Introduction
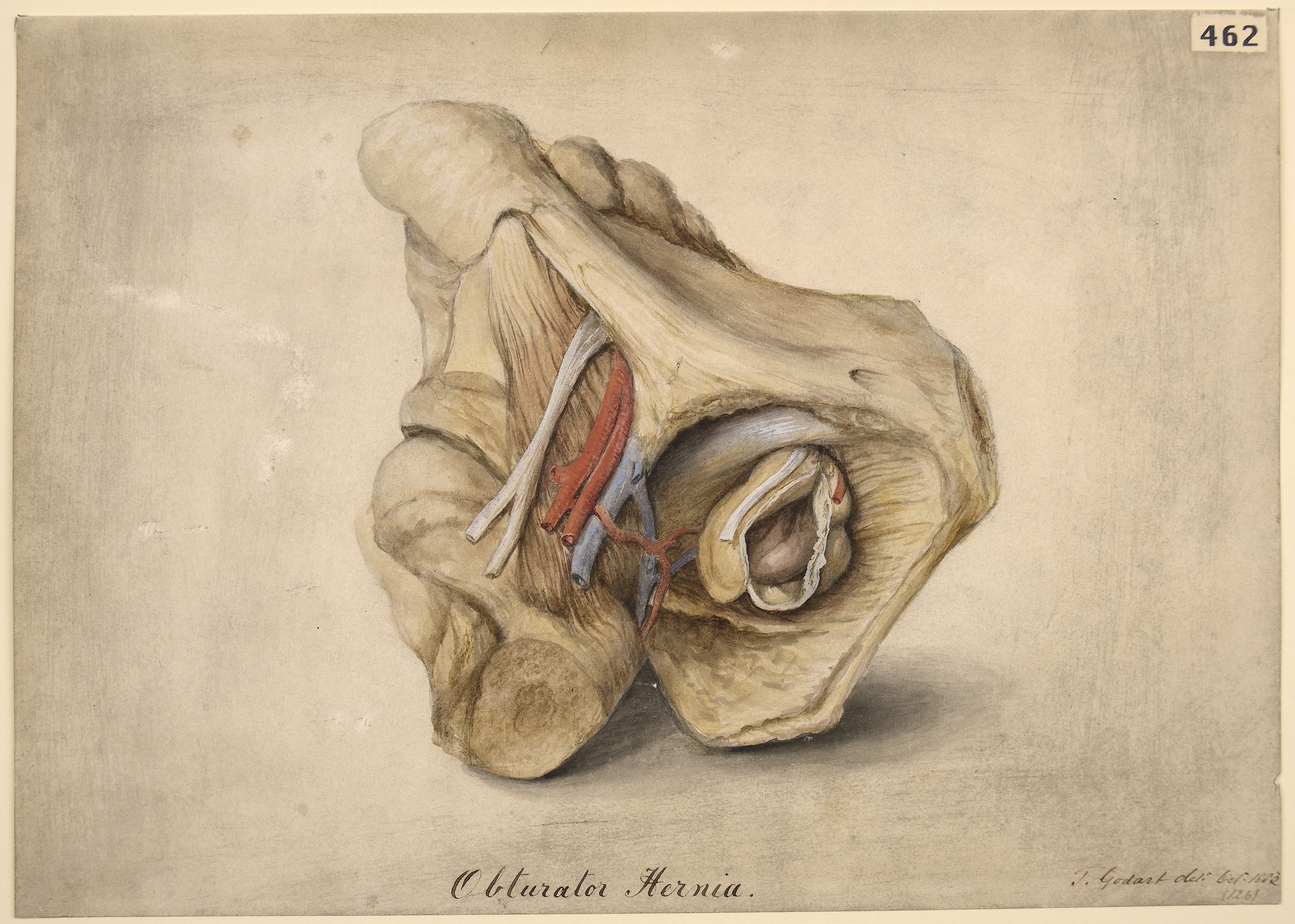
Obturator herniae are uncommon presentations of abdominal pain, comprising <0.04% of all herniae[1] An obturator hernia occurs when abdominal contents traverse the obturator foramen. As this is a small opening in the pelvis, there is an increased propensity for these herniae to get incarcerated and subsequently strangulated obturator hernia.[2] See Image. Obturator Hernia.
The diagnosis of an obturator hernia can be difficult, with the late presentation and often poor functional status of the patient.[3] A high index of suspicion is required in the elderly population, and even then, diagnosis may not be achieved without imaging or operative findings.
The treatments of obturator herniae are manifold, with multiple reports now available of minimally invasive methods of treating these cases.[4][5] Patient selection is important in all cases, and a swift resolution of the patient state is crucial.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
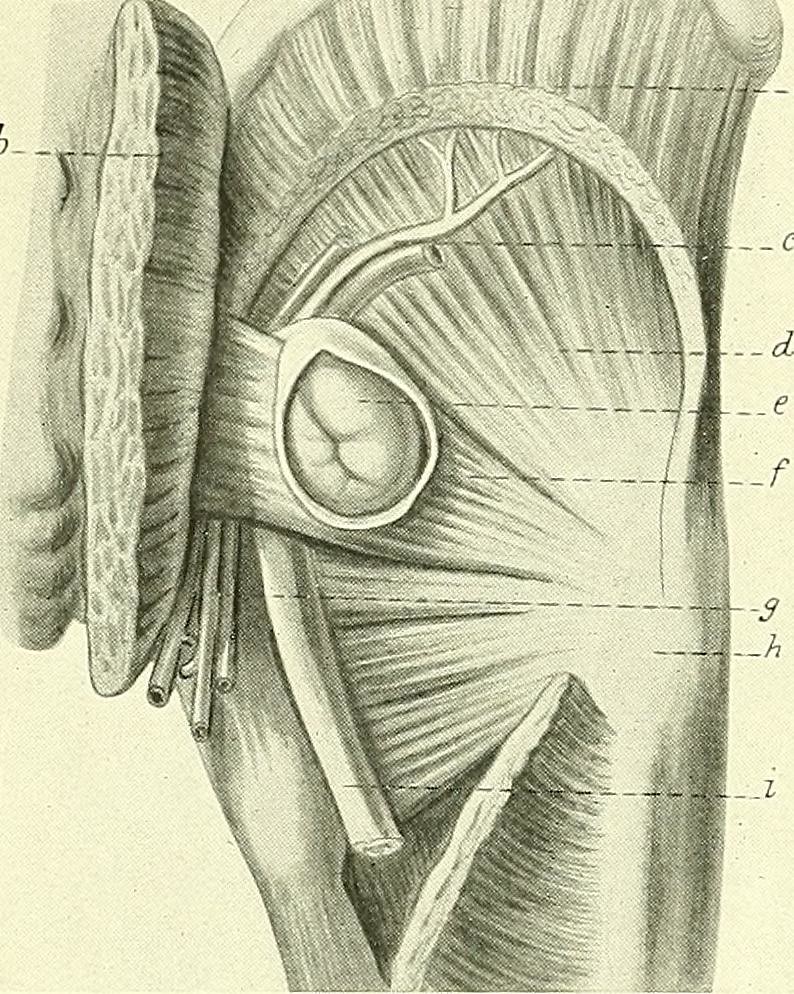
The obturator foramen is an opening in the pelvis created by the ischium and pubis bones. The foramen itself is covered by a quadrella musculoaponeurotic membrane – the obturator membrane. The neurovascular bundle (obturator artery, vein, and nerve) pierces this membrane anterosuperiorly, then passes through the obturator canal. The obturator canal starts as the obturator groove, becoming the obturator canal by a ligamentous band attaching to the posterior and anterior obturator tubercle. This canal connects the pelvis to the medial compartment of the thigh. The obturator canal is about 0.2 to 0.5 cm wide, and 2to 3cm long.[6] The obturator nerve is the most cranial of the neurovascular bundle passing through the canal. It subsequently then divides upon exiting the canal into an anterior and posterior division.
The obturator membrane is covered on either side by the obturator muscles. As such, any hernia that forms will pass through obturator internus, the obturator membrane, and obturator externus in that order. The natural location for the hernial sac to lie after its passage through these structures is deep and inferior to the pectineus muscle, superficial to obturator externus. However, the hernia could protrude through the obturator externus muscle, taking with it the posterior obturator nerve. In this position, the hernial sac lies posterior to the adductor brevis. Very rarely, the hernial sac can be found between the obturator internus and externus muscles.
The obturator foramen has a different shape according to the sex of the individual. Women tend to have triangular, wider foramina, while men tend to have more oval ones.
Epidemiology
Obturator herniae are called ‘the skinny old woman hernia’. This is due to the high incidence of these herniae in women in their seventh or eighth decade, who are normally gaunt (8), and indeed it can almost be said to be found almost exclusively in women.[1][7] As alluded to before, this might be explained by the different shape of the obturator canal in women – having a wider transverse measurement, that is more obliquely placed, thus allowing for the easier passage of the hernial contents. Multiparity may also lead to structural changes in the tissues, allowing for an obturator canal that is more likely to expand and allow for herniation through it.[8] Bilateral obturator herniae are rare, possibly due to the presence of the sigmoid colon on the left.[9][10]
History and Physical
Obturator hernias are rarely diagnosed in a non-symptomatic patient, with the majority of cases presenting as an emergency with intestinal obstruction (see Image. Intestinal Coil).[1][6][7][11] The presentation of a strangulated obturator hernia is rare, with it being less than 0.04% of all hernias.[12] However, in an emaciated elderly female presenting with intestinal obstruction, this should be considered as a possible diagnosis. This is especially so in the case of a virgin abdomen in this population – thereby raising suspicion of a cause other than adhesions.
The intimate relationship of the hernia with the obturator nerve could lead to the presence of the Howship-Romberg sign. This is obturator neuralgia, causing pain in the medial thigh that is relieved by flexing the hip and exacerbated by extension, adduction, and medial rotation of the hip. The Hannington-Kiff sign is an absent adductor reflex in the thigh. This is elicited by placing a finger on the adductors 5 cm above the knee, then percussing said finger with a tendon hammer. A contraction of muscle indicated an adductor reflex that is present. The Hannington-Kiff sign is more specific than the Howship-Romberg sign, but could be hard to elicit, and is operator dependent.[13]
Evaluation
It is important to note that the physical signs of an obturator hernia are operator dependent and may not be immediately evident. In these cases, it would be prudent to perform computed tomography (CT) scan to achieve an adequate diagnosis, with a reported diagnostic accuracy of up to 90%.[14]
The patient would also require general labs to be worked up for a possible operative procedure as per local protocol.
Treatment / Management
Invariably, treatment is required of these hernias due to the likelihood of there being strangulation of the hernia. Also, these hernias often require treatment as an emergency procedure, as it is unlikely that the obturator hernia is likely to be reducible.
The treatment options for an obturator hernia are thus to be decided between an open and laparoscopic procedure. Laparoscopic hernia repairs are becoming more prevalent, with a number of reports of obturator hernia being repaired via a minimally-invasive approach [7],[15],[16]. Given the location of this hernia deep within the pelvis, a laparoscopic approach allows for clear visualisation of the contents of the hernia and subsequent treatment. Almost all case reports published have described a transabdominal preperitoneal (TAPP) approach.[15][16][17][18] This would allow the surgeon to visually inspect the contents of the hernia, and if bowel were present, to assess the viability of the incacerated/strangulated bowel. If a bowel resection were required, this could be performed either laparoscopically or via conversion to an open operation, depending on the experience of the operating surgeon.(B2)
The operative steps in an open procedure remain the same for any strangulated hernia repair – requiring a lower midline laparotomy, identification of the hernia, inspection of the contents, with possible bowel resection and anastomosis, followed by repair of the hernial orifice with either primary suture repair or with mesh placement [19]. Other approaches are described, including retropubic and inguinal approaches; however, these should be performed by surgeons with experience in such approaches.[20] A lower midline laparotomy being a very common approach may be one that surgeons would be more familiar with, and less likely to cause any issues.
The laparoscopic approach has been described previously. For a TAPP repair, pneumoperitoneum is achieved (normally via an open Hassen technique), with ports placed 5cm either side of the midline below the umbilicus. This is especially so as it would be prudent for the clinical evaluation of the contralateral side (if initially diagnosed with a unilateral obturator hernia), as there might be missed bilateral herniae in this population.[21] Once the hernial sac is identified, it is gently retracted using careful dissection if required. The hernial contents are visualized, paying attention to the bowel if present. A bowel resection may be required and will follow well-established operative steps. The excess hernial sac may be left behind, avoiding unnecessary dissection. The final part of the procedure would be the placement of a mesh. An incision is made on the anterior aspect of the abdomen using diathermy. This incision is then extended using sharp dissection, thus allowing the surgeon to tease the peritoneum alone away from the pre-peritoneal fat. Once adequate space is created, a mesh may be placed in this space. The peritoneal covering is then sutured closed.
Differential Diagnosis
It is important to note that an obturator hernia is still a rare hernia. In the presence of absolute constipation in an elderly patient, it becomes important to try and elicit whether this could be a small or large bowel obstruction. Small bowel obstruction in this population is commonly due to hernias, adhesions, and tumors, whereas large bowel adhesions are likely due to tumors, hernia, and volvulus. The diagnosis will require a form of cross sectional imaging, commonly a CT scan, after ensuring the patient is appropriately resuscitated.
Prognosis
Obturator herniae pose an interesting challenge in estimating mortality - due to their rare presentation. Historically, the mortality has been estimated between 13% to 40% and has been reported in more recent reports as well.[22][23][24] Equally, the morbidity of the condition relates to the late presentation and identification of the problem. This can lead to infective complications (such as the development of collections) and anastomotic leaks (due to bowel resections).[25]
Complications
The complications from an obturator hernia follow any other hernia, including strangulation (leading to bowel resection and associated complications), damage to the obturator nerve due to compressive symptoms, along with associated operative complications.
Postoperative and Rehabilitation Care
The postoperative care for these patients should follow existing local protocol for any bowel resection (if performed) or emergency hernia repair. This would include adequate analgesia, bowel rest (following any early recovery scheme implemented locally), and wound care. This would be followed by early introduction of oral intake and mobilization.
There are no established protocols regarding the routine follow up of these patients. Generally, a postoperative follow up at 2 and 6 weeks following the operation might be required to ensure continued healing and patient satisfaction.
Deterrence and Patient Education
Obturator herniae are not a preventable condition, and indeed, the diagnosis being so rare precludes any long term study of the condition appropriately. However, the treating physician needs to be aware of this condition, especially in the appropriate age group.
Enhancing Healthcare Team Outcomes
The treatment of an obturator hernia would invariably involve co-ordination of care from different grades of healthcare professionals. The emergency department will most likely be the first point of contact for these patients. The presentation of any individual with severe abdominal pain and bowel obstruction warrants a thorough investigation with appropriate blood tests and imaging. However, the patient should be of the utmost importance in these cases, and they will most likely be in severe pain. Appropriate communication between the physicians and the nursing staff to ensure the delivery of analgesia is essential. The placement of a nasogastric tube might be warranted in cases of intestinal obstruction.
Radiologists play an important role in the diagnosis of these cases, and this involves the handover of important information for them to perform an adequate scan. Obturator herniae may be difficult to call on a CT scan, and therefore require the radiologist to be actively looking for it.
The involvement of the surgical team constitutes a major part of patient care - and this especially requires close monitoring from the intensive care and nursing staff within the team. Post-operatively these patients will require close monitoring, keeping in mind the mortality of such cases.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chung CC, Mok CO, Kwong KH, Ng EK, Lau WY, Li AK. Obturator hernia revisited: a review of 12 cases in 7 years. Journal of the Royal College of Surgeons of Edinburgh. 1997 Apr:42(2):82-4 [PubMed PMID: 9114674]
Level 2 (mid-level) evidenceMnari W, Hmida B, Maatouk M, Zrig A, Golli M. Strangulated obturator hernia: a case report with literature review. The Pan African medical journal. 2019:32():144. doi: 10.11604/pamj.2019.32.144.14846. Epub 2019 Mar 26 [PubMed PMID: 31303916]
Level 3 (low-level) evidenceGilbert JD, Byard RW. Obturator hernia and the elderly. Forensic science, medicine, and pathology. 2019 Sep:15(3):491-493. doi: 10.1007/s12024-018-0046-z. Epub 2018 Nov 5 [PubMed PMID: 30397870]
Shapiro K,Patel S,Choy C,Chaudry G,Khalil S,Ferzli G, Totally extraperitoneal repair of obturator hernia. Surgical endoscopy. 2004 Jun; [PubMed PMID: 15095078]
Level 2 (mid-level) evidenceWu JM, Lin HF, Chen KH, Tseng LM, Huang SH. Laparoscopic preperitoneal mesh repair of incarcerated obturator hernia and contralateral direct inguinal hernia. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2006 Dec:16(6):616-9 [PubMed PMID: 17243881]
Level 3 (low-level) evidenceLosanoff JE, Richman BW, Jones JW. Obturator hernia. Journal of the American College of Surgeons. 2002 May:194(5):657-63 [PubMed PMID: 12022607]
Mantoo SK, Mak K, Tan TJ. Obturator hernia: diagnosis and treatment in the modern era. Singapore medical journal. 2009 Sep:50(9):866-70 [PubMed PMID: 19787172]
Level 3 (low-level) evidenceDhital B,Gul-E-Noor F,Downing KT,Hirsch S,Boutis GS, Pregnancy-Induced Dynamical and Structural Changes of Reproductive Tract Collagen. Biophysical journal. 2016 Jul 12; [PubMed PMID: 27410734]
Chowbey PK, Bandyopadhyay SK, Khullar R, Soni V, Baijal M, Wadhwa A, Sharma A. Endoscopic totally extraperitoneal repair for occult bilateral obturator hernias and multiple groin hernias. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2004 Oct:14(5):313-6 [PubMed PMID: 15630949]
Level 3 (low-level) evidenceGlicklich M, Eliasoph J. Incarcerated obturator hernia: case diagnosed at barium enema fluoroscopy. Radiology. 1989 Jul:172(1):51-2 [PubMed PMID: 2740520]
Level 3 (low-level) evidenceBergstein JM, Condon RE. Obturator hernia: current diagnosis and treatment. Surgery. 1996 Feb:119(2):133-6 [PubMed PMID: 8571196]
Level 3 (low-level) evidenceZiegler DW, Rhoads JE Jr. Obturator hernia needs a laparotomy, not a diagnosis. American journal of surgery. 1995 Jul:170(1):67-8 [PubMed PMID: 7793500]
Naude G, Bongard F. Obturator hernia is an unsuspected diagnosis. American journal of surgery. 1997 Jul:174(1):72-5 [PubMed PMID: 9240957]
Ijiri R, Kanamaru H, Yokoyama H, Shirakawa M, Hashimoto H, Yoshino G. Obturator hernia: the usefulness of computed tomography in diagnosis. Surgery. 1996 Feb:119(2):137-40 [PubMed PMID: 8571197]
Level 2 (mid-level) evidenceNg DC, Tung KL, Tang CN, Li MK. Fifteen-year experience in managing obturator hernia: from open to laparoscopic approach. Hernia : the journal of hernias and abdominal wall surgery. 2014 Jun:18(3):381-6. doi: 10.1007/s10029-013-1080-0. Epub 2013 Apr 2 [PubMed PMID: 23546862]
Level 2 (mid-level) evidenceLiu J, Zhu Y, Shen Y, Liu S, Wang M, Zhao X, Nie Y, Chen J. The feasibility of laparoscopic management of incarcerated obturator hernia. Surgical endoscopy. 2017 Feb:31(2):656-660. doi: 10.1007/s00464-016-5016-5. Epub 2016 Jun 10 [PubMed PMID: 27287915]
Level 2 (mid-level) evidenceHaith LR Jr, Simeone MR, Reilly KJ, Patton ML, Moss BE, Shotwell BA. Obturator hernia: laparoscopic diagnosis and repair. JSLS : Journal of the Society of Laparoendoscopic Surgeons. 1998 Apr-Jun:2(2):191-3 [PubMed PMID: 9876738]
Level 3 (low-level) evidenceAmiki M, Goto M, Tomizawa Y, Sugiyama A, Sakon R, Inoue T, Ito S, Oneyama M, Shimojima R, Hara Y, Narita K, Tachimori Y, Sekikawa K. Laparoscopic transabdominal preperitoneal hernioplasty for recurrent obturator hernia: A case report. Asian journal of endoscopic surgery. 2020 Jul:13(3):457-460. doi: 10.1111/ases.12739. Epub 2019 Jul 22 [PubMed PMID: 31332930]
Level 3 (low-level) evidenceSze Li S, Kenneth Kher Ti V. Two different surgical approaches for strangulated obturator hernias. The Malaysian journal of medical sciences : MJMS. 2012 Jan:19(1):69-72 [PubMed PMID: 22977378]
Petrie A, Tubbs RS, Matusz P, Shaffer K, Loukas M. Obturator hernia: anatomy, embryology, diagnosis, and treatment. Clinical anatomy (New York, N.Y.). 2011 Jul:24(5):562-9. doi: 10.1002/ca.21097. Epub 2011 Feb 14 [PubMed PMID: 21322061]
Nakayama T, Kobayashi S, Shiraishi K, Nishiumi T, Mori S, Isobe K, Furuta Y. Diagnosis and treatment of obturator hernia. The Keio journal of medicine. 2002 Sep:51(3):129-32 [PubMed PMID: 12371643]
Arbman G. Strangulated obturator hernia. A simple method for closure. Acta chirurgica Scandinavica. 1984:150(4):337-9 [PubMed PMID: 6377785]
Level 3 (low-level) evidenceYokoyama Y, Yamaguchi A, Isogai M, Hori A, Kaneoka Y. Thirty-six cases of obturator hernia: does computed tomography contribute to postoperative outcome? World journal of surgery. 1999 Feb:23(2):214-6; discussion 217 [PubMed PMID: 9880435]
Level 2 (mid-level) evidenceLo CY, Lorentz TG, Lau PW. Obturator hernia presenting as small bowel obstruction. American journal of surgery. 1994 Apr:167(4):396-8 [PubMed PMID: 8179083]
Yip AW, AhChong AK, Lam KH. Obturator hernia: a continuing diagnostic challenge. Surgery. 1993 Mar:113(3):266-9 [PubMed PMID: 8441961]