Introduction
The true beginning of the concept of a pacemaker began over 200 years ago. In the late 1700s, Luigi Galvani discovered that he could cause contraction of a frog heart simply by passing an electrical current through the heart. This concept was further realized nearly 100 years later with the first successful resuscitation of a child by Guilliame de Boulogne utilizing electricity. He was able to accomplish this by introducing an electrical current to the patient's chest with a return electrode on the leg after a drowning. After this feat, many successful resuscitations were reported, leading to the term "artificial cardiac pacemaker" by Dr. Hyman in 1932.[1][2]
Pacemakers are adjustable artificial electrical pulse generators, frequently emitting a pulse with a duration between 0.5 and 25 milliseconds with an output of 0.1 to 15 volts, at a frequency up to 300 times per minute. The cardiologist or pacemaker technologist will be able to interrogate and control the pacing rate, the pulse width, and the voltage, whether the device is temporary or permanent. Pacemakers are typically categorized as external or internal. The external variety is almost always placed for temporary stabilization of the patient or to facilitate some type of surgical procedure. The implantable type is usually permanent and often, significantly more complex than the temporary, external variety.
Pacemakers are one type of cardiac implantable electronic devices (known as CIED). This broad category also includes implantable cardioverter-defibrillators (ICDs). Collectively, this group of devices was first introduced in the 1950s, shortly after the advent of the transistor. As technology has improved, so has the pacemaker device. The first implantable ICD was developed in 1980, and since that time, it has become more difficult to differentiate between pacemakers and ICDs. This is because every ICD currently implanted has an anti-bradycardia pacing function. It is critical for the patient and any health care provider to understand which device has been implanted to prevent unnecessary ICD therapy. This is most likely to occur with any electromagnetic interference (EMI) and could lead to activation of the device (if it is an ICD). Most types of CIED use several insulated lead wires with non-insulated tips that are implanted in the heart, either by percutaneous vein insertion or directly by a cardiac surgeon. Cardiac pacemakers are made up of two parts: the pulse generator and the leads or electrodes.
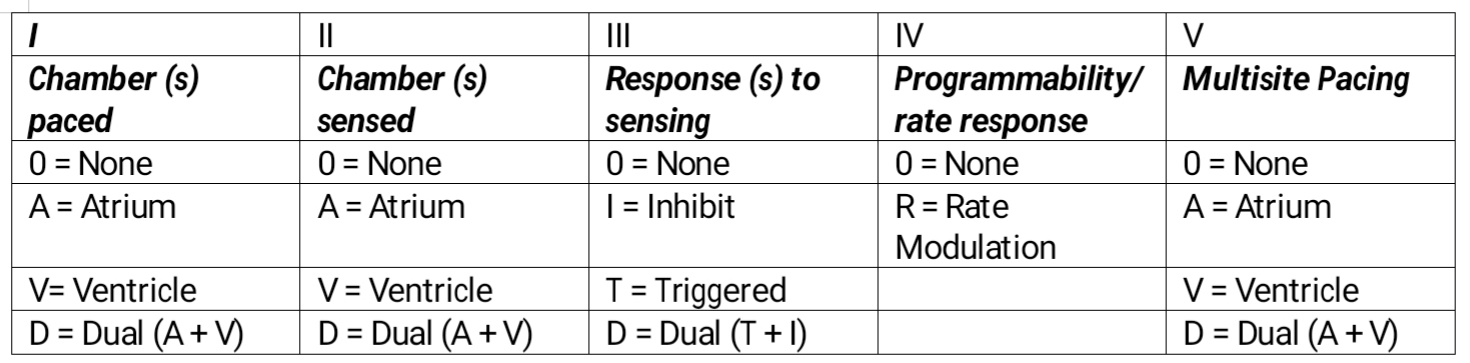
The North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG) jointly developed a generic pacemaker code, utilized worldwide, that would allow providers and manufacturers to describe the characteristics of the device. This was last updated in 2002 and is shown below in the Pacemaker Table.[3]
The first letter in the code indicated which chamber is paced; the second letter indicates which chamber is being sensed by the device; the third letter indicates if there is a response to sensing; the fourth position indicates whether the device will modulate or change the programmed rate independent of the patient's cardiac activity, for example, with exercise; the fifth and last letter of the code indicates additional multisite pacing. The last two letters of the code (in the fourth and fifth position) are rarely used in typical nomenclature.[3]
The latest generation of pacemakers have many capabilities. The simplest settings are AAI and VVI. The AAI mode paces and senses in the atrium and each sensed event triggers the generator to fire within the P wave. The VVI mode paces and senses the ventricle and is suppressed by a sensed ventricular event.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS) have jointly established national guidelines to direct the implantation of artificial cardiac pacemakers.[4][5] A detailed discussion of these guidelines is beyond the scope of this article, but an outline will be presented. The main indications for pacemaker implantation include:
- Symptomatic bradycardia from sinus node disease
- Symptomatic bradycardia from atrioventricular node disease
- Long QT syndrome
- Hypertrophic obstructive cardiomyopathy
- Dilated cardiomyopathy
- During AV node ablation
- Cardiac resynchronization therapy with biventricular pacing
- Advanced 2nd or third-degree heart block
- Recurrent syncope
Pacemakers are programmed noninvasively today. Pacemaker generators have an x-ray code which can be visualized on the chest x-ray.
Epidemiology
There is no easy method to determine the absolute number of implantable cardiac devices in the United States and the world today. Although only an estimate, various sources list the number of individuals in the United States with an implantable pacemaker anywhere between 500,000 and 3 million. The chance of pacemaker implantation increases dramatically with age. In fact, over 70% of all pacemakers are implanted in patients over the age of 65. With an aging population and increasing life expectancy, one can only expect the number of ICDs to increase in the future exponentially. Since their advent in the 1950s, over 3000 models of pacemakers have been introduced into the United States alone.
Toxicokinetics
Magnet Inhibition
When a patient with a pacemaker requires surgery or a procedure where electrocautery or related devices will be used, this can interfere with the function of the device. Thus magnet inhibition is commonly done. Placing the magnet over the pacemaker temporarily reprograms the device into an asynchronous pacing mode but does not completely switch it off. After the procedure, the cardiologist has to reprogram the device.
In most cases, almost any pacemaker can be inhibited this way. Further, there are some pacers, in which the magnet function can be disabled.
History and Physical
Patients who eventually require permanent pacemaker implantation often present with symptoms of dizziness, lightheadedness, fatigue, syncope, or lack of exercise tolerance. Frequently, these symptoms arise from bradyarrhythmias and patients will have sinus node dysfunction or atrioventricular (AV) conduction defects. A thorough history to determine if these symptoms are related to bradycardia episodes is key, as well as a physical exam. In addition, an electrocardiogram or loop recorder monitor are important steps in o order to determine if permanent pacemaker insertion is indicated.
Treatment / Management
Permanent pacemakers are most commonly placed via the transvenous route in a procedural suite or operating room. Patients are frequently sedated or under monitored anesthesia care (MAC) for the placement of these devices. For open epicardial placement by a cardiac surgeon, a patient will require general anesthesia.[6][7][8](B2)
The American Society of Anesthesiologists released a practice advisory for the perioperative management of cardiac implantable electronic devices in 2011. [9] A summary of the guidelines, which provide an outline of how to manage patients with ICDs undergoing surgical procedures, is listed below:
- Perform a focused history and physical to determine the presence of a CIED utilizing a review of medical records, chest x-rays, electrocardiograms, and palpation of the device.
- Determine the type of CIED and its function by inspecting device card, utilizing chest x-ray, and interviewing the patient. It is critical to determine if the device is a pacemaker or ICD.
- Determine if the patient is dependent on the device's pacing function.
- Determine if electromagnetic interference will occur during the surgical procedure and if so, suspend the anti-tachyarrhythmia functions by reprogramming or use of a magnet if applicable; consider placing external defibrillator pads if the device has been deactivated and placed pads as far from an implantable device as possible.
- Monitor function of the device intraoperatively; special conditions include lithotripsy, MRI, electroconvulsive therapy, and radiation therapy.
- Postoperatively, monitor rhythm and device function, obtain interrogation of the device, and restore settings as appropriate.
Differential Diagnosis
- Acute coronary syndromes
- Cardiogenic pulmonary edema
- Carotid sinus hypersensitivity
- Hyperparathyroidism and thyrotoxicosis
- Hypothyroidism
- Pacemaker malfunction
- Pacemaker mediated tachycardia
- Paroxysmal supraventricular tachycardia
- Pulmonary embolism
Complications
Complications occur during pacemaker insertion and include:
- Pneumothorax
- Wound infection
- Pericarditis
- Skin erosion
- Lead dislodgment
- Hematoma
- Failure to sense, capture or output
- Pacemaker mediated tachycardia
- Twiddler syndrome
- Pacemaker syndrome
- Pacemaker pseudomalfunction
Enhancing Healthcare Team Outcomes
Guidelines for proper follow up following pacemaker insertion are not clearly defined. there is a great variance in follow-up regarding pacemaker evaluation, battery status, and stimulation and sensing thresholds. More important, studies show that reprogramming of pacemakers is often neglected in the long run, and thus the pacemaker visit may be redundant.[10][11] (level III)
Even though nurses do not insert pacemakers, they are vital for assessing the preoperative and postoperative status of patients undergoing pacemaker insertion. Advanced practice nurses now usually assess patients in preoperative clinics and play a vital role in educating the patient and family about pacemaker care and followup. Another key feature is the management of medications by the pharmacist in patients with pacemakers. Prior to surgery, the decision to stop anticoagulation and start beta-blockers should always be made in consultation with a cardiologist. Only by stratifying risk in the preoperative period and medication reconciliation can one offer patients optimal care after pacemaker insertion.[12]
Outcomes
The short come outcomes for pacemaker insertions are good, but the long-term outcomes vary on many factors. Mortality following pacemaker insertion varies from 1-4% and complications occur in 4-15% of patients. Variables which affect mortality and complications include the presence of renal failure, high NYHA class, low ejection fraction, low platelet count, stroke and body mass index. Given the high morbidity of pacemakers, an interprofessional team of healthcare workers that closely monitors the patient and makes a timely referral may help mitigate the complications. [13] [14](Level III)
Media
(Click Image to Enlarge)
Pacemaker Table. External pacing is the fastest available method to synchronize cardiac rhythm in all the bradyarrhythmias indicated by the American Heart Association. This temporary method is used to maintain cardiac output in all those irreversible conditions where there is a need for a permanent pacemaker or those reversible situations where permanent pacing is contraindicated.
Contributed by M Ellison, MD, FASA
References
Crofoot M, Sarwar A, Weir AJ. External Pacemaker. StatPearls. 2024 Jan:(): [PubMed PMID: 30137851]
Ivanchina AE, Kopylov FY, Volkova AL, Samojlenko IV, Syrkin AL. [Clinical Value of Algorithms of Minimization of Right Ventricular Pacing in Patients With Sick Sinus Syndrome and History of Atrial Fibrillation]. Kardiologiia. 2018 Aug:(8):58-63 [PubMed PMID: 30131043]
Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B, Reynolds DW, Schoenfeld MH, Sutton R. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group. Pacing and clinical electrophysiology : PACE. 2002 Feb:25(2):260-4 [PubMed PMID: 11916002]
Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA 3rd, Ferguson TB Jr, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD, American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines, Heart Rhythm Society. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology. 2013 Jan 22:61(3):e6-75. doi: 10.1016/j.jacc.2012.11.007. Epub 2012 Dec 19 [PubMed PMID: 23265327]
Level 1 (high-level) evidence2012 Writing Group Members, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA 3rd, Ferguson TB Jr, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD, 2008 Writing Committee Members, Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, ACCF/AHA Task Force Members, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Creager MA, DeMets D, Ettinger SM, Guyton RA, Hochman JS, Kushner FG, Ohman EM, Stevenson W, Yancy CW, American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, Heart Failure Society of America, Society of Thoracic Surgeons. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. The Journal of thoracic and cardiovascular surgery. 2012 Dec:144(6):e127-45. doi: 10.1016/j.jtcvs.2012.08.032. Epub [PubMed PMID: 23140976]
Level 1 (high-level) evidenceVan Gelder IC, Rienstra M, Crijns HJ, Olshansky B. Rate control in atrial fibrillation. Lancet (London, England). 2016 Aug 20:388(10046):818-28. doi: 10.1016/S0140-6736(16)31258-2. Epub [PubMed PMID: 27560277]
Mattsson G, Magnusson P. [The leadless pacemaker system: present applications and future perspectives]. Lakartidningen. 2018 Aug 8:115():. pii: E7UM. Epub 2018 Aug 8 [PubMed PMID: 30106456]
Level 3 (low-level) evidenceTjong FVY, Beurskens NEG, Neuzil P, Defaye P, Delnoy PP, Ip J, Guerrero JJG, Rashtian M, Banker R, Reddy V, Exner D, Sperzel J, Knops RE, Leadless II IDE and, Observational Study Investigators. The learning curve associated with the implantation of the Nanostim leadless pacemaker. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2018 Nov:53(2):239-247. doi: 10.1007/s10840-018-0438-8. Epub 2018 Aug 13 [PubMed PMID: 30105428]
Level 2 (mid-level) evidenceStone ME, Salter B, Fischer A. Perioperative management of patients with cardiac implantable electronic devices. British journal of anaesthesia. 2011 Dec:107 Suppl 1():i16-26. doi: 10.1093/bja/aer354. Epub [PubMed PMID: 22156267]
Zhang S, Gaiser S, Kolominsky-Rabas PL, National Leading-Edge Cluster Medical Technologies “Medical Valley EMN”. Cardiac implant registries 2006-2016: a systematic review and summary of global experiences. BMJ open. 2018 Apr 12:8(4):e019039. doi: 10.1136/bmjopen-2017-019039. Epub 2018 Apr 12 [PubMed PMID: 29654008]
Level 1 (high-level) evidenceMagnusson P, Liv P. Living with a pacemaker: patient-reported outcome of a pacemaker system. BMC cardiovascular disorders. 2018 Jun 4:18(1):110. doi: 10.1186/s12872-018-0849-6. Epub 2018 Jun 4 [PubMed PMID: 29866050]
Thanavaro JL. Cardiac risk assessment: decreasing postoperative complications. AORN journal. 2015 Feb:101(2):201-12. doi: 10.1016/j.aorn.2014.03.014. Epub [PubMed PMID: 25645037]
Knight BP, Gersh BJ, Carlson MD, Friedman PA, McNamara RL, Strickberger SA, Tse HF, Waldo AL, American Heart Association Council on Clinical Cardiology (Subcommittee on Electrocardiography and Arrhythmias), Quality of Care and Outcomes Research Interdisciplinary Working Group, Heart Rhythm Society, AHA Writing Group. Role of permanent pacing to prevent atrial fibrillation: science advisory from the American Heart Association Council on Clinical Cardiology (Subcommittee on Electrocardiography and Arrhythmias) and the Quality of Care and Outcomes Research Interdisciplinary Working Group, in collaboration with the Heart Rhythm Society. Circulation. 2005 Jan 18:111(2):240-3 [PubMed PMID: 15657388]
Level 2 (mid-level) evidenceBodagh N, Pappa E, Farooqi F. Multidisciplinary surgical team approach for excision of squamous cell carcinoma overlying pacemaker site. BMJ case reports. 2018 Feb 6:2018():. pii: bcr-2017-221660. doi: 10.1136/bcr-2017-221660. Epub 2018 Feb 6 [PubMed PMID: 29437678]
Level 2 (mid-level) evidence