Introduction
Peak expiratory flow measurement (peak flow) is a simple measure of the maximal flow rate that can be achieved during forceful expiration following full inspiration. Patients can learn the technique quickly, and the equipment necessary is affordable and widely available. Major societies and advocacy groups have published patient-facing websites with clear videos that demonstrate proper technique, which can help clinicians electing to start home measurements for their patients.[1]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The most widely accepted use of peak flow measurement is in the daily and/or as-needed ambulatory evaluation of asthma.[2] Obtaining a “personal best” peak flow measurement during steady state for each patient is preferable to using published normal values, and this number should be used by both patients and clinicians to evaluate disease activity objectively. Typically, this number should be obtained during a period when the patient is feeling well and has just received maximal asthma therapy. It can be denoted on the meter to aid in interpretation.
Specific instructions on how often and when an individual patient should be instructed to measure peak flow depends on patient characteristics and provider preference. For those patients who demonstrate a pattern of not having pronounced symptoms despite increasing disease activity, a clinician should outline daily (or more) measurement to identify deterioration rapidly and intervene appropriately. For those patients who are relatively well controlled and can sense worsening symptoms early in the course of an exacerbation, as-needed measurement is appropriate.
Equipment
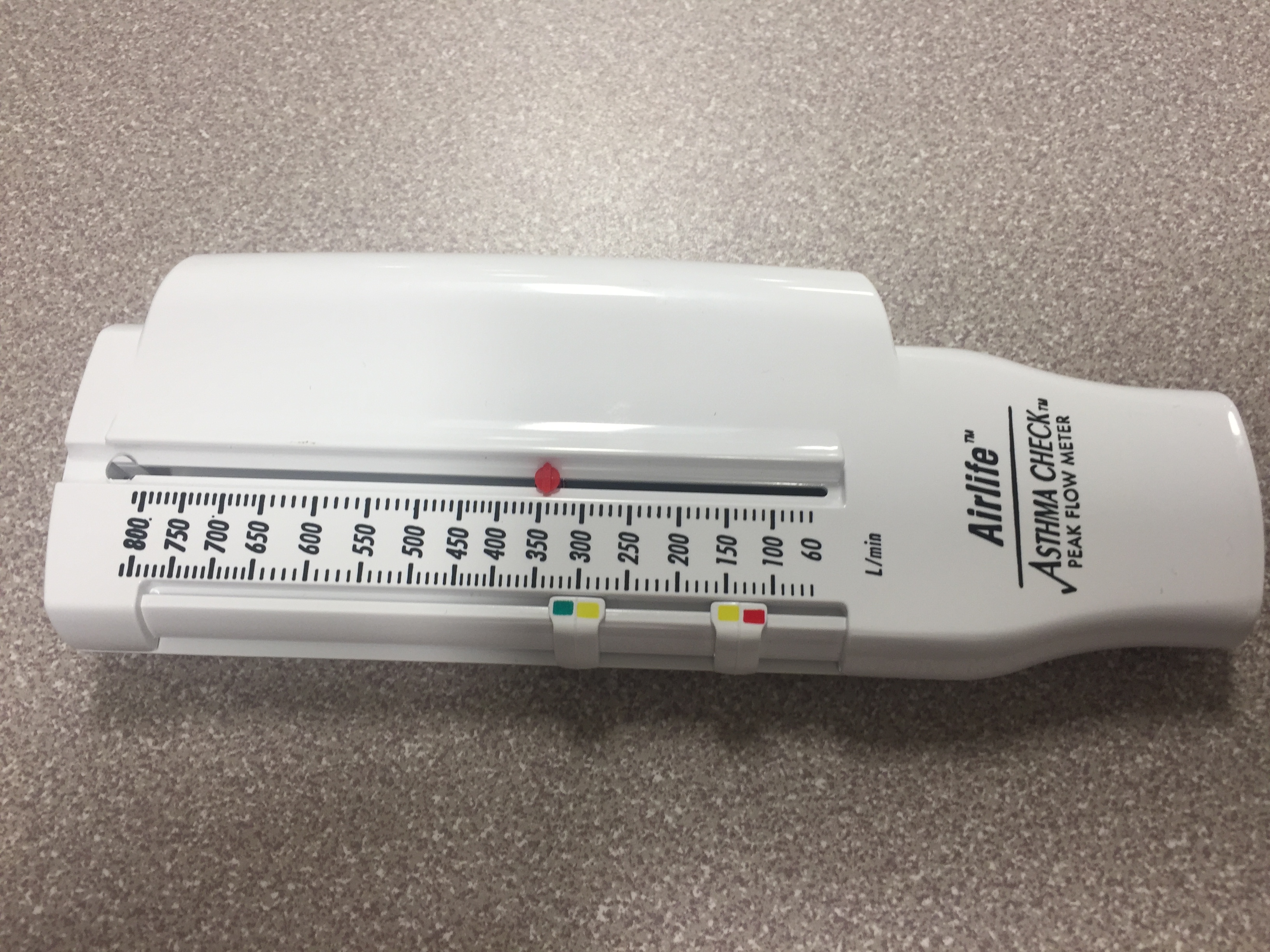
The most commonly used peak flow meter is a simple hand-held device that patients can reuse many times. Various manufacturer's models vary widely in styling, but they are typically cylindrical plastic devices with a mouthpiece on one end and an indicator and readings along the body.
Future
Peak expiratory flow rate, by itself, has limitations that make it inferior to FEV1 in clinical utility. However, traditionally FEV1 measurement at home was not practical or technologically feasible. Several miniaturized smart devices are now available on the market that will calculate both parameters, and some are even capable of interfacing with other devices to allow the automatic tabulation of data and transmission to health care providers. Prices for these devices continue to decline and are commonly available for less than one hundred dollars. Clinicians should prepare for these types of devices as they become more prevalent.
Technique or Treatment
While there are several traditional peak flow meters of various designs on the market, they all use the same general principle. First, the patient should reset the meter by sliding the marker all the way to zero on the scale. While sitting or standing up straight, the patient should take in a full, deep breath. The mouthpiece is then placed in the patient’s mouth followed by a single, fast, forceful expiration. The marker will slide outward on the numbered scale, indicating the peak expiratory flow rate for that attempt. Using the best reading from several repeated attempts is recommended; patients should not average several attempts as the lower readings usually represent faulty technique or poor effort.
Clinical Significance
Typical peak flow meters are equipped with gauge markers indicating three “zones” that can be set by the patient or clinic staff to aid users in interpreting their peak flow scores. For ease of patient interpretation, the colors of a traditional traffic light have been used to designate varying degrees of peak flow limitation. These should correlate with a written asthma action plan.
Green Zone: Usually set at 80% to 100% of personal best or normal peak flow. As long as no symptoms are present, the patient is considered at steady state. No changes are needed to the present regimen.
Yellow Zone: Fifty percent to 80% of personal best. Patients are typically instructed to employ their home action plan when they identify repeated readings in this zone. Standard action plans include increasing the dose and frequency of short-acting beta-agonist and possibly increasing the dose of inhaled corticosteroids. Action plans often contain reminders to the patient to look for and avoid, noxious stimuli such as fumes and second-hand smoke as well.
Red Zone: Fifty percent or less of personal best. Peak flow measurements in this range indicate that serious airway obstruction may be occurring and should be considered a medical emergency. Patients usually activate their Yellow Zone plan, as well as escalate to either oral corticosteroid therapy and/or seek emergency care. Some patients may be instructed to keep a supply of oral corticosteroids on hand to initiate therapy immediately.
Peak flow measurement is also useful in guiding disposition in the emergency setting. A patient with a peak flow of less than or equal to 50% without improvement despite aggressive therapy should be admitted to the hospital for ongoing care and close monitoring for signs of impeding respiratory failure. Respiratory therapy and nursing can easily obtain and report serial peak flow measurements throughout the hospital course to guide disposition decisions as well. Of note, it is a common challenge in the inpatient setting that patients will not know their personal best. In this situation, published tables of normal peak expiratory flow rates for height and weight are available.
It has been noted that peak flow rates in individual patients tend to decrease over time, likely from waning skill and effort. This observation highlights the need for ongoing retraining of techniques, even after the initial clinic visit. Some authors have recommended that this retraining occurs at every follow-up visit, in conjunction with inhaler retraining.[3]
Clinicians should be cautioned against over-reliance on this method of ambulatory monitoring alone. A comprehensive approach that accounts for both subjective symptoms, as well as objective data from the peak flow meter, has been suggested by society guidelines, and data show that this approach can decrease health care utilization.
Special Populations
Pediatrics
Children as young as five can be trained to use the peak flow meter with reliable results. However, during acute exacerbations, cooperation with the technique may be limited, and the results, therefore, need to be interpreted with caution. Tables of normal peak flow rates are available for children and adolescents. Additionally, clinicians should consider providing a second meter for the child to keep at school in the nurse’s office should concerns arise.
Pregnancy
Despite body changes that occur as pregnancy progresses, peak flow rate and personal best numbers do not change through each trimester and into the postpartum period. Changes in the observed peak flow rate in pregnant women should be treated as worsening obstruction until proven otherwise.[4]
Enhancing Healthcare Team Outcomes
Peak expiratory flow measurement (peak flow) is a measure of the maximal flow rate that can be achieved during forceful expiration following full inspiration. Clinicians and nurses should work in a team approach to educate the patient on the technique. [Level V]
Media
References
Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, Chanez P, Enright PL, Gibson PG, de Jongste JC, Kerstjens HA, Lazarus SC, Levy ML, O'Byrne PM, Partridge MR, Pavord ID, Sears MR, Sterk PJ, Stoloff SW, Sullivan SD, Szefler SJ, Thomas MD, Wenzel SE, American Thoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. American journal of respiratory and critical care medicine. 2009 Jul 1:180(1):59-99. doi: 10.1164/rccm.200801-060ST. Epub [PubMed PMID: 19535666]
Lahdensuo A, Haahtela T, Herrala J, Kava T, Kiviranta K, Kuusisto P, Perämäki E, Poussa T, Saarelainen S, Svahn T. Randomised comparison of guided self management and traditional treatment of asthma over one year. BMJ (Clinical research ed.). 1996 Mar 23:312(7033):748-52 [PubMed PMID: 8605463]
Level 1 (high-level) evidenceGannon PF, Belcher J, Pantin CF, Burge PS. The effect of patient technique and training on the accuracy of self-recorded peak expiratory flow. The European respiratory journal. 1999 Jul:14(1):28-31 [PubMed PMID: 10489825]
Brancazio LR, Laifer SA, Schwartz T. Peak expiratory flow rate in normal pregnancy. Obstetrics and gynecology. 1997 Mar:89(3):383-6 [PubMed PMID: 9052590]
Tsukioka K. [Comparison of different types of peak flow meter and reference values for peak expiratory flow (PEF) for healthy Japanese subjects]. Nihon rinsho. Japanese journal of clinical medicine. 1996 Nov:54(11):2927-32 [PubMed PMID: 8950932]
Chen X, Han P, Kong Y, Shen K. The relationship between changes in peak expiratory flow and asthma exacerbations in asthmatic children. BMC pediatrics. 2024 Apr 27:24(1):284. doi: 10.1186/s12887-024-04754-7. Epub 2024 Apr 27 [PubMed PMID: 38678177]