients are at risk for increased severity and a prolonged clinical course of the illness, with diarrhea lasting months to years in some patients.
Complications
- Hypokalemia
- Dehydration
- Hyponatremia
- Metabolic alkalosis
- Renal failure
- Hemolytic uremic syndrome
Consultations
- Infectious disease
- Pediatrician
Deterrence and Patient Education
- Strict hand and personal hygiene
Pearls and Other Issues
- Norovirus is a leading cause of acute gastroenteritis in the United States and worldwide.
- Norovirus is contagious and requires a low inoculum in the host to cause infection. It has a short incubation period of approximately 1 to 2 days, and clinical symptoms typically last 1 to 3 days.
- Proper handwashing is important in disease to prevent the spread of disease.
Enhancing Healthcare Team Outcomes
The management of norovirus is best done with an interprofessional team of healthcare professionals that includes a nurse, an infectious disease expert, pediatrician, epidemiologist, and a pharmacist. Once a diagnosis of norovirus has been made, the key is to prevent further spread of the infection. The nurse is in the prime position to educate the patient and the family about the importance of hand washing. The outpatient nurse must educate food handlers on strict hand hygiene and keep updated on hygienic codes. The food storage environment must be regularly cleaned and disinfected. all individuals who have been diagnosed with norovirus should self-quarantine themselves. Infected children should remain at home until the symptoms subside. [13][14][5](Level 5) The pharmacist should work with the prescriber on ancillary pharmaceutical care, since antibiotics are not part of the regimen. Finally, the pharmacist should encourage the patient to drink ample fluids and remain hydrated, as well as explaining to them that antibiotics are not effective against this type of infection.
Outcomes
In the healthy population, norovirus is a self-limited infection with an excellent outcome. Most people recover within 5-10 days. However, the condition still results in thousands of ER visits and hospital admissions each year because of complications like dehydration and electrolyte deficiencies. The two populations with the worst outcomes are neonates and those who are immunocompromised. The key to preventing the morbidity is to ensure adequate hydration and correction of any electrolyte deficiency. [15][16](Level V)
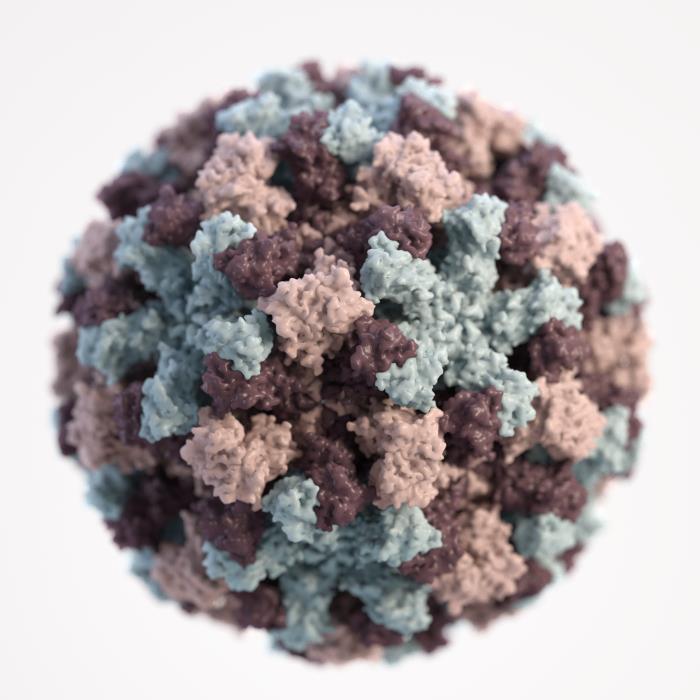
Media
(Click Image to Enlarge)
References
Sell J, Dolan B. Common Gastrointestinal Infections. Primary care. 2018 Sep:45(3):519-532. doi: 10.1016/j.pop.2018.05.008. Epub 2018 Jul 9 [PubMed PMID: 30115338]
Sadkowska-Todys M, Zieliński A, Czarkowski MP. Infectious diseases in Poland in 2016. Przeglad epidemiologiczny. 2018:72(2):129-141 [PubMed PMID: 30111085]
Atmar RL, Ramani S, Estes MK. Human noroviruses: recent advances in a 50-year history. Current opinion in infectious diseases. 2018 Oct:31(5):422-432. doi: 10.1097/QCO.0000000000000476. Epub [PubMed PMID: 30102614]
Level 3 (low-level) evidenceRandazzo W, D'Souza DH, Sanchez G. Norovirus: The Burden of the Unknown. Advances in food and nutrition research. 2018:86():13-53. doi: 10.1016/bs.afnr.2018.02.005. Epub 2018 May 21 [PubMed PMID: 30077220]
Level 3 (low-level) evidenceBányai K, Estes MK, Martella V, Parashar UD. Viral gastroenteritis. Lancet (London, England). 2018 Jul 14:392(10142):175-186. doi: 10.1016/S0140-6736(18)31128-0. Epub 2018 Jun 29 [PubMed PMID: 30025810]
McIntosh EDG. Healthcare-associated infections: potential for prevention through vaccination. Therapeutic advances in vaccines and immunotherapy. 2018 Feb:6(1):19-27. doi: 10.1177/2515135518763183. Epub 2018 Mar 14 [PubMed PMID: 29998218]
Level 3 (low-level) evidenceDe Grazia S, Bonura F, Cappa V, Li Muli S, Pepe A, Urone N, Giammanco GM. Performance evaluation of a newly developed molecular assay for the accurate diagnosis of gastroenteritis associated with norovirus of genogroup II. Archives of virology. 2018 Dec:163(12):3377-3381. doi: 10.1007/s00705-018-4010-8. Epub 2018 Sep 6 [PubMed PMID: 30191373]
Melgaço FG, Corrêa AA, Ganime AC, Brandão MLL, Medeiros VM, Rosas CO, Lopes SMDR, Miagostovich MP. Evaluation of skimmed milk flocculation method for virus recovery from tomatoes. Brazilian journal of microbiology : [publication of the Brazilian Society for Microbiology]. 2018 Nov:49 Suppl 1(Suppl 1):34-39. doi: 10.1016/j.bjm.2018.04.014. Epub 2018 Aug 16 [PubMed PMID: 30166268]
Hyun J, Ko DH, Lee SK, Kim HS, Kim JS, Song W, Kim HS. Evaluation of a New Multiplex Real-Time PCR Assay for Detecting Gastroenteritis-Causing Viruses in Stool Samples. Annals of laboratory medicine. 2018 May:38(3):220-225. doi: 10.3343/alm.2018.38.3.220. Epub [PubMed PMID: 29401556]
Cohen R, Raymond J, Gendrel D. Antimicrobial treatment of diarrhea/acute gastroenteritis in children. Archives de pediatrie : organe officiel de la Societe francaise de pediatrie. 2017 Dec:24(12S):S26-S29. doi: 10.1016/S0929-693X(17)30515-8. Epub [PubMed PMID: 29290231]
Chen Y, Hall AJ, Kirk MD. Norovirus Disease in Older Adults Living in Long-Term Care Facilities: Strategies for Management. Current geriatrics reports. 2017:6(1):26-33. doi: 10.1007/s13670-017-0195-z. Epub 2017 Feb 24 [PubMed PMID: 29204334]
Fisher A, Dembry LM. Norovirus and Clostridium difficile outbreaks: squelching the wildfire. Current opinion in infectious diseases. 2017 Aug:30(4):440-447. doi: 10.1097/QCO.0000000000000382. Epub [PubMed PMID: 28538249]
Level 3 (low-level) evidenceMattison CP, Cardemil CV, Hall AJ. Progress on norovirus vaccine research: public health considerations and future directions. Expert review of vaccines. 2018 Sep:17(9):773-784. doi: 10.1080/14760584.2018.1510327. Epub 2018 Aug 27 [PubMed PMID: 30092671]
Level 3 (low-level) evidenceKambhampati AK, Marsh ZA, Hlavsa MC, Roberts VA, Vieira AR, Yoder JS, Hall AJ. Prevention and Control of Youth Camp-Associated Acute Gastroenteritis Outbreaks. Journal of the Pediatric Infectious Diseases Society. 2019 Nov 6:8(5):392-399. doi: 10.1093/jpids/piy068. Epub [PubMed PMID: 30085136]
Gaythorpe KAM, Trotter CL, Conlan AJK. Modelling norovirus transmission and vaccination. Vaccine. 2018 Sep 5:36(37):5565-5571. doi: 10.1016/j.vaccine.2018.07.053. Epub 2018 Jul 31 [PubMed PMID: 30076105]
Hei H, Bezpalko O, Smathers SA, Coffin SE, Sammons JS. Development of a novel prevention bundle for pediatric healthcare-associated viral infections. Infection control and hospital epidemiology. 2018 Sep:39(9):1086-1092. doi: 10.1017/ice.2018.149. Epub 2018 Jul 20 [PubMed PMID: 30027857]