Introduction
The patella is the largest sesamoid bone in the human body.[1] The posterior aspect of the patella contains a thick cartilage layer, which is the thickest cartilage in the body. A vertical ridge separates the medial and lateral facets of the articular surface and articulates with the femoral trochlea.[2] The patella protects the anterior aspect of the knee joint, serves as the insertion for the quadriceps tendon, and functions as a fulcrum to maximize the efficiency of the extensor mechanism.[3] The inferior pole of the patella attaches to the patella tendon. The patellar retinaculum is formed by contributions from the fascia lata, vastus medialis, and vastus lateralis. The patella receives centripetal blood supply from the geniculate arteries, with the superior vessels lying anterior to the quadriceps tendon and the inferior vessels passing posterior to the patellar tendon.[4] The most important blood supply to the patella penetrates the inferior pole along the fat pad below the patella.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Fractures of the patella may be due to direct or indirect forces, and the mechanism of injury often determines the fracture pattern. The patella most commonly fails indirectly under tension. Eccentric forces from the extensor mechanism may overpower the mechanical properties of the bone.[5] Due to the patella’s subcutaneous position, a direct injury may result from a blow to the anterior knee, such as from a fall or impact from the dashboard in a motor vehicle accident.[5]
With the demand for primary total knee arthroplasty projected to grow to 3.48 million procedures performed in 2030, a 673% increase from 2005, a rise in periprosthetic patella fractures is expected to increase.[6] The combination of increased life expectancy, increased activity demands of patients, along with an increasing need for total knee arthroplasty, has led to a simultaneous increase in periprosthetic fractures. Periprosthetic fractures are complex problems and requiring a comprehensive history, thorough preoperative discussion with the patient and family members, and extensive surgical planning. Similar to native patella fractures, periprosthetic fractures are caused by direct trauma or eccentric load via the patella or quadriceps tendon.[7]
Epidemiology
Fractures of the patella account for approximately 1% of all fractures.[2] They occur more commonly in males. Open injuries account for 6% to 9% of patellar fractures and are commonly associated with other injuries given the high energy mechanism.[2][8][9] In a small percentage of the population, a secondary ossification center in the patella, most commonly at the superolateral patellar edge, may fail to fuse, resulting in a bipartite patella.[10] On radiographs, they may be mistaken for a fracture. In 50% of patients with this condition, the bipartite patella is found in both knees.[10]
Periprosthetic fractures of the patella are devastating injuries and are the most frequent complication following total knee arthroplasty.[7] The Mayo Joint registry analyzed 12,000 primary total knee arthroplasties over thirteen years and found the prevalence of periprosthetic patellar fractures to be 0.68%.[11] Postoperative periprosthetic patella fractures are more common than intraoperative fractures. Revision total knee arthroplasty with patellar component substitution has twice the rate of postoperative periprosthetic patella fracture (1.8%) and nine times the rate of intraoperative patella fracture (0.2%) compared to primary total knee arthroplasty.[12] Periprosthetic fractures are classified by timing (intraoperative or postoperative) and subclassified by displacement, adequacy of bone stock, the stability of the patella component, and competence of the extensor mechanism.
Pathophysiology
The patella experiences complex, dynamic loading patterns.[3] With the knee in extension, the pull of the quadriceps places the patella in tension. Conversely, flexing the knee places compressive forces along the posterior patella. Additionally, the patella experiences compression and 3-point bending forces exerted by the quadriceps and patellar tendons during knee flexion.[5] If rapid knee flexion occurs during active contraction of the quadriceps, the 3-force bending forces may cause the patella to fail in compression. The indirect eccentric tension through the extensor mechanism often results in avulsion fractures of the inferior pole or transverse fractures extending into the extensor retinaculum, causing fracture displacement.[5] With direct fractures of the patella, the retinaculum and extensor mechanism often remain intact despite the substantial fracture comminution and cartilage damage.[2]
Periprosthetic patellar fractures are classified on a temporal basis, intraoperative or postoperative. Postoperative periprosthetic patellar fractures are more prevalent that intraoperative fractures and have predisposing factors associated with their pathology.[13] Intraoperative periprosthetic patellar fractures may arise from; revision arthroplasty, excessive force applied to the patella clamp, overzealous reaming of the patella (<10 to 15mm of remaining bone stock), anterior perforation during preparation, and thermal necrosis from cement application.[14]
Postoperative periprosthetic patellar fractures are classified as traumatic or atraumatic. Traumatic causes are similar to those described in native patellar fractures. Atraumatic mechanism of fractures is caused by surgical technique, patient factors, and implant choice. Reuben advised against the revision to a new patellar component if <10 mm of bone stock remains and advocates for the retention of a well-positioned and minimally worn prosthesis during revision total knee arthroplasty.[15] Tria et al. reported a 3.5% incidence of a periprosthetic patella fracture in 504 primary total knee arthroplasties. Of those, 100% of the periprosthetic patellar fractures were associated with a lateral release. Lateral release endangers the superior lateral geniculate artery and may violate the major vascular supply to the patella.[16] Osteolysis and loosening of the patella prosthesis predispose the patella to fracture with the associated loss of bone stock.[17]
Contrary to intraoperative periprosthetic patellar fractures associated with aggressive reaming, postoperative stress failure of the patella is a complication associated with inadequate reaming. Overstuffing the patellofemoral joint with a patellar prosthesis larger than the bone resected or a femoral component that is too large, places abnormal stress on the patella and predispose to stress failure. Component malpositioning during the index arthroplasty has a significant role in patella tracking. Patellar maltracking places undue stress on the patella and can lead to a postoperative fracture.[17] The implant selected by the surgeon for the index arthroplasty affects the risk of periprosthetic patellar fracture. A patellar prosthesis designed with a single central peg, large central peg, metal-back, and press-fit insertion is associated with postoperative fracture. The single central peg creates a stress riser while the large central peg requires additional bone resection for implantation. Metal backed components increase the contact stress across the patellofemoral joint and are a risk factor for failure.[12]
Patient factors associated with periprosthetic patellar fractures are osteopenia/osteoporosis, inflammatory arthritides, inadequate bone stock, male sex, and increased activity level.[12] Male sex is associated with more considerable patellofemoral stress from greater body weight and higher activity levels.[18]
The original classification of patellar fractures characterizes them into seven common fracture patterns: nondisplaced, transverse with displacement, inferior pole, comminuted without displacement, comminuted with displacement, vertical, or osteochondral.[1] The descriptive nature of this system provides information on the mechanism of injury but does not dictate treatment or provide prognostic information. In the AO/OTA classification of patellar fractures, extra-articular (avulsion or isolated body) fractures are classified as 34A. Vertical partial articular fractures are classified as 34B. Complete articular fractures are classified as 34C and graded in severity based on the amount of comminution.[19]
Classification of periprosthetic patellar fractures focuses on the stability of the patellar prosthesis, degree of fracture displacement, location and pattern, quality of bone stock, and competence of the extensor mechanism. While no universally accepted classification exists for periprosthetic patellar fractures, Ortiguera and Berry developed a classification system that can be used to dictate treatment. Type I fractures are most commonly treated non-operatively while Type II and III fractures often require operative intervention, repair/reconstruction of the extensor mechanism, and revision of patellar prosthesis.[11]
Ortiguera and Berry Classification of Periprosthetic Patellar Fractures[11]
- Type I: Stable implant, intact extensor mechanism
- Type II: Disrupted extensor mechanism
- Type IIIa: Loose patellar component, reasonable bone stock
- Type IIIb: Loose patellar component, inadequate bone stock
History and Physical
A thorough history and physical examination are necessary to identify the injury mechanism and other potential injuries. Patients who sustain high-energy dashboard injuries may also present with fractures to the ipsilateral acetabulum and lower extremity. Initial inspection of the injured knee is aimed at assessing soft tissue trauma. A saline load test using 155 to 175 mL of sterile saline may be warranted if there is suspicion for open injury to the knee joint.[20] Palpation of closed injuries may reveal crepitus, fracture gap, and swelling indicative of hemarthrosis. A straight-leg test must be performed to assess the extensor mechanism, although this may be limited secondary to pain.
Periprosthetic fractures of the patella may not present the same as native patella fractures. Trauma is a significant cause of periprosthetic patellar fractures; however, some patients may not recall a single episode that is responsible for a fracture. At the time of diagnosis, forty-four percent of patients with atraumatic periprosthetic patellar fractures complained of minimal or no symptoms.[11] Similar to the native patellar fractures, traumatic injuries present with diffuse anterior knee pain, tenderness to palpation, effusion, weakness, instability, and difficulty with stairs.
Evaluation
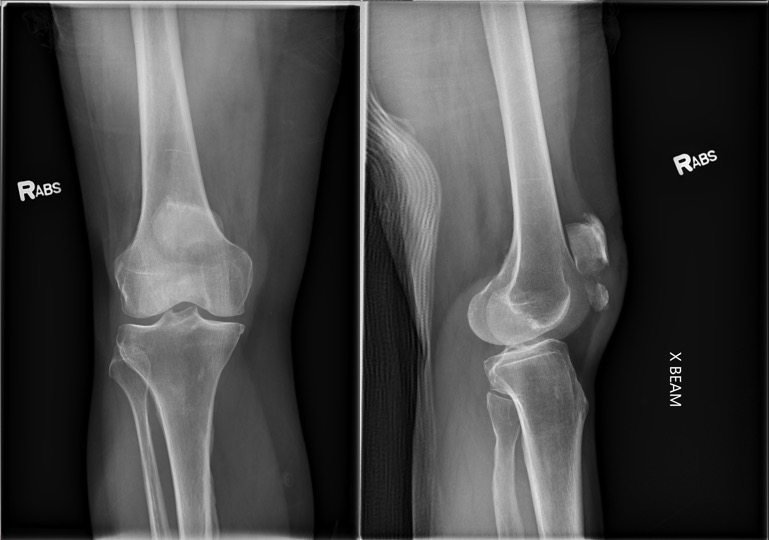
Radiographic evaluation with anteroposterior (AP) and lateral knee radiographs should be obtained. Lateral views are useful to assess for the displacement of the patellar fragments. Advanced imaging of patellar fractures is rarely warranted. Imaging of bipartite patella most commonly demonstrates a fragment at the superolateral pole. They can be differentiated from acute fractures by the appearance of smooth edges. Imaging of the contralateral knee may reveal a bilateral bipartite patella in up to 50% of cases.[10]
Patients with suspected periprosthetic patellar fractures should be evaluated with formal anteroposterior, lateral, and skyline radiographs. In rare situations, a Technetium-99m bone scan may be of use to diagnose an occult fracture or to differentiate from an acute or chronic fracture. Careful interpretation of a bone scan is required as this type of scan may be positive for 48 months following the initial injury.[21]
Treatment / Management
Restoration of the extensor mechanism is the primary treatment goal for patellar fractures. Nonoperative management is indicated for minimally displaced fractures (less than 2 to 3 mm of step-off and less than 1 to 4 mm fracture gap) with the extensor mechanism in continuity.[1] Patients with displaced patellar fractures who are not medically or psychologically fit for surgery may also undergo a trial of nonoperative treatment. A long-leg splint, knee immobilizer, or hinged knee brace locked in extension can be used to stabilize the fracture while allowing early weight-bearing. Physical therapy is recommended after the pain subsides to work on the active and active-assisted range of motion. Repeat radiographs should be obtained a week after initiation of motion exercises to evaluate for fracture displacement. Approximately six weeks after the initial injury, the patient can be started on resistance exercises.
Open reduction and internal fixation are indicated for open fractures, substantially displaced fractures, and fractures with a loss of extensor function. Urgent irrigation, debridement, and antibiotic treatment are indicated for open fractures. The Arbeitsgemeinschaft fur Osteosynthesefragen (AO)/Association for the Study of Internal Fixation (ASIF) developed the technique of tension band wire fixation as the standard of care for patellar fractures.[1] This technique converts the tension forces along the anterior fracture site into compression forces at the articular surface. As with any attempt at tension band technique, success relies heavily on a straight transverse, non-comminuted compression side. Evolutions of the surgical treatment led to the modified anterior tension band (MATB) technique, which combines an 18-gauge stainless-steel wire in a figure-of-eight configuration wrapped around two vertical Kirschner wires (K-wires). According to the AO, the MATB technique should be combined with an additional cerclage around the patella to supplement the fixation for comminuted patellar fractures. Wire migration and soft tissue irritation have prompted research into alternative materials and minimally invasive approaches. Despite the variety of techniques and instrumentations described in the literature, high union rates and clinical outcomes based on the Bostman grading scale have been reported after surgical fixation.[1][2] Other methods of fixation include tension band plating along the anterior surface, as well as circumferential cerclage wiring or plating around the perimeter of the patella. These methods of fixation are typically reserved for highly comminuted fractures in which tension band principles cannot be used.
Every attempt should be made to preserve the patella; however, resection of all (total patellectomy) or part of the patella (partial patellectomy) may be indicated in certain situations. Biomechanical studies have demonstrated that removal of the patella decreases the quadriceps strength by 50%.[5][22] Partial patellectomy is indicated for severely comminuted fractures of the superior or inferior pole that comprise less than 40% of the patellar height and are not amenable to fixation.[23] This is performed by excising the fracture fragment and advancing the quadriceps or patellar tendon via suture tunnels or suture anchors.(A1)
Postoperatively, similar to nonoperative treatment, patients are placed in a hinged knee brace locked in extension and are allowed to weight-bear as tolerated after surgical fixation. Early knee motion is usually begun at the first follow-up visit to prevent stiffness. As the pain diminishes, knee motion is progressed, and isometric strengthening of the quadriceps is initiated. The rehabilitation protocol may vary after a partial patellectomy or a tenuous fixation by delaying knee motion to ensure adequate healing.
Treatment of periprosthetic patellar fractures are complicated and should be reserved for the skillful surgeon familiar with the various operative and nonoperative options. Of utmost importance for the success of total knee arthroplasty is the competence of the extensor mechanism.[24] Transverse fractures displaced < 2 cm, vertical fractures, and comminuted fractures are often associated with an intact extensor mechanism.[13] Type I fractures have an intact extensor mechanism and a stable patella button and are best treated with six to eight weeks of immobilization in a cylinder cast or an extension brace. Fractures with > 2 cm displacement, an unstable patella button, and compromised extensor mechanism are indications for operative intervention.[13] Treatment options include open reduction with internal fixation, partial/total patellectomy, revision patella arthroplasty, patelloplasty, and extensor mechanism repair/augmentation. Surgical options may be necessary alone or in combination.[12] Type II fractures require repair or reconstruction of the extensor mechanism with suture, allograft, autograft, or xenograft. Type IIIa fractures are amenable to revision patellar arthroplasty or resection (patelloplasty). Type IIIb fractures with a loose patellar button and poor bone stock should undergo patelloplasty or total patellectomy. If patelloplasty is planned, proper patient education is required as crepitus and continued anterior knee pain is common.[11][12](B2)
Complications
Postoperative complications include symptomatic hardware,[8][9] implant failure and wire migration,[25] and knee stiffness.[26] Nonunion and infection are rare complications but are more likely in open fractures.[27] The rate of osteonecrosis of the patella following fractures is reportedly as high as 25%; however, this has not significantly affected clinical outcomes.[4]
Type I periprosthetic fractures, 18% of patients developed complications consisting of nonunion, arthrofibrosis, and patellar button loosening. Type II fractures were associated with a 50% complication rate, with 45% undergoing a revision procedure for instability, pain, and weakness. Type III fractures were associated with a 66% risk of complications.[11] Failure of fixation, extensor lag > 15 degrees, nonunion, infection, instability, and arthrofibrosis were the most common complications of Type IIIa/IIIb fractures and 25% underwent revision operation.[11]
Enhancing Healthcare Team Outcomes
Management of patella fractures will best be achieved by a specialty orthopedic trained nurse, orthopedic surgeon, and pharmacist to assist with pain control. Physical therapy may need to be involved. Interprofessional care of this injury will produce the best result. [Level V]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Melvin JS, Mehta S. Patellar fractures in adults. The Journal of the American Academy of Orthopaedic Surgeons. 2011 Apr:19(4):198-207 [PubMed PMID: 21464213]
Boström A. Fracture of the patella. A study of 422 patellar fractures. Acta orthopaedica Scandinavica. Supplementum. 1972:143():1-80 [PubMed PMID: 4516496]
Kaufer H. Mechanical function of the patella. The Journal of bone and joint surgery. American volume. 1971 Dec:53(8):1551-60 [PubMed PMID: 5121795]
Scapinelli R. Blood supply of the human patella. Its relation to ischaemic necrosis after fracture. The Journal of bone and joint surgery. British volume. 1967 Aug:49(3):563-70 [PubMed PMID: 6037574]
Carpenter JE, Kasman R, Matthews LS. Fractures of the patella. Instructional course lectures. 1994:43():97-108 [PubMed PMID: 9097140]
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. The Journal of bone and joint surgery. American volume. 2007 Apr:89(4):780-5 [PubMed PMID: 17403800]
Grace JN, Sim FH. Fracture of the patella after total knee arthroplasty. Clinical orthopaedics and related research. 1988 May:(230):168-75 [PubMed PMID: 3365890]
Torchia ME, Lewallen DG. Open fractures of the patella. Journal of orthopaedic trauma. 1996:10(6):403-9 [PubMed PMID: 8854318]
Level 2 (mid-level) evidenceAnand S, Hahnel JC, Giannoudis PV. Open patellar fractures: high energy injuries with a poor outcome? Injury. 2008 Apr:39(4):480-4. doi: 10.1016/j.injury.2007.10.032. Epub 2008 Mar 7 [PubMed PMID: 18316085]
Level 2 (mid-level) evidenceAtesok K, Doral MN, Lowe J, Finsterbush A. Symptomatic bipartite patella: treatment alternatives. The Journal of the American Academy of Orthopaedic Surgeons. 2008 Aug:16(8):455-61 [PubMed PMID: 18664634]
Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. The Journal of bone and joint surgery. American volume. 2002 Apr:84(4):532-40 [PubMed PMID: 11940611]
Level 2 (mid-level) evidenceBerry DJ, Rand JA. Isolated patellar component revision of total knee arthroplasty. Clinical orthopaedics and related research. 1993 Jan:(286):110-5 [PubMed PMID: 8425331]
Sheth NP, Pedowitz DI, Lonner JH. Periprosthetic patellar fractures. The Journal of bone and joint surgery. American volume. 2007 Oct:89(10):2285-96 [PubMed PMID: 17908909]
Rorabeck CH, Angliss RD, Lewis PL. Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instructional course lectures. 1998:47():449-58 [PubMed PMID: 9571446]
Reuben JD, McDonald CL, Woodard PL, Hennington LJ. Effect of patella thickness on patella strain following total knee arthroplasty. The Journal of arthroplasty. 1991 Sep:6(3):251-8 [PubMed PMID: 1940931]
Tria AJ Jr, Harwood DA, Alicea JA, Cody RP. Patellar fractures in posterior stabilized knee arthroplasties. Clinical orthopaedics and related research. 1994 Feb:(299):131-8 [PubMed PMID: 8119007]
Level 2 (mid-level) evidenceFiggie HE 3rd, Goldberg VM, Figgie MP, Inglis AE, Kelly M, Sobel M. The effect of alignment of the implant on fractures of the patella after condylar total knee arthroplasty. The Journal of bone and joint surgery. American volume. 1989 Aug:71(7):1031-9 [PubMed PMID: 2760078]
Tharani R, Nakasone C, Vince KG. Periprosthetic fractures after total knee arthroplasty. The Journal of arthroplasty. 2005 Jun:20(4 Suppl 2):27-32 [PubMed PMID: 15991125]
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and Dislocation Classification Compendium-2018. Journal of orthopaedic trauma. 2018 Jan:32 Suppl 1():S1-S170. doi: 10.1097/BOT.0000000000001063. Epub [PubMed PMID: 29256945]
Nord RM, Quach T, Walsh M, Pereira D, Tejwani NC. Detection of traumatic arthrotomy of the knee using the saline solution load test. The Journal of bone and joint surgery. American volume. 2009 Jan:91(1):66-70. doi: 10.2106/JBJS.G.01682. Epub [PubMed PMID: 19122080]
Level 1 (high-level) evidenceEngh GA, Ammeen DJ. Periprosthetic fractures adjacent to total knee implants: treatment and clinical results. Instructional course lectures. 1998:47():437-48 [PubMed PMID: 9571445]
Carpenter JE, Kasman RA, Patel N, Lee ML, Goldstein SA. Biomechanical evaluation of current patella fracture fixation techniques. Journal of orthopaedic trauma. 1997 Jul:11(5):351-6 [PubMed PMID: 9294799]
Level 1 (high-level) evidenceBöstman O, Kiviluoto O, Nirhamo J. Comminuted displaced fractures of the patella. Injury. 1981 Nov:13(3):196-202 [PubMed PMID: 7327739]
Cottino U, Abdel MP, Hanssen AD. Chronic extensor mechanism insufficiency in total knee arthroplasty (TKA). Current reviews in musculoskeletal medicine. 2015 Dec:8(4):368-72. doi: 10.1007/s12178-015-9292-9. Epub [PubMed PMID: 26384696]
Choi HR, Min KD, Choi SW, Lee BI. Migration to the popliteal fossa of broken wires from a fixed patellar fracture. The Knee. 2008 Dec:15(6):491-3. doi: 10.1016/j.knee.2008.06.005. Epub 2008 Aug 27 [PubMed PMID: 18752955]
Level 3 (low-level) evidenceSmith ST, Cramer KE, Karges DE, Watson JT, Moed BR. Early complications in the operative treatment of patella fractures. Journal of orthopaedic trauma. 1997 Apr:11(3):183-7 [PubMed PMID: 9181501]
Level 2 (mid-level) evidenceCatalano JB, Iannacone WM, Marczyk S, Dalsey RM, Deutsch LS, Born CT, Delong WG. Open fractures of the patella: long-term functional outcome. The Journal of trauma. 1995 Sep:39(3):439-44 [PubMed PMID: 7473905]
Level 2 (mid-level) evidence