Introduction
The oculocardiac reflex (OCR), also known as the Aschner reflex or trigeminovagal reflex, was first described in 1908 as a heart rate diminishment when direct pressure is placed on the eyeball. The heart rate is characteristically decreased by over 20% following globe pressure or extraocular muscle traction. The OCR typically leads to sinus bradycardia, though arterial pressure reduction, arrhythmia, asystole, and even cardiac arrest have also been documented arising from this reflex. Ophthalmic procedures, particularly strabismus surgery, often induce the OCR. Facial trauma, regional anesthetic nerve blocks, and mechanical stimulation may also trigger this reflex.[1][2][3]
The OCR's incidence is reported to be anywhere from 14% to 90% and decreases with age. Pediatric populations face the highest risk of OCR development due to their increased susceptibility. Young individuals are also particularly vulnerable to OCR's complications due to their heavy dependence on the heart rate for maintaining cardiac output. The OCR's varying occurrence and severity are linked to factors like hypoxia, hypercarbia, acidosis, and the anesthetic agent type employed during surgery.[4][5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The OCR arc consists of an afferent and efferent limb (see Image. Schematic Diagram of Trigeminal Nerve Stimulation Effects). The trigeminal or 5th cranial nerve (CN V) comprises the reflex's afferent or sensory limb. The vagus or 10th cranial nerve (CN X) constitutes the efferent OCR limb. Ocular and periorbital stretch receptors activate this pathway.
The short and long ciliary nerves conduct impulses that carry the sensory message to the ciliary ganglion. The impulses are then transported via CN V's ophthalmic division to the Gasserian ganglion, followed by the trigeminal nucleus, where the afferent limb terminates in the central nervous system (CNS). The CNS processes the sensory input, facilitating communication between the trigeminal sensory nucleus and the vagus nerve's visceral motor nucleus. The outflow triggers the efferent limb, sending impulses from the brainstem to the myocardium, specifically the sinoatrial node, activating the vagal motor response. Negative chronotropy consequently arises, causing bradycardia.
Risk Factors
The OCR is often triggered by extraocular muscle traction, with the medial rectus muscle most commonly implicated. However, some studies show no particular muscle significantly associated with increased OCR occurrence.
Additional stimuli linked to OCR activation include direct globe pressure, ocular manipulation, and ocular pain. Retrobulbar blocks, ocular hematomas, and facial or orbital trauma may also activate the reflex due to increased pressure. However, the OCR is fatigable, decreasing in intensity with multiple, repeated stimuli.[6][7][8]
Complications
The OCR's complications arise from vagal responses and may include the following:
- Sinus bradycardia
- Arrhythmia
- Reduced atrial pressure
- Ventricular tachycardia
- Ventricular fibrillation
- Multifocal premature ventricular contractions
- Ventricular bigeminy
- Asystole
- Cardiac arrest
- Dizziness
- Lightheadedness
- Nausea
- Weakness
Prompt recognition and management are essential to avert significant morbidity and mortality.
Clinical Significance
Bradycardia is the OCR's most common manifestation, though it may deteriorate to potentially fatal arrhythmias, asystole, and cardiac arrest. Apt et al (1973) and Espahbodi et al (2015) reported OCR occurrence rates in patients undergoing ophthalmologic surgeries to be 67.9% and 63%, respectively. Most patients do not experience detrimental outcomes following OCR activation, but its effects can be potentially injurious.[9][10][11]
OCR activation has also been linked to noncardiac manifestations, including hypotension, syncope, and gastrointestinal symptoms like nausea and vomiting due to the vagal motor response. Vagal effects may influence postoperative nausea and vomiting severity. Nausea and vomiting rates in pediatric patients can reach 85% poststrabismus surgery, making it a leading cause of inpatient admission after outpatient procedures.
Emphasis must be given to the immediate cessation of the triggering stimulus as the only definitive treatment when addressing OCR prevention, treatment, and complications. Relieving eye or orbital pressure can deactivate the reflex. Proceeding cautiously is essential after removing the source. However, stimulus withdrawal may be more challenging in uncontrolled situations like trauma. Pharmacological management with cardiac monitoring may be necessary in instances where the OCR may develop.
The occurrence of the reflex may be reduced by choosing the appropriate anesthetic, as some agents are associated with a greater risk of OCR activation than others. Studies indicate that pretreatment with intravenous anticholinergics like atropine or glycopyrrolate decreases OCR incidence. Atropine blocks peripheral cardiac muscarinic receptors, increasing sinoatrial node firing and atrioventricular node conduction and countering OCR's vagal outflow.
Ketamine may also counteract vagal stimulation by enhancing sympathetic activity. Choi et al. reported lower OCR incidence with ketamine infusion than sevoflurane, halothane, and propofol. Espahbodi et al. (2015) found ketamine superior to atropine in OCR reduction. Other studies associated ketamine with a lower incidence of postoperative nausea, vomiting, and agitation.
Blunting the afferent OCR limb may also decrease its occurrence. Retro- or peribulbar blocks with xylocaine hydrochloride can block the ciliary ganglion. Combining with other agents known to decrease OCR incidence, such as atropine, can further prevent OCR activation.
Fast-acting opioids like fentanyl, sufentanil, and remifentanil can precipitate OCR and induce bradycardia. Many anesthetic agents' effects on the OCR have been studied, but several require further investigation. Preanesthetic medications like atropine and retrobulbar blocks should be routinely used during ocular procedures or when managing eye trauma to mitigate OCR effects and safeguard patients.
Enhancing Healthcare Team Outcomes
Manipulating the orbit poses a potential challenge in the operating room due to various stimuli activating the OCR. Therefore, anesthesiologists, ophthalmologists, maxillofacial surgeons, trauma teams, anesthesia nurses, and emergency medicine physicians working with orbital or facial structures must be aware of this reflex, its potential consequences, and strategies for managing or preventing its occurrence.
Vigilance and comprehensive monitoring are paramount to early detection and intervention in patient care. Clinicians must take advantage of diagnostic modalities like electrocardiography and blood pressure monitoring when caring for at-risk patients. The healthcare team must also be prepared to seamlessly administer drugs like atropine and glycopyrrolate and initiate Advanced Cardiac Life Support when necessary. Preparedness and vigilance are vital for promptly identifying and addressing potential complications, especially if symptomatic bradycardia or cardiac arrest arises from OCR activation. Continuous monitoring allows healthcare providers to intervene swiftly, potentially saving lives and enhancing patient outcomes.
Media
(Click Image to Enlarge)
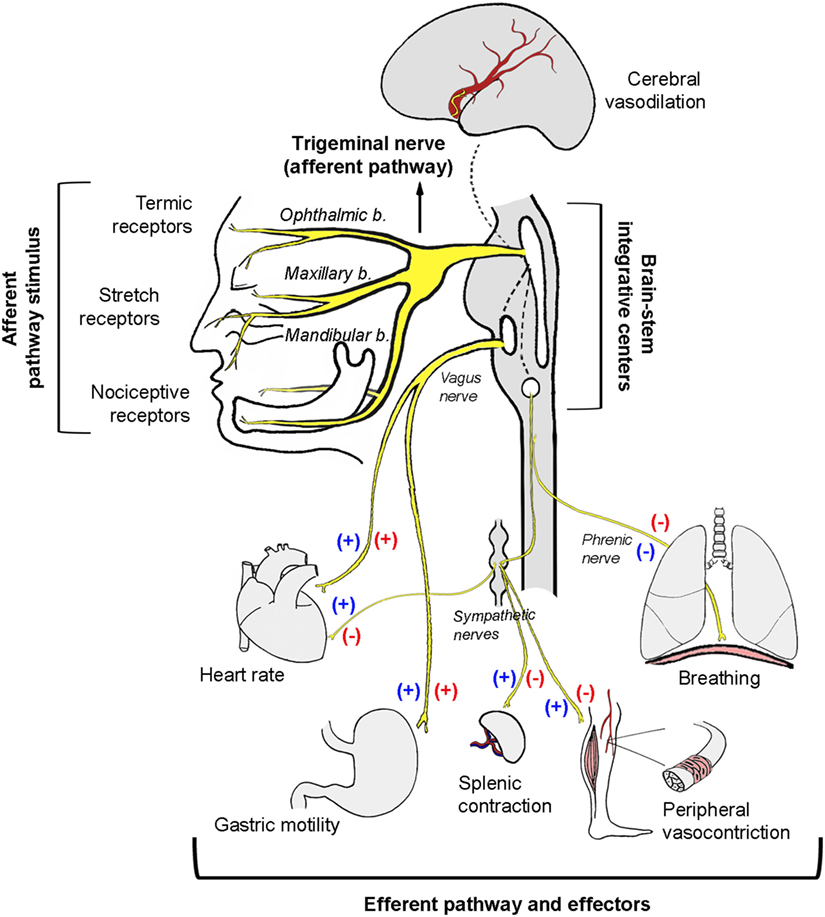
Schematic Diagram of Trigeminal Nerve Stimulation Effects. Protective reflexes such as the diving, nasopharyngeal, and oculocardiac reflexes, involve coactivation of both autonomic limbs (blue symbols). The trigeminocardiac reflex triggers a robust depressor response through reciprocal parasympathetic activation and sympathetic system inhibition (red symbols).
Buchholz B, Kelly J, Bernatene EA, Mendez Diodati N, Gelpi RJ. Antagonistic and synergistic activation of cardiovascular vagal and sympathetic motor outflows in trigeminal reflexes. Front Neurol. 2017;8:52.
doi: 10.3389/fneur.2017.00052
References
Waldschmidt B, Gordon N. Anesthesia for pediatric ophthalmologic surgery. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2019 Jun:23(3):127-131. doi: 10.1016/j.jaapos.2018.10.017. Epub 2019 Apr 14 [PubMed PMID: 30995517]
Dunphy L, Anand P. Paediatric orbital trapdoor fracture misdiagnosed as a head injury: a cautionary tale! BMJ case reports. 2019 Apr 3:12(4):. doi: 10.1136/bcr-2018-228739. Epub 2019 Apr 3 [PubMed PMID: 30948403]
Level 3 (low-level) evidenceArnold RW, Bond AN, McCall M, Lunoe L. The oculocardiac reflex and depth of anesthesia measured by brain wave. BMC anesthesiology. 2019 Mar 14:19(1):36. doi: 10.1186/s12871-019-0712-z. Epub 2019 Mar 14 [PubMed PMID: 30871507]
Rahimi Varposhti M, Moradi Farsani D, Ghadimi K, Asadi M. Reduction of oculocardiac reflex with Tetracaine eye drop in strabismus surgery. Strabismus. 2019 Mar:27(1):1-5. doi: 10.1080/09273972.2018.1561732. Epub 2019 Mar 4 [PubMed PMID: 30831045]
Jean YK, Kam D, Gayer S, Palte HD, Stein ALS. Regional Anesthesia for Pediatric Ophthalmic Surgery: A Review of the Literature. Anesthesia and analgesia. 2020 May:130(5):1351-1363. doi: 10.1213/ANE.0000000000004012. Epub [PubMed PMID: 30676353]
Shakil H, Wang AP, Horth DA, Nair SS, Reddy KKV. Trigeminocardiac Reflex: Case Report and Literature Review of Intraoperative Asystole in Response to Manipulation of the Temporalis Muscle. World neurosurgery. 2019 Feb:122():424-427. doi: 10.1016/j.wneu.2018.10.186. Epub 2018 Nov 3 [PubMed PMID: 30399470]
Level 3 (low-level) evidenceDucloyer JB, Couret C, Magne C, Lejus-Bourdeau C, Weber M, Le Meur G, Lebranchu P. Prospective evaluation of anesthetic protocols during pediatric ophthalmic surgery. European journal of ophthalmology. 2019 Nov:29(6):606-614. doi: 10.1177/1120672118804798. Epub 2018 Oct 3 [PubMed PMID: 30280604]
Başağaoğlu B, Steinberg A, Tung IT, Olorunnipa S, Maricevich RS. Oculocardiac Reflex as a Late Presentation of Orbital Floor Fracture. The Journal of craniofacial surgery. 2018 Oct:29(7):e720-e722. doi: 10.1097/SCS.0000000000004966. Epub [PubMed PMID: 30192295]
Bloch M. Oculocardiac reflex: 'My heart just stopped'. Emergency medicine Australasia : EMA. 2018 Aug:30(4):592-593. doi: 10.1111/1742-6723.13113. Epub 2018 May 24 [PubMed PMID: 29797424]
Arnold RW, Biggs RE, Beerle BJ. Intravenous dexmedetomidine augments the oculocardiac reflex. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2018 Jun:22(3):211-213.e1. doi: 10.1016/j.jaapos.2018.01.016. Epub 2018 May 5 [PubMed PMID: 29733898]
DesPain AW, Chapman J, Shaukat H. Oculocardiac Reflex in a Pediatric Trauma Patient. Pediatric emergency care. 2020 Jul:36(7):e399-e401. doi: 10.1097/PEC.0000000000001429. Epub [PubMed PMID: 29489611]