Introduction
Osteoarthritis (OA) is the most common form of arthritis in the world. It can be classified into 2 categories: primary osteoarthritis and secondary osteoarthritis. Classically, OA presents with joint pain and loss of function; however, the disease is clinically very variable and can present merely as an asymptomatic incidental finding to a devastating and permanently disabling disorder.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Risk factors for developing OA include age, female gender, obesity, anatomical factors, muscle weakness, and joint injury (occupation/sports activities).
Primary OA is the most common subset of the disease and is diagnosed in the absence of a predisposing trauma or disease but is associated with the risk factors listed above.
Secondary OA occurs with a preexisting joint abnormality. Predisposing conditions include trauma or injury, congenital joint disorders, inflammatory arthritis, avascular necrosis, infectious arthritis, Paget disease, osteopetrosis, osteochondritis dissecans, metabolic disorders (hemochromatosis, Wilson’s disease), hemoglobinopathy, Ehlers-Danlos syndrome, or Marfan syndrome.[4][5]
Epidemiology
OA affects about 3.3 to 3.6% of the population globally. It causes moderate to severe disability in 43 million people, making it the 11th most debilitating disease worldwide. In the United States, it is estimated that 80% of the population over 65 years old has radiographic evidence of OA, although only 60% of this subset has symptoms. This is because radiographic OA is at least twice as common as symptomatic OA. Therefore, radiographic changes do not prove that OA is the cause of the patient’s joint pain. In 2011, there were almost 1 million hospitalizations for OA, with an aggregate cost of nearly $15 billion, making it the second most expensive disease seen in the United States.[1][3]
Pathophysiology
OA is a disease of the entire joint sparing no tissues. The cause of OA is an interplay of risk factors (mentioned above), mechanical stress, and abnormal joint mechanics. The combination leads to pro-inflammatory markers and proteases that eventually mediate joint destruction. The complete pathway that leads to the destruction of the entire joint is unknown.
Usually, the earliest changes that occur in OA are at the level of the articular cartilage that develops surface fibrillation, irregularity, and focal erosions. These erosions eventually extend down to the bone and continually expand to involve more of the joint surface. On a microscopic level, after cartilage injury, the collagen matrix is damaged, causing chondrocytes to proliferate and form clusters. A phenotypic change to hypertrophic chondrocyte occurs, causing cartilage outgrowths that ossify and form osteophytes. As more of the collagen matrix is damaged, chondrocytes undergo apoptosis. Improperly mineralized collagen causes subchondral bone thickening; in advanced disease, bone cysts infrequently occur. Even rarer, bony erosions appear in erosive OA.
There is also some degree of synovial inflammation and hypertrophy, although this is not the inciting factor as is the case with inflammatory arthritis. Soft-tissue structures (ligaments, joint capsule, menisci) are also affected. In end-stage OA, both calcium phosphate and calcium pyrophosphate dihydrate crystals are present. Their role is unclear, but they are thought to contribute to synovial inflammation.[6][7][8]
History and Physical
The presentation and progression of OA vary greatly from person to person. The triad of symptoms of OA is joint pain, stiffness, and locomotor restriction. Patients can also present with muscle weakness and balance issues.
Pain is typically related to activity and resolves with rest. In those patients in whom the disease progresses, pain is more continuous and begins to affect activities of daily living, eventually causing severe limitations in function. Patients may also experience bony swelling, joint deformity, and instability (patients complain that the joint is “giving way” or “buckling,” a sign of muscle weakness).
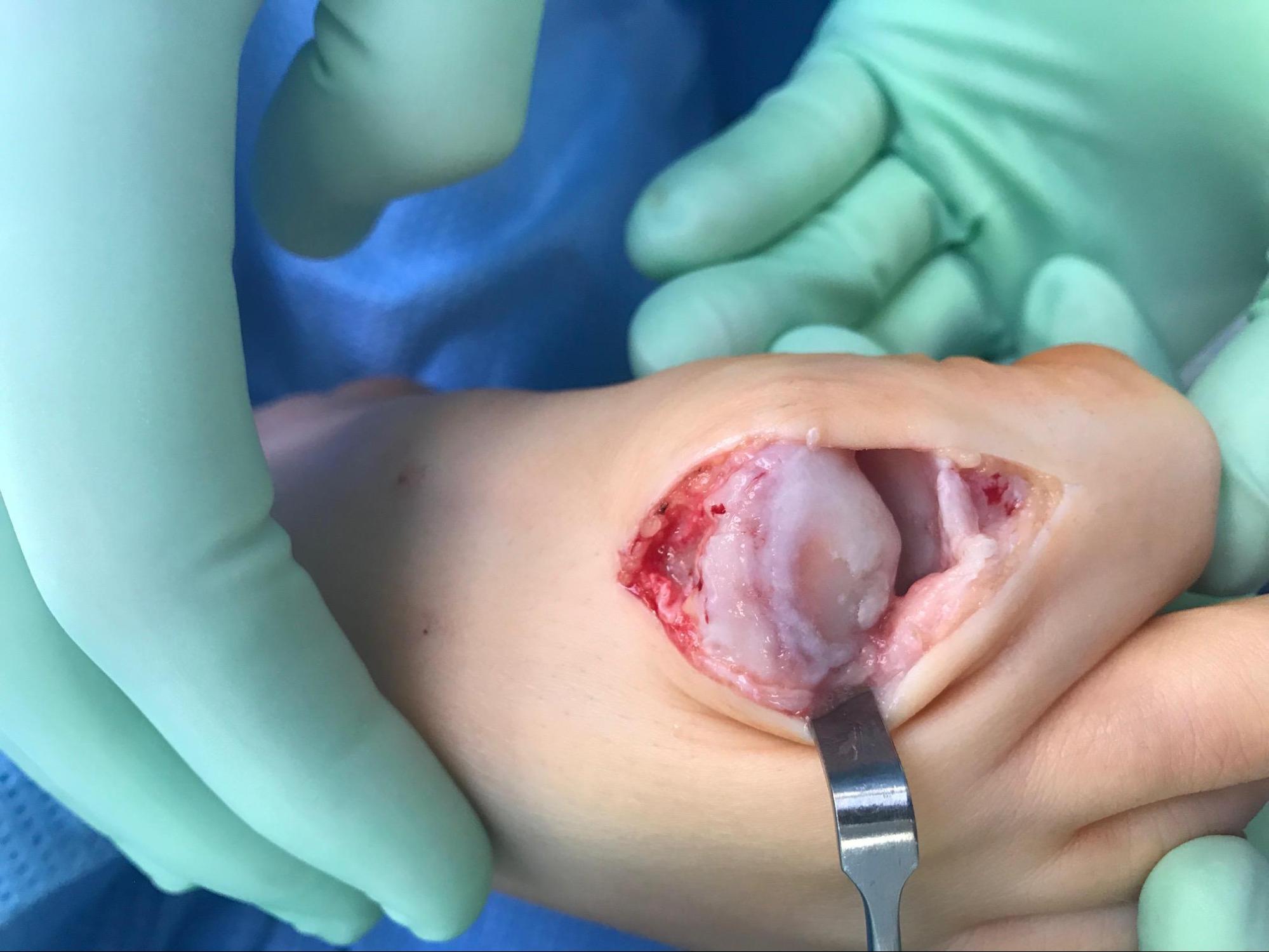
OA typically affects proximal and distal interphalangeal joints, first carpometacarpal (CMC) joints, hips, knees, first metatarsophalangeal joints, and joints of the lower cervical and lumbar spine. OA can be monoarticular or polyarticular in the presentation. Joints can be at different stages of disease progression. Typical exam findings in OA include bony enlargement, crepitus, effusions (non-inflammatory), and a limited range of motions. Tenderness may be present at joint lines, and there may be pain upon passive motion. Classic physical exam findings in hand OA include Heberden’s nodes (posterolateral swellings of DIP joints), Bouchard’s nodes (posterolateral swellings of PIP joints), and “squaring” at the base of the thumb (first CMC joints). See Image. Osteoarthritis, Hand.
Evaluation
A thorough history and physical exam (with a focused musculoskeletal exam) should be performed on all patients, with some findings summarized above. OA is a clinical diagnosis and can be diagnosed with confidence if the following are present: 1) pain worse with activity and better with rest, 2) age more than 45 years, 3) morning stiffness lasting less than 30 minutes, 4) bony joint enlargement, and 5) limitation in range of motion. A differential diagnosis should include rheumatoid arthritis, psoriatic arthritis, crystalline arthritis, hemochromatosis, bursitis, avascular necrosis, tendinitis, radiculopathy, among other soft tissue abnormalities.[9][10]
Blood tests such as CBC, ESR, rheumatoid factor, ANA are usually normal in OA, although they may be ordered to rule out inflammatory arthritis. If the synovial fluid is obtained, the white blood cell count should be less than 2000/microL, predominantly mononuclear cells (non-inflammatory), which is consistent with a diagnosis of OA.
X-rays of the affected joint can show findings consistent with OA, such as marginal osteophytes, joint space narrowing, subchondral sclerosis, and cysts; however, radiographic findings do not correlate to the severity of disease and may not be present early in the disease. MRI is not routinely indicated for OA workup; however, it can detect OA at earlier stages than normal radiographs. Ultrasound can also identify synovial inflammation, effusion, and osteophytes which can be related to OA.
There are several classification systems for OA. In general, they include the effects on joints, the age of onset, radiographic appearance, presumed etiology (primary vs. secondary), and rate of progression. The American College of Rheumatology classification is the most widely used classification system. At this time, it is not possible to predict which patients will progress to severe OA and which patients will have their disease arrest at earlier stages.
Treatment / Management
Treatment goals for OA are to minimize both pain and functional loss. Comprehensive management of the disease involves both non-pharmacologic and pharmacologic therapies. Typically, patients with mild symptoms can be managed by the former, while more advanced diseases need a combination of both.[11][12][13](A1)
Mainstays for non-pharmacologic therapy include 1) avoidance of activities exacerbating pain or overloading the joint, 2) exercise to improve strength, 3) weight loss, and 4) occupational therapy for unloading joints via brace, splint, cane, or crutch. Weight loss is a critical intervention in those who are overweight and obese; each pound of weight loss can decrease the load across the knee 3 to 6-fold. Formal physical therapy can immensely assist patients in using equipment such as canes appropriately while also instructing them on exercises. Exercise programs that combine both aerobic and resistance training have been shown to decrease pain and improve physical function in multiple trials and should be encouraged by physicians regularly. Malalignment of joints should be corrected via mechanical means such as realignment knee brace or orthotics.
Pharmacotherapy of OA involves oral, topical, and/or intraarticular options. Acetaminophen and oral NSAIDs are the most popular and affordable options for OA and are usually the initial choice of pharmacologic treatment. NSAIDs are usually prescribed orally or topically and, initially, should be started as needed rather than scheduled. Due to gastrointestinal toxicity, and renal and cardiovascular side effects, oral NSAIDs should be used very cautiously with close monitoring long term. Topical NSAIDs are less efficacious than their oral counterparts but offer fewer gastrointestinal and other systemic side effects; however, they often cause local skin irritation.
Intraarticular joint injections can also be an effective treatment for OA, especially in a setting of acute pain. Glucocorticoid injections have a variable response, and there is ongoing controversy regarding repeated injections. Hyaluronic acid injections are another option, but their efficacy over placebo is also controversial. Notably, there is no role for oral glucocorticoids.
Duloxetine has modest efficacy in OA; opioids can be used in those patients without an adequate response to the above and who may not be candidates for surgery or refuse it altogether.
It is important to note that patients vary greatly in their response to treatment, and there is a large component of trial and error in selecting the agents that will be most effective. In those patients specifically with knee or hip OA who have failed multiple non-pharmacologic and pharmacologic treatment modalities, surgery is the next option. Failure rates for both knee and hip replacements are quite low, and they can provide pain relief and increased functionality. The timing of surgery is key to predict success. Very poor functional status and considerable muscle weakness may not lead to improved postoperative functional status versus those undergoing surgery earlier in the disease course.[14][15](A1)
Differential Diagnosis
Differentials include:
- Rheumatoid arthritis
- Psoriatic arthritis
- Crystalline arthritis
- Bursitis
- Tendinitis
- Hemochromatosis
- Avascular necrosis
- Radiculopathy
- Other soft-tissue conditions
Prognosis
The prognosis for osteoarthritis patients depends on which joints are affected and the level of symptomatology and functional impairment. Some patients remain relatively unaffected by osteoarthritis, while others can experience severe disability. In some cases, joint replacement surgery offers the best long-term outcome.
Complications
- Pain
- Falls
- Difficulty ambulation
- Joint malalignment
- Decreased range of motion of the joint
- Radiculopathies
Postoperative and Rehabilitation Care
Lifestyle changes - especially enrollment in exercise and weight reduction.
Deterrence and Patient Education
The clinical team needs to explain the etiology and pathophysiology of the arthritic process and outline the plan for intervention, which will vary significantly based on the degree of pathology, joints affected, level of dysfunction, age of the patient, expectations for future activities, and what is therapeutically possibly. Compliance with medication, weight loss, and exercise/physical therapy routines must be stressed.
Enhancing Healthcare Team Outcomes
Osteoarthritis is a chronic progressive disorder that affects millions of people with advancing age. The condition has no cure and is managed by a team of healthcare professionals that include an internist, radiologist, endocrinologist, orthopedic surgeon, and rheumatologist. The nurse, pharmacist, and physical therapist are also integral members of the interprofessional healthcare team. Only through cohesive activity and communication involving all healthcare disciplines are optimal results achievable. [Level 5]
Patients with osteoarthritis require education on the natural history of the disease and understand their treatment options. Obese patients need a dietary consult and enroll in an exercise program. Evidence shows that water-based activities can help relieve symptoms and improve joint function; hence consultation with a physical therapist is recommended. Further, many of these patients may benefit from a walking aid. Patients with pain should become familiar with the types of drugs and supplements available and their potential adverse effects. Only through the education of the patient can the morbidity of this disorder be decreased.[16][17][18] [Level 5]
Evidence-Based Outcomes
The prognosis for osteoarthritis patients depends on the joint involved, how many joints are involved, and the severity. There is no cure for osteoarthritis, and all the currently available treatments are directed towards reducing symptoms. Factors associated with the rapid progression of the disease include obesity, advanced age, multiple joint involvement, and the presence of varus deformity. Patients who undergo joint replacement tend to have a good prognosis with success rates of over 80%. However, most prosthetic joints wear out in 10 to 15 years, and repeat surgery is required. Also important is that patients must undergo preoperative workup as the post-surgical complications can be serious and disabling.[19][20][21] [Level 5]
Media
(Click Image to Enlarge)
References
Bortoluzzi A, Furini F, Scirè CA. Osteoarthritis and its management - Epidemiology, nutritional aspects and environmental factors. Autoimmunity reviews. 2018 Nov:17(11):1097-1104. doi: 10.1016/j.autrev.2018.06.002. Epub 2018 Sep 11 [PubMed PMID: 30213694]
Miller A, Lutsky KF, Shearin J, Cantlon M, Wolfe S, Beredjiklian PK. Radiographic Patterns of Radiocarpal and Midcarpal Arthritis. Journal of the American Academy of Orthopaedic Surgeons. Global research & reviews. 2017 Jun:1(3):e017. doi: 10.5435/JAAOSGlobal-D-17-00017. Epub 2017 Jun 15 [PubMed PMID: 30211351]
Berenbaum F, Wallace IJ, Lieberman DE, Felson DT. Modern-day environmental factors in the pathogenesis of osteoarthritis. Nature reviews. Rheumatology. 2018 Nov:14(11):674-681. doi: 10.1038/s41584-018-0073-x. Epub [PubMed PMID: 30209413]
Donahue SW. Krogh's principle for musculoskeletal physiology and pathology. Journal of musculoskeletal & neuronal interactions. 2018 Sep 1:18(3):284-291 [PubMed PMID: 30179205]
Krishnan Y,Grodzinsky AJ, Cartilage diseases. Matrix biology : journal of the International Society for Matrix Biology. 2018 May 24 [PubMed PMID: 29803938]
Stewart HL, Kawcak CE. The Importance of Subchondral Bone in the Pathophysiology of Osteoarthritis. Frontiers in veterinary science. 2018:5():178. doi: 10.3389/fvets.2018.00178. Epub 2018 Aug 28 [PubMed PMID: 30211173]
Loef M, Schoones JW, Kloppenburg M, Ioan-Facsinay A. Fatty acids and osteoarthritis: different types, different effects. Joint bone spine. 2019 Jul:86(4):451-458. doi: 10.1016/j.jbspin.2018.07.005. Epub 2018 Aug 3 [PubMed PMID: 30081198]
Dobson GP, Letson HL, Grant A, McEwen P, Hazratwala K, Wilkinson M, Morris JL. Defining the osteoarthritis patient: back to the future. Osteoarthritis and cartilage. 2018 Aug:26(8):1003-1007. doi: 10.1016/j.joca.2018.04.018. Epub 2018 May 25 [PubMed PMID: 29775734]
De Laroche R,Simon E,Suignard N,Williams T,Henry MP,Robin P,Abgral R,Bourhis D,Salaun PY,Dubrana F,Querellou S, Clinical interest of quantitative bone SPECT-CT in the preoperative assessment of knee osteoarthritis. Medicine. 2018 Aug [PubMed PMID: 30170388]
Ackerman IN, Cavka B, Lippa J, Bucknill A. The feasibility of implementing the ICHOM Standard Set for Hip and Knee Osteoarthritis: a mixed-methods evaluation in public and private hospital settings. Journal of patient-reported outcomes. 2017:2():32. doi: 10.1186/s41687-018-0062-5. Epub 2018 Aug 1 [PubMed PMID: 30148249]
Level 2 (mid-level) evidenceKriz J, Seegenschmiedt HM, Bartels A, Micke O, Muecke R, Schaefer U, Haverkamp U, Eich HT. Updated strategies in the treatment of benign diseases-a patterns of care study of the german cooperative group on benign diseases. Advances in radiation oncology. 2018 Jul-Sep:3(3):240-244. doi: 10.1016/j.adro.2018.02.008. Epub 2018 Feb 26 [PubMed PMID: 30197936]
Level 3 (low-level) evidencedi Laura Frattura G, Filardo G, Giunchi D, Fusco A, Zaffagnini S, Candrian C. Risk of falls in patients with knee osteoarthritis undergoing total knee arthroplasty: A systematic review and best evidence synthesis. Journal of orthopaedics. 2018 Sep:15(3):903-908. doi: 10.1016/j.jor.2018.08.026. Epub 2018 Aug 24 [PubMed PMID: 30174378]
Level 1 (high-level) evidenceXing D,Wang Q,Yang Z,Hou Y,Zhang W,Chen Y,Lin J, Evidence-based guidelines for intra-articular injection in knee osteoarthritis: Formulating and evaluating research questions. International journal of rheumatic diseases. 2018 Aug [PubMed PMID: 30146747]
Level 1 (high-level) evidenceHealey EL, Afolabi EK, Lewis M, Edwards JJ, Jordan KP, Finney A, Jinks C, Hay EM, Dziedzic KS. Uptake of the NICE osteoarthritis guidelines in primary care: a survey of older adults with joint pain. BMC musculoskeletal disorders. 2018 Aug 17:19(1):295. doi: 10.1186/s12891-018-2196-2. Epub 2018 Aug 17 [PubMed PMID: 30115048]
Level 3 (low-level) evidenceO'Brien J, Hamilton K, Williams A, Fell J, Mulford J, Cheney M, Wu S, Bird ML. Improving physical activity, pain and function in patients waiting for hip and knee arthroplasty by combining targeted exercise training with behaviour change counselling: study protocol for a randomised controlled trial. Trials. 2018 Aug 7:19(1):425. doi: 10.1186/s13063-018-2808-z. Epub 2018 Aug 7 [PubMed PMID: 30086780]
Level 1 (high-level) evidenceQuinn RH, Murray J, Pezold R, Hall Q. Management of Osteoarthritis of the Hip. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Oct 15:26(20):e434-e436. doi: 10.5435/JAAOS-D-18-00351. Epub [PubMed PMID: 30134309]
Brosseau L,Thevenot O,MacKiddie O,Taki J,Wells GA,Guitard P,Léonard G,Paquet N,Aydin SZ,Toupin-April K,Cavallo S,Moe RH,Shaikh K,Gifford W,Loew L,De Angelis G,Shallwani SM,Aburub AS,Mizusaki Imoto A,Rahman P,Álvarez Gallardo IC,Cosic MB,Østerås N,Lue S,Hamasaki T,Gaudreault N,Towheed TE,Koppikar S,Kjeken I,Mahendira D,Kenny GP,Paterson G,Westby M,Laferrière L,Longchamp G, The Ottawa Panel guidelines on programmes involving therapeutic exercise for the management of hand osteoarthritis. Clinical rehabilitation. 2018 Jun 1 [PubMed PMID: 29911409]
Gwynne-Jones DP, Gray AR, Hutton LR, Stout KM, Abbott JH. Outcomes and Factors Influencing Response to an Individualized Multidisciplinary Chronic Disease Management Program for Hip and Knee Osteoarthritis. The Journal of arthroplasty. 2018 Sep:33(9):2780-2786. doi: 10.1016/j.arth.2018.04.011. Epub 2018 Apr 16 [PubMed PMID: 29739632]
Kuijpers MFL, Hannink G, van Steenbergen LN, Schreurs BW. Total Hip Arthroplasty in Young Patients in The Netherlands: Trend Analysis of }19,000 Primary Hip Replacements in the Dutch Arthroplasty Register. The Journal of arthroplasty. 2018 Dec:33(12):3704-3711. doi: 10.1016/j.arth.2018.08.020. Epub 2018 Aug 22 [PubMed PMID: 30217401]
Loures FB, Correia W, Reis JH, Pires E Albuquerque RS, de Paula Mozela A, de Souza EB, Maia PV, Barretto JM. Outcomes after knee arthroplasty in extra-articular deformity. International orthopaedics. 2019 Sep:43(9):2065-2070. doi: 10.1007/s00264-018-4147-9. Epub 2018 Sep 14 [PubMed PMID: 30215100]
Tashjian RZ,Chalmers PN, Future Frontiers in Shoulder Arthroplasty and the Management of Shoulder Osteoarthritis. Clinics in sports medicine. 2018 Oct [PubMed PMID: 30201174]