Introduction
Osteoarthritis (OA) is the most common type of arthritis in clinical practice and is one of the leading causes of disability worldwide. The presence of radiographic evidence of OA occurs in most people by age 65 and is found in about 80% of those over age 75. OA can range from an asymptomatic condition to debilitating oligo or polyarthritis. Mechanical pain is the most common presenting symptom of this disease. The hands, knees, and hips are the most commonly affected joints, although any joint can be affected.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of primary osteoarthritis is poorly understood and involves both genetic and environmental factors. Epigenetics was found to contribute to the development of OA by 30% to 65%. Age is the strongest risk factor for OA and is believed to be linked to a decreased adaptability of the joint to resist biomechanical injury, sarcopenia, and increased bone turnover. Female gender is associated with a higher prevalence of OA due to gender differences in joint alignment, ligament strength, pregnancy, and bone density. Menopause, in particular, is associated with an increased risk of OA, suggesting a role of estrogen in OA development and pain sensitization. Anatomical factors, including joint malalignment or congenital deformities, can lead to biomechanical injury, increasing the susceptibility of developing OA. Modifiable environmental factors play a major role in the development of OA. This includes occupations requiring repetitive movements and obesity, metabolic syndrome, smoking, vitamin D deficiency, muscle weakness, and low bone density.[2][3][4][5]
Epidemiology
Osteoarthritis most commonly involves the hands, knees, feet, facet joints of the spine and hips, with the knee being the most common location. The Global Burden of Diseases, Injuries, and Risk Factors Study 2017 (GBD 2017) estimated the global prevalence of knee osteoarthritis to be 263 million, with an incidence of 13 million per year. Women are at higher risk of developing primary OA than men and suffering from more severe disease. In particular, postmenopausal women are affected by the involvement of the hands, feet, and knees.[1][6]
Pathophysiology
The pathogenesis of osteoarthritis is multifactorial and interrelated. There are three major processes, including mechanical wear-and-tear, structural degeneration, and joint inflammation. The main process is believed to be due to the overuse of the joint and aging, although increased levels of several cytokines and chemokines in the affected joints' synovium suggest an inflammatory process is also present. Matrix metalloproteinases are activated and cause degradation of the cartilage extracellular matrix. The stress to cartilage promotes chondrocyte proliferation and activation, leading to the production of matrix-degrading enzymes. Later in the disease, chondrocytes undergo apoptosis, and the number of cells decreases overall.
On the anatomic level, OA's earliest process is articular cartilage damage, including surface fibrillation, irregularity, and focal erosions. Cartilage damage causes chondrocyte proliferation, and outgrowths can ossify and form osteophytes or bone spurs.
Subchondral bone sclerosis and bone cyst formation occur later in the disease and may increase joint stiffness and pain. Advanced disease results in episodic synovitis. Although rare, bony erosions may occur in erosive OA.[7][8]
Histopathology
In a healthy synovial joint, bone ends are linked by an elastic layer of articular hyaline cartilage. This layer mainly consists of water, type II collagen that maintains the structure, and proteoglycans that provide the cartilage with the ability to withstand compressive and shear forces.
Early in osteoarthritis, loss of proteoglycans disrupts the cartilage fibers, leads to the softening of cartilage, and increases the water content. The earliest sign of cartilage damage observed by light microscopy is chondral fibrillation, followed by cracks and deeper fissures. Cartilage loss promotes chondrocyte proliferation and activation. Fibroblasts in, a type I collagen matrix fills the areas that have lost cartilage and are called a “pannus.” The remodeled matrix can then become calcified and invaded by small vessels later in the disease.
In end-stage disease, the subchondral bone becomes thicker and sclerotic. The margins of the articular bone form outgrowths called “bone spurs” or “osteophytes.” Bone cysts may appear connected to the subchondral surface by a fissure filled with inflammatory fluid, myxoid material, or bone fragments.[8][7]
History and Physical
Classically, osteoarthritis presents with joint pain that is worse with use and improves with rest. The pain usually peaks in the late afternoon or early evening and can also be evident in the early morning upon awakening from sleep. The pain can be divided into two types.
- Dull, aching, throbbing pain that becomes more constant over time and is predictable. It can also be accompanied by stiffness after prolonged immobilization (also known as "gelling phenomenon").
- Intense, unpredictable pain for short periods can be emotionally traumatizing and limit the patient's readiness to participate in daily activities.
Based on the aforementioned types of pain, OA can be clinically classified into three stages:
- Early OA: Predictable sharp pain that is often triggered by a mechanical stimulus that limits the patient's ability to participate in high impact activities.
- Mid OA: In addition to the pain described above, there is unpredictable joint pain or locking – particularly for the knee. The pain becomes increasingly more constant and can affect daily activities.
- Advanced OA: Constant dull-aching pain with intermittent short episodes of unpredictable intense pain that results in avoidance of engaging in recreational or social activities.
Additional joint symptoms include tenderness, stiffness, crepitus, limited range of movement, joint swelling, deformity, or instability.
Findings on physical examination in OA include bony enlargement (most commonly affecting the DIP and PIP joints of the fingers and toes), crepitus, effusions (non-inflammatory), joint line tenderness, and limited range of motion due to pain, swelling, or joint deformity. Heberden's nodes describe the posterolateral bony swelling of the DIP joints, and Bouchard nodes describe the posterolateral bony swelling of the PIP joints. OA involving the base of the thumb (first CMC joint) is often described as a "shoulder appearance" or "squaring".[9][10][11]
Evaluation
No laboratory test can diagnose osteoarthritis, as the diagnosis is clinically based. Imaging can aid in the diagnosis of OA and can be used to exclude other types of arthritis. Inflammatory markers, including the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are usually normal in OA but may be useful in ruling out other conditions when the diagnosis is uncertain. Additional laboratory testing can be employed to exclude inflammatory conditions such as rheumatoid arthritis, which may include a rheumatoid factor (RF) and anti-cyclic citrullinated peptide (CCP) antibodies. Genetic testing looking into aberrations in collagen formation and other collagen matrix proteins, which lead to premature OA, are currently employed by research facilities. Many other biomarkers are being investigated as novel techniques to diagnose early OA, monitor disease progression, and/or respond to interventions. More data is needed, however, to validate these methods.
A variety of imaging modalities are available to confirm the diagnosis and evaluate the severity of the OA. The most commonly used modality in clinical practice is plain radiography. The European League Against Rheumatism (EULAR) recommends plain radiography as the gold standard for the initial assessment of knee or hand OA. Findings consistent with OA in plain radiography include joint space narrowing, subchondral sclerosis, subchondral cysts, and osteophyte formation. Subchondral erosions and ankylosis can be seen in radiographic films of erosive hand OA. MRI may be helpful in patients with an uncertain diagnosis to evaluate surrounding joint structures. Ultrasound is an accessible and fast imaging modality that can be used to assess inflammatory changes, including osteophytes and joint effusions, with more specificity to the peripheral joints.[12][13][14][15]
Treatment / Management
Management Overview
Management of osteoarthritis is based on the severity and distribution of the disease. Non-medical interventions, including physical therapy and weight loss, are strongly effective and should be initially attempted. Bracing, splinting, using a cane, and other assistive devices are additional non-medical treatments that should be considered when appropriate. Oral or topical NSAIDs are first-line therapies if pharmacological options are being considered. Oral NSAIDs should be avoided in patients who have a history of coronary artery disease or stroke. They should also be limited in patients with an increased risk of developing gastrointestinal complications, including those with a history of peptic ulcer disease, the elderly, or those using corticosteroids. Intra-articular corticosteroid injections should be used sparingly as well. Repeated injections have been shown to accelerate joint damage. SNRIs (Duloxetine), muscle relaxants, glucosamine and chondroitin sulfate, visco-supplementation injections, and opioids are other measures available as treatment options for OA. Various treatment interventions were evaluated and found to be ineffective in pain relief, including acetaminophen and topical capsaicin. There are relatively new treatments that have not yet been proven effective, including platelet-rich plasma, stem cell treatments, and cannabinoids. Tricyclic antidepressants have also been tried to help control pain. Significant advances in evaluating the biochemistry of cartilage, nerve transmission, and inflammatory cytokines are also pointing to newer treatments. Further research is needed to evaluate the efficacy and safety of these agents.[16][17][18][19](A1)
Primary Knee and Hip Osteoarthritis
The initial management of primary knee and hip osteoarthritis follows the general guidelines outlined above. Weight loss should be attempted in any patient with BMI is greater than 25kg/m2. At any point in the disease, a trial of exercise focusing on muscle strengthening and improving range of motion using low impact modalities should be attempted. These exercises can be either land-based or aquatic. Adjunctive measures can also include ice or heat, therapeutic ultrasound, electrical stimulation (such as transcutaneous electrical nerve stimulation [TENS], or neuromuscular electrical stimulation [NMES]).
Although not completely understood, glucosamine and chondroitin sulfate supplementation can help reduce the pain in patients with knee OA. No significant reduction in pain or function was reported with the use of vitamin D supplementation.[20](A1)
If a pharmacological option is being considered, the lowest effective dose of NSAIDs should be used. Topical diclofenac was found to be superior to oral NSAIDs in reducing pain in clinical trials. Acetaminophen was found to lack significant pain reduction in knee osteoarthritis, presumed to be due to the lack of anti-inflammatory effects. Tramadol is a weak opioid and is another pharmacological option. Tramadol alone or combined with acetaminophen has limited benefit in relieving chronic pain in OA compared to placebo.[21][22][23](A1)
Intra-articular corticosteroid injections can also be considered in moderate to severe pain despite the use of oral analgesics. It can provide immediate pain relief that can last for 12-week. Long term efficacy has not been proven, and frequent injections should be avoided due to the possible risk of promoting further cartilage damage.[23][24][25](A1)
Intra-articular hyaluronic acid injections have conflicting and limited evidence demonstrating small benefits in reducing pain and improving knee OA function. These injections remain a treatment option, however, with rare side effects.[25] Compared to platelet-rich plasma (PRP) injections, treatment with PRP was found to be superior to intraarticular hyaluronic acid injections. It can reduce pain and improve function in patients with knee OA without an increased risk of adverse events.[26][27][28](A1)
Partial or total knee replacement is reserved for patients who fail both pharmacological and non-pharmacological treatment modalities. Less invasive joint-preserving surgical interventions such as joint resurfacing, unicompartmental knee arthroplasty, or hip osteotomy should be considered in younger patients with the limited disease who remain symptomatic despite conservative management. Arthroscopic debridement was found to be ineffective and can accelerate OA.[29](A1)
Primary Hand Osteoarthritis
Non-pharmacological treatment options in primary hand osteoarthritis include the local application of heat or cold, splinting, physical and occupational therapy to improve range of motion and muscle strength. Topical or oral NSAIDs are first-line pharmacological therapy in hand OA. Intraarticular corticosteroid injections are not recommended but are occasionally used for flares. Surgery is often reserved for severe erosive disease with loss of function and persistent pain.[30][31][32](A1)
Differential Diagnosis
- Rheumatoid arthritis
- Gout
- Pseudogout
- Septic arthritis
- Hemochromatosis
- Fibromyalgia
- Lyme disease
- Ankylosing spondylitis
- Psoriatic arthritis
- Parvovirus-associated arthritis
- Neuropathic arthropathy
Prognosis
Clinically symptomatic osteoarthritis progresses slowly over time but can accelerate with trauma or overuse. Radiographic progression is also usually slowly progressive. High-quality data are lacking to support which findings indicate a poor prognostic value. It is generally understood that certain presentations are linked with a less favorable prognosis, including severe pain, muscle weakness, high BMI, worsening radiographic findings, depression, and widespread disease. A high BMI and intensive physical activity at work predict knee replacement surgery in the future.[33]
Complications
- Chronic pain
- Long term analgesics use
- Reduced joint mobility
- Decreased stability and increased fall risk
- Joint malalignment
- Deformity
- Stress fractures
- Hemarthrosis
- Osteonecrosis
- Joint infection
- Gout and Pseudogout flares
- Depression
Deterrence and Patient Education
Patients with osteoarthritis or who are at risk for developing osteoarthritis should be educated on lifestyle modifications to reduce the risk of disease progression or development. Patient education should focus on weight loss and moderate daily exercise to improve mobility and stability. Patients should be advised to avoid overuse of pain medication and watch for unfavorable side effects from their medication's prolonged use. Available assistive devices, including canes and splints, should be offered to patients if clinically indicated.
Enhancing Healthcare Team Outcomes
Many patients with osteoarthritis suffer from chronic pain and difficulty performing daily activities; hence, an interprofessional approach is necessary to improve this large cohort of patients' quality of life. Primary care physicians (internists or family physicians), orthopedic surgeons, rheumatologists, specialty trained nurses, and physical therapists share the responsibility to the care of these patients. Most importantly, patients should be counseled and educated about the prognosis and natural history of the disease. Patients should be encouraged to implement lifestyle modifications and control modifiable risk factors to hinder the disease's progression. Referring patients to physiotherapy, orthotics, occupational therapy, or dietitian services is recommended if clinically indicated.[34][35] [Level 5]
Referral to the orthopedic surgeon should not be delayed in patients who fail to respond adequately to pharmacological management. Joint replacement surgeries have high success rates and can effectively alleviate pain and improve joint alignment lasting 10 to 15 years.[36][37] [Level 5]
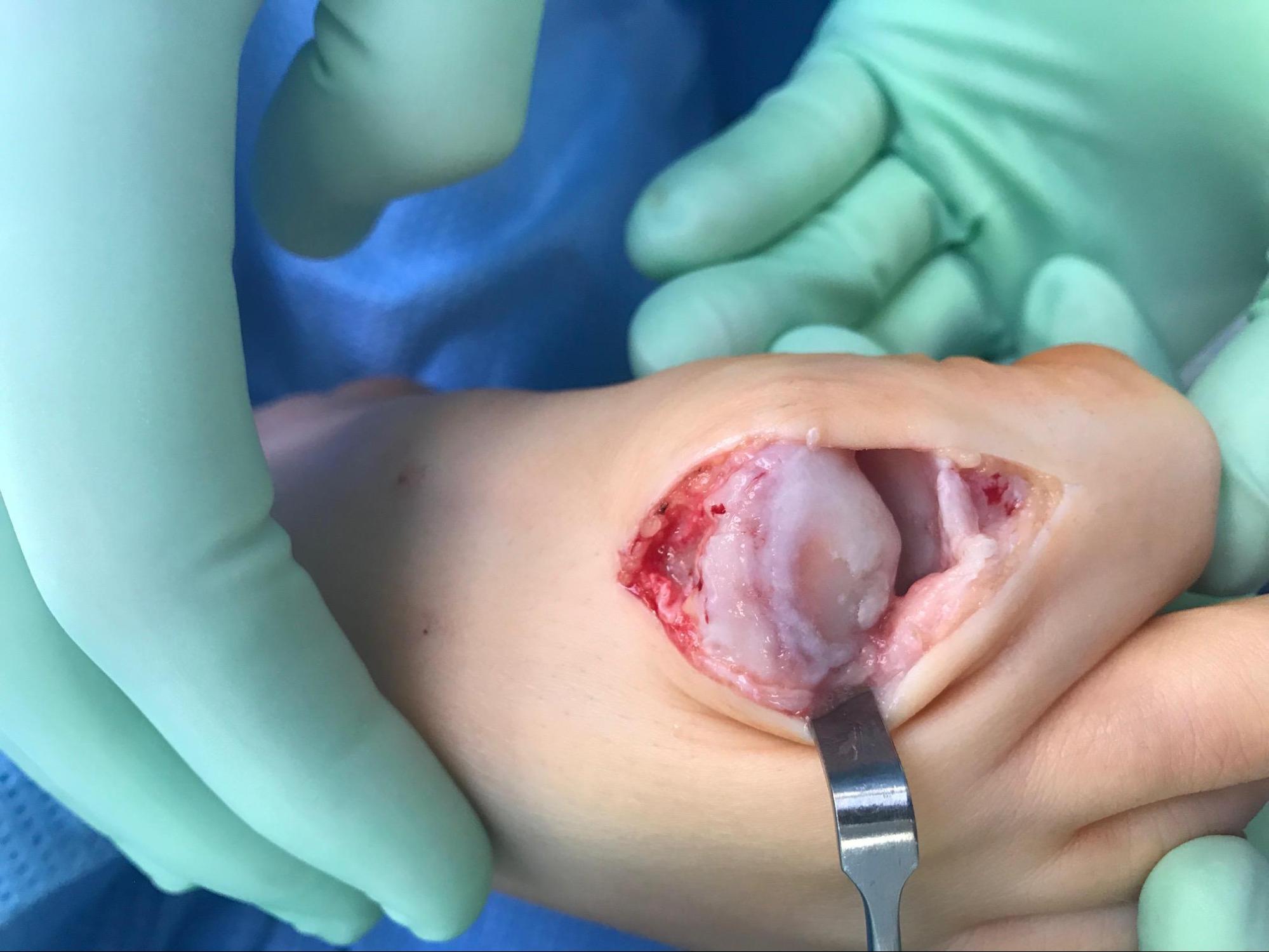
Media
(Click Image to Enlarge)
References
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018 Nov 10:392(10159):1789-1858. doi: 10.1016/S0140-6736(18)32279-7. Epub 2018 Nov 8 [PubMed PMID: 30496104]
Level 1 (high-level) evidenceVina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Current opinion in rheumatology. 2018 Mar:30(2):160-167. doi: 10.1097/BOR.0000000000000479. Epub [PubMed PMID: 29227353]
Level 3 (low-level) evidenceRego-Pérez I, Durán-Sotuela A, Ramos-Louro P, Blanco FJ. Mitochondrial Genetics and Epigenetics in Osteoarthritis. Frontiers in genetics. 2019:10():1335. doi: 10.3389/fgene.2019.01335. Epub 2020 Jan 17 [PubMed PMID: 32010192]
Yip C, Badley EM, Canizares M, Power JD, Perruccio AV. Risk Factor Profiles for Individuals With Diagnosed OA and With Symptoms Indicative of OA: Findings From the Canadian Longitudinal Study on Aging. ACR open rheumatology. 2020 Mar:2(3):174-179. doi: 10.1002/acr2.11120. Epub 2020 Mar 1 [PubMed PMID: 32114717]
Allen KD, Golightly YM. State of the evidence. Current opinion in rheumatology. 2015 May:27(3):276-83. doi: 10.1097/BOR.0000000000000161. Epub [PubMed PMID: 25775186]
Level 3 (low-level) evidenceJohnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best practice & research. Clinical rheumatology. 2014 Feb:28(1):5-15. doi: 10.1016/j.berh.2014.01.004. Epub [PubMed PMID: 24792942]
Khlopas H, Khlopas A, Samuel LT, Ohliger E, Sultan AA, Chughtai M, Mont MA. Current Concepts in Osteoarthritis of the Ankle: Review. Surgical technology international. 2019 Nov 10:35():280-294 [PubMed PMID: 31237341]
Sulzbacher I. Osteoarthritis: histology and pathogenesis. Wiener medizinische Wochenschrift (1946). 2013 May:163(9-10):212-9. doi: 10.1007/s10354-012-0168-y. Epub 2012 Dec 20 [PubMed PMID: 23263638]
Hawker GA, Stewart L, French MR, Cibere J, Jordan JM, March L, Suarez-Almazor M, Gooberman-Hill R. Understanding the pain experience in hip and knee osteoarthritis--an OARSI/OMERACT initiative. Osteoarthritis and cartilage. 2008 Apr:16(4):415-22. doi: 10.1016/j.joca.2007.12.017. Epub 2008 Mar 4 [PubMed PMID: 18296075]
Level 3 (low-level) evidenceAllen KD, Coffman CJ, Golightly YM, Stechuchak KM, Keefe FJ. Daily pain variations among patients with hand, hip, and knee osteoarthritis. Osteoarthritis and cartilage. 2009 Oct:17(10):1275-82. doi: 10.1016/j.joca.2009.03.021. Epub 2009 Apr 17 [PubMed PMID: 19410670]
Peter JB, Marmor L. Osteoarthritis of the first carpometacarpal joint. California medicine. 1968 Aug:109(2):116-20 [PubMed PMID: 5673986]
Hosnijeh FS, Runhaar J, van Meurs JB, Bierma-Zeinstra SM. Biomarkers for osteoarthritis: Can they be used for risk assessment? A systematic review. Maturitas. 2015 Sep:82(1):36-49. doi: 10.1016/j.maturitas.2015.04.004. Epub 2015 Apr 14 [PubMed PMID: 25963100]
Level 1 (high-level) evidenceZhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, Bresnihan B, Herrero-Beaumont G, Kirschner S, Leeb BF, Lohmander LS, Mazières B, Pavelka K, Punzi L, So AK, Tuncer T, Watt I, Bijlsma JW. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Annals of the rheumatic diseases. 2010 Mar:69(3):483-9. doi: 10.1136/ard.2009.113100. Epub 2009 Sep 17 [PubMed PMID: 19762361]
Level 2 (mid-level) evidenceZhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, Dincer F, Dziedzic K, Hauselmann HJ, Kaklamanis P, Kloppenburg M, Lohmander LS, Maheu E, Martin-Mola E, Pavelka K, Punzi L, Reiter S, Smolen J, Verbruggen G, Watt I, Zimmermann-Gorska I, ESCISIT. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Annals of the rheumatic diseases. 2009 Jan:68(1):8-17. doi: 10.1136/ard.2007.084772. Epub 2008 Feb 4 [PubMed PMID: 18250111]
Wang X, Oo WM, Linklater JM. What is the role of imaging in the clinical diagnosis of osteoarthritis and disease management? Rheumatology (Oxford, England). 2018 May 1:57(suppl_4):iv51-iv60. doi: 10.1093/rheumatology/kex501. Epub [PubMed PMID: 29351654]
Ton J, Perry D, Thomas B, Allan GM, Lindblad AJ, McCormack J, Kolber MR, Garrison S, Moe S, Craig R, Dugré N, Chan K, Finley CR, Ting R, Korownyk CS. PEER umbrella systematic review of systematic reviews: Management of osteoarthritis in primary care. Canadian family physician Medecin de famille canadien. 2020 Mar:66(3):e89-e98 [PubMed PMID: 32165479]
Level 1 (high-level) evidenceBarrow DR, Abbate LM, Paquette MR, Driban JB, Vincent HK, Newman C, Messier SP, Ambrose KR, Shultz SP. Exercise prescription for weight management in obese adults at risk for osteoarthritis: synthesis from a systematic review. BMC musculoskeletal disorders. 2019 Dec 20:20(1):610. doi: 10.1186/s12891-019-3004-3. Epub 2019 Dec 20 [PubMed PMID: 31861990]
Level 1 (high-level) evidenceLeopoldino AO, Machado GC, Ferreira PH, Pinheiro MB, Day R, McLachlan AJ, Hunter DJ, Ferreira ML. Paracetamol versus placebo for knee and hip osteoarthritis. The Cochrane database of systematic reviews. 2019 Feb 25:2(2):CD013273. doi: 10.1002/14651858.CD013273. Epub 2019 Feb 25 [PubMed PMID: 30801133]
Level 1 (high-level) evidenceCharlesworth J, Fitzpatrick J, Perera NKP, Orchard J. Osteoarthritis- a systematic review of long-term safety implications for osteoarthritis of the knee. BMC musculoskeletal disorders. 2019 Apr 9:20(1):151. doi: 10.1186/s12891-019-2525-0. Epub 2019 Apr 9 [PubMed PMID: 30961569]
Level 1 (high-level) evidenceHussain S, Singh A, Akhtar M, Najmi AK. Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials. Rheumatology international. 2017 Sep:37(9):1489-1498. doi: 10.1007/s00296-017-3719-0. Epub 2017 Apr 18 [PubMed PMID: 28421358]
Level 1 (high-level) evidenceStewart M, Cibere J, Sayre EC, Kopec JA. Efficacy of commonly prescribed analgesics in the management of osteoarthritis: a systematic review and meta-analysis. Rheumatology international. 2018 Nov:38(11):1985-1997. doi: 10.1007/s00296-018-4132-z. Epub 2018 Aug 17 [PubMed PMID: 30120508]
Level 1 (high-level) evidenceToupin April K, Bisaillon J, Welch V, Maxwell LJ, Jüni P, Rutjes AW, Husni ME, Vincent J, El Hindi T, Wells GA, Tugwell P. Tramadol for osteoarthritis. The Cochrane database of systematic reviews. 2019 May 27:5(5):CD005522. doi: 10.1002/14651858.CD005522.pub3. Epub 2019 May 27 [PubMed PMID: 31132298]
Level 1 (high-level) evidenceJüni P, Hari R, Rutjes AW, Fischer R, Silletta MG, Reichenbach S, da Costa BR. Intra-articular corticosteroid for knee osteoarthritis. The Cochrane database of systematic reviews. 2015 Oct 22:2015(10):CD005328. doi: 10.1002/14651858.CD005328.pub3. Epub 2015 Oct 22 [PubMed PMID: 26490760]
Level 1 (high-level) evidenceZhong HM, Zhao GF, Lin T, Zhang XX, Li XY, Lin JF, Zhao SQ, Pan ZJ. Intra-Articular Steroid Injection for Patients with Hip Osteoarthritis: A Systematic Review and Meta-Analysis. BioMed research international. 2020:2020():6320154. doi: 10.1155/2020/6320154. Epub 2020 Feb 24 [PubMed PMID: 32185212]
Level 1 (high-level) evidenceXing D, Wang B, Liu Q, Ke Y, Xu Y, Li Z, Lin J. Intra-articular Hyaluronic Acid in Treating Knee Osteoarthritis: a PRISMA-Compliant Systematic Review of Overlapping Meta-analysis. Scientific reports. 2016 Sep 12:6():32790. doi: 10.1038/srep32790. Epub 2016 Sep 12 [PubMed PMID: 27616273]
Level 1 (high-level) evidenceChen Z, Wang C, You D, Zhao S, Zhu Z, Xu M. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: A meta-analysis. Medicine. 2020 Mar:99(11):e19388. doi: 10.1097/MD.0000000000019388. Epub [PubMed PMID: 32176063]
Level 1 (high-level) evidenceHohmann E, Tetsworth K, Glatt V. Is platelet-rich plasma effective for the treatment of knee osteoarthritis? A systematic review and meta-analysis of level 1 and 2 randomized controlled trials. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2020 Aug:30(6):955-967. doi: 10.1007/s00590-020-02623-4. Epub 2020 Feb 14 [PubMed PMID: 32060630]
Level 1 (high-level) evidenceZhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis and cartilage. 2008 Feb:16(2):137-62. doi: 10.1016/j.joca.2007.12.013. Epub [PubMed PMID: 18279766]
Level 1 (high-level) evidenceStoffer-Marx MA, Klinger M, Luschin S, Meriaux-Kratochvila S, Zettel-Tomenendal M, Nell-Duxneuner V, Zwerina J, Kjeken I, Hackl M, Öhlinger S, Woolf A, Redlich K, Smolen JS, Stamm TA. Functional consultation and exercises improve grip strength in osteoarthritis of the hand - a randomised controlled trial. Arthritis research & therapy. 2018 Nov 9:20(1):253. doi: 10.1186/s13075-018-1747-0. Epub 2018 Nov 9 [PubMed PMID: 30413191]
Level 1 (high-level) evidenceMarshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nature reviews. Rheumatology. 2018 Nov:14(11):641-656. doi: 10.1038/s41584-018-0095-4. Epub [PubMed PMID: 30305701]
Lue S, Koppikar S, Shaikh K, Mahendira D, Towheed TE. Systematic review of non-surgical therapies for osteoarthritis of the hand: an update. Osteoarthritis and cartilage. 2017 Sep:25(9):1379-1389. doi: 10.1016/j.joca.2017.05.016. Epub 2017 Jun 15 [PubMed PMID: 28602781]
Level 1 (high-level) evidenceApold H, Meyer HE, Nordsletten L, Furnes O, Baste V, Flugsrud GB. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC musculoskeletal disorders. 2014 Jun 23:15():217. doi: 10.1186/1471-2474-15-217. Epub 2014 Jun 23 [PubMed PMID: 24957045]
Brosseau L, Thevenot O, MacKiddie O, Taki J, Wells GA, Guitard P, Léonard G, Paquet N, Aydin SZ, Toupin-April K, Cavallo S, Moe RH, Shaikh K, Gifford W, Loew L, De Angelis G, Shallwani SM, Aburub AS, Mizusaki Imoto A, Rahman P, Álvarez Gallardo IC, Cosic MB, Østerås N, Lue S, Hamasaki T, Gaudreault N, Towheed TE, Koppikar S, Kjeken I, Mahendira D, Kenny GP, Paterson G, Westby M, Laferrière L, Longchamp G. The Ottawa Panel guidelines on programmes involving therapeutic exercise for the management of hand osteoarthritis. Clinical rehabilitation. 2018 Nov:32(11):1449-1471. doi: 10.1177/0269215518780973. Epub 2018 Jun 18 [PubMed PMID: 29911409]
Gwynne-Jones DP, Gray AR, Hutton LR, Stout KM, Abbott JH. Outcomes and Factors Influencing Response to an Individualized Multidisciplinary Chronic Disease Management Program for Hip and Knee Osteoarthritis. The Journal of arthroplasty. 2018 Sep:33(9):2780-2786. doi: 10.1016/j.arth.2018.04.011. Epub 2018 Apr 16 [PubMed PMID: 29739632]
Kuijpers MFL, Hannink G, van Steenbergen LN, Schreurs BW. Total Hip Arthroplasty in Young Patients in The Netherlands: Trend Analysis of }19,000 Primary Hip Replacements in the Dutch Arthroplasty Register. The Journal of arthroplasty. 2018 Dec:33(12):3704-3711. doi: 10.1016/j.arth.2018.08.020. Epub 2018 Aug 22 [PubMed PMID: 30217401]
Loures FB, Correia W, Reis JH, Pires E Albuquerque RS, de Paula Mozela A, de Souza EB, Maia PV, Barretto JM. Outcomes after knee arthroplasty in extra-articular deformity. International orthopaedics. 2019 Sep:43(9):2065-2070. doi: 10.1007/s00264-018-4147-9. Epub 2018 Sep 14 [PubMed PMID: 30215100]