Introduction
Obstetricians first used ultrasound to diagnose an early intrauterine pregnancy in the 1960s and 1970s. Emergency physicians adapted ultrasound for point-of-care use in the 1990s. Ultrasound is a noninvasive diagnostic modality that can quickly confirm an intrauterine pregnancy at the bedside, significantly shortening the emergency department (ED) length of stay for pregnant patients.[18][1] Point-of-care pelvic ultrasound in the hands of emergency medicine providers yields the highest diagnostic potential in the first trimester period of pregnancy.[2][3] For this reason, the remainder of the article focus is on ultrasound in first-trimester pregnancy.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
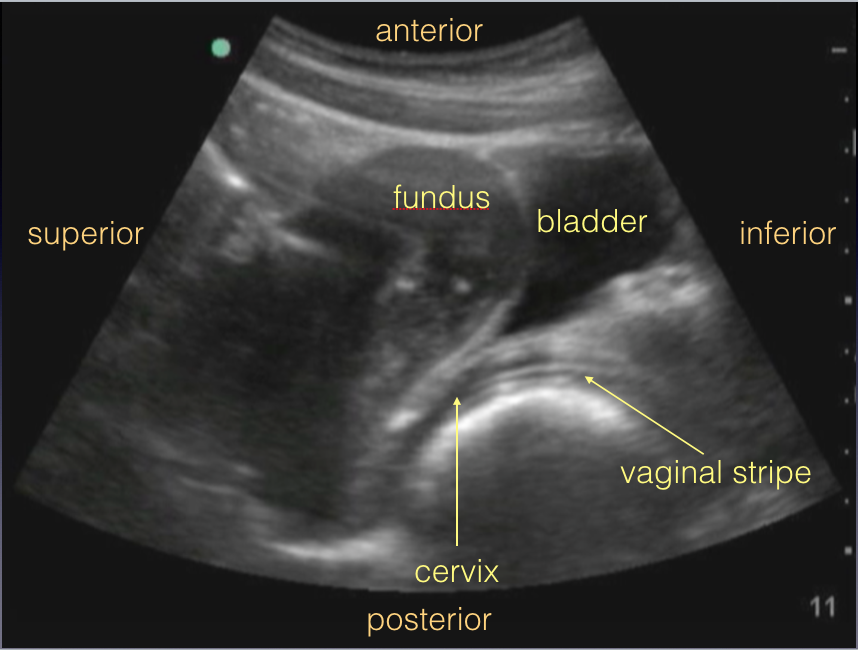
The landmarks of the uterus are the bladder and vaginal stripe. The bladder is located anterior and inferior to the uterus, and the vaginal stripe is a hyperechoic line that is located posterior to the bladder. The vaginal stripe ends at the cervix, and the uterine fundus usually curves up anteriorly (anteverted uterus, approximately 80% of women), but in a smaller subset of females, curves posteriorly (retroverted uterus). The endometrium usually appears as a hyperechoic line in the center of the uterine fundus.
An intrauterine pregnancy (IUP) is confirmed on ultrasound when an intrauterine gestational sac containing a yolk sac and/or a fetal heart rate is visualized with an endomyometrial mantle greater than 7mm. Lack of any of these features would be classified as no definitive intrauterine pregnancy (NDIUP).[4][5][6]
Indications
Vaginal bleeding
- Confirmation of an IUP in the setting of vaginal bleeding in a first-trimester pregnancy effectively rules out an ectopic pregnancy if the pregnancy was conceived without reproductive endocrinology assistance. The diagnosis, in this case, is usually a threatened abortion. NDIUP in the setting of vaginal bleeding warrants further workup for an ectopic pregnancy.[2]
Positive pregnancy test, asymptomatic
- Emergency physicians are often the first providers to ultrasound first trimester pregnancies, as obstetricians will ask a patient to schedule her first appointment at approximately 8 weeks gestation according to her last menstrual period. For this reason, patients will often present to the ED after finding out they are pregnant from a home pregnancy test, sometimes for no other reason other than to formally diagnose the pregnancy. Under these circumstances, an ultrasound should be attempted to confirm the presence of an IUP, as well as to date the fetus if present. While it was once thought the earlier a pregnancy is dated, the more accurate the gestational age, the difference may be too small to justify.[7] However, dating the gestation by using the “crown-rump-length” calculation (CRL) over the longest dimension of the fetal pole without including the yolk sac would be appropriate and important to communiicate to the patient's obstetrician, especially if the patient delayed her first obstetric appointment and ultrasound.[8] If NDIUP is appreciated in an asymptomatic patient, a serum beta-hCG should be ordered, and the patient should arrange for repeat testing in 48 hours with obstetrician follow-up to ensure the hormone is rising appropriately.
Abdominal pain
- Confirmation of an IUP in the setting of abdominal pain effectively rules out an ectopic pregnancy if the pregnancy was conceived without reproductive endocrinology assistance, given the rare incidence of heterotopic pregnancy in these women.
- Confirmation of a live ectopic pregnancy, defined as a gestational sac containing a yolk sac or fetal heartbeat outside the uterus or with an endomyometrial mantle less than or equal to 7 mm (which supports the diagnosis of an interstitial ectopic pregnancy) should lead to prompt obstetrician consultation for operative management.
- In an hCG-positive female with abdominal pain, where the uterus reveals NDIUP as well as free fluid in the pelvis, prompt obstetrician consultation should be sought. If there is additional free fluid in Morison’s pouch, these findings carry high specificity for ectopic pregnancy needing operative management.[9]
Hypotension
- Free peritoneal fluid in Morison’s pouch or the pelvis in a patient with an NDIUP who has a positive urine pregnancy test is highly specific for an ectopic pregnancy requiring operative management.[9]
Hyperemesis gravidarum
- A twin gestation or molar pregnancy may explain significant nausea and vomiting.
If the transabdominal pelvic ultrasound shows NDIUP, a transvaginal ultrasound is indicated. If a female is or has received reproductive endocrine assistance in getting pregnant, early consultation with her reproductive endocrinologist is recommended.[10]
Contraindications
There are no absolute contraindications to performing a transabdominal pelvic ultrasound in early pregnancy. Care should be taken not to scan over a wound or incision to avoid contamination and infection. A transvaginal ultrasound is contraindicated in the setting of hypotension. It is also recommended to use settings that expose the first-trimester fetus to as low as reasonably achievable (ALARA) frequencies by avoiding color and spectral Doppler during the exam.
Equipment
First-trimester pregnancy transabdominal ultrasound should be performed with a low-frequency probe, ideally with a large convex footprint. If a transvaginal ultrasound exam is indicated, an endocavitary probe with sheath can improve visualization of the uterus and adnexal structures. A high-level disinfectant system is needed to clean the endocavitary probe between uses.
Personnel
A trained provider can perform first-trimester pregnancy ultrasound. Emergency physicians are required to correctly perform and interpret a minimum of 25 to 50 cardiac ultrasound exams upon residency graduation.[3]
Preparation
Transabdominal Pelvic Ultrasound
Ideally, the patient’s bladder will be full, as it provides an acoustic window for visualizing the uterus. The patient should be lying supine on a stretcher with her abdomen exposed and towels tucked around the gown and undergarment edges to keep them dry from the ultrasound gel. For dominant right-hand operators, the ultrasound machine should be positioned at the patient’s anatomic right, plugged in (if applicable) and turned on. The lights should be dimmed if possible.[11]
Transvaginal Ultrasound
A transabdominal pelvic ultrasound should always be performed before a transvaginal ultrasound. The patient’s bladder should be as empty as possible before performing a transvaginal ultrasound, to allow the probe to get as close to the uterus and adnexa as possible. To allow adequate visualization of an anteverted uterus, the patient should be positioned in a stretcher with stirrups and her pelvis at the edge of the stretcher, or her pelvis should be elevated approximately 8 cm to 10 cm with an upside-down bedpan and two to three folded chucks.[11]
Technique or Treatment
A low-frequency convex probe is best for a transabdominal pelvic ultrasound. Alternatively, a phased array probe can be used if a convex probe is not available. The settings on the ultrasound machine should be set to "obstetrics" or “pregnancy.” The first view should be a sagittal view through the uterus. The convex probe is placed just superior to the pubic symphysis, with the indicator directed superiorly. The footprint should be directed slightly inferiorly. Structures closest to the probe appear at the top of the screen, and structures further away appear toward the bottom of the screen, so in this view, the top of the screen is anterior, and the bottom of the screen is posterior. The left of the screen represents the direction the indicator is pointing toward, which in this view is superior or cephalad, and the right of the screen is inferior or caudad. The bladder, if full, will take up most of the anterior (top) portion of the screen, ending just superior to the pubic symphysis on the right of the screen. Posterior to the bladder is the vaginal stripe, a hyperechoic line starting at the inferior (right) side of the screen and leading to the cervix and uterus. Fanning to the right and left until the uterus disappears in both directions allows for a complete view of the uterus. If a gestational sac is visualized, interrogation for a yolk sac or fetal heartbeat within the gestational sac, as well as measurement of the thinnest endomyometrial mantle around the gestational sac should take place to confirm the presence of an IUP. If there is a fetal heartbeat, Motion-Mode (M-mode) should be employed to calculate the fetal heartbeat. When selecting M-mode, move the M-mode line to where it crosses through the flicker of the fetal heartbeat before graphing the motion across that line over time. A regular pattern of peaks and troughs should trace out on the screen. Freeze that image and use your calculations menu to select the most appropriate calipers for calculating the fetal heartbeat. By placing your calipers at the start of one peak to the start of the next, the machine should calculate the fetal heart rate based on that distance. Some machines require that the calipers be placed over two beats (start of one peak to the start of the second peak after that peak) to calculate an average fetal heart rate.
Transvaginal ultrasound: The endocavitary probe is a high-frequency transducer with a longer handle compared to other transducers. The footprint is small and tightly curved. The transducer shape in its entirety is analogous to a rifle, where the indicator is the side opposite the “trigger.” Before performing a transvaginal ultrasound, a transabdominal ultrasound should be performed to look for uterine landmarks (vaginal stripe and bladder) as well as an IUP. If NDIUP is appreciated, have the patient empty her bladder and when she returns, place an upside-down bedpan with several chucks underneath her pelvis and, while keeping the patient draped, insert the probe with the indicator pointing anteriorly (toward the ceiling). Watch the decompressed bladder move out of view towards the top left side of the screen. When the bladder is barely out of sight, the probe is at the appropriate depth and by fanning the probe to the left and right, obtain a sagittal view of the uterus. The top of the screen represents the inferior aspect of the patient (cervix), the bottom of the screen represents the superior aspect of the patient, the left of the screen represents the anterior aspect of the patient, and the right of the screen represents the posterior aspect of the patient. The Pouch of Douglas, therefore, is the right lower aspect of the screen. While fanning through the uterus, look for a yolk sac and/or fetal heartbeat to diagnose an IUP.
After interrogating for an IUP as well as for free fluid in the Pouch of Douglas, rotate your probe 90 degrees counterclockwise to visualize the uterus in a transverse (more accurately, coronal) plane, where the top of the screen is still inferior, the bottom of the screen is superior, the left of the screen is the patient’s right, and the right of the screen is the patient’s left. In this plane, the uterus tapers on either side where the fallopian tubes take off. On ultrasound, it is difficult to appreciate the fallopian tubes unless there is a tubal ectopic, or fluid within the tubes (hydrosalpinx or pyosalpinx). However, the areas where the uterus tapers in size on either side are called the cornua. The ovaries typically sit between the cornua and the more lateral iliac vessels and are slightly more hypoechoic than the uterus. After locating the cornua with the indicator pointing toward the patient’s right side, and the footprint steered toward the patient’s right side, fan anteriorly and posteriorly until either an undefined hypoechoic area or a defined ovary with anechoic follicles is appreciated. If an undefined hypoechoic area is seen, apply gentle pressure with the probe until an ovary comes into view. Typical ovarian dimensions are 1.5 cm x 1.5 cm x 3 cm. A simple ovarian cyst is 2.5 cm or greater, whereas a follicle is smaller than 2.5 cm. A corpus luteum cyst, which tends to have a thicker wall than a simple cyst, is frequently appreciated in the first 12 weeks of pregnancy.[11]
Complications
Pelvic ultrasound, like most diagnostic ultrasound applications, is associated with little if any risk. There may be some associated discomfort when pressure is applied to the probe both in transabdominal and transvaginal views.
Clinical Significance
Pelvic ultrasound is a rapid, inexpensive, safe application that expedites the diagnosis of intrauterine pregnancy. [12]Pelvic ultrasound can also expedite management in the setting of a ruptured ectopic pregnancy when free fluid and NDIUP is present.[9]
Enhancing Healthcare Team Outcomes
Pregnany is managed by an interprofessional team that includes nurses and pharmacists. It is important for healthcare workers to know that an obstetric ultrasound is a useful technique for identifying several pregnancy related pathologies. The technique is portable, does not use contrast and can be performed at the bedside.
Media
References
Wilson SP,Connolly K,Lahham S,Subeh M,Fischetti C,Chiem A,Aspen A,Anderson C,Fox JC, Point-of-care ultrasound versus radiology department pelvic ultrasound on emergency department length of stay. World journal of emergency medicine. 2016; [PubMed PMID: 27547276]
Hahn SA,Promes SB,Brown MD, Clinical Policy: Critical Issues in the Initial Evaluation and Management of Patients Presenting to the Emergency Department in Early Pregnancy. Annals of emergency medicine. 2017 Feb; [PubMed PMID: 28126120]
Emergency ultrasound guidelines. Annals of emergency medicine. 2009 Apr; [PubMed PMID: 19303521]
Nyberg DA,Mack LA,Harvey D,Wang K, Value of the yolk sac in evaluating early pregnancies. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 1988 Mar; [PubMed PMID: 3280823]
Lewiss RE,Shaukat NM,Saul T, The endomyometrial thickness measurement for abnormal implantation evaluation by pelvic sonography. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2014 Jul; [PubMed PMID: 24958399]
Doubilet PM, Ultrasound evaluation of the first trimester. Radiologic clinics of North America. 2014 Nov; [PubMed PMID: 25444100]
Doubilet PM, Should a first trimester dating scan be routine for all pregnancies? Seminars in perinatology. 2013 Oct; [PubMed PMID: 24176152]
Tunón K,Eik-Nes SH,Grøttum P,Von Düring V,Kahn JA, Gestational age in pregnancies conceived after in vitro fertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter. Ultrasound in obstetrics [PubMed PMID: 10776011]
Moore C,Todd WM,O'Brien E,Lin H, Free fluid in Morison's pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007 Aug; [PubMed PMID: 17554008]
Rodgers SK,Chang C,DeBardeleben JT,Horrow MM, Normal and Abnormal US Findings in Early First-Trimester Pregnancy: Review of the Society of Radiologists in Ultrasound 2012 Consensus Panel Recommendations. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015 Nov-Dec; [PubMed PMID: 26562242]
Level 3 (low-level) evidenceLevine D, Ectopic pregnancy. Radiology. 2007 Nov; [PubMed PMID: 17940301]
Panebianco NL,Shofer F,Fields JM,Anderson K,Mangili A,Matsuura AC,Dean AJ, The utility of transvaginal ultrasound in the ED evaluation of complications of first trimester pregnancy. The American journal of emergency medicine. 2015 Jun; [PubMed PMID: 25817202]