Introduction
The pelvic ring consists of the sacrum and 2 innominate bones, each comprising an ilium, ischium, and pubis. The bony anatomy of the ring lacks inherent stability, underscoring the essential role of strong ligamentous attachments in maintaining its structure. Displacement of the pelvic ring necessitates disruption in at least 2 sites. Pelvic ring injuries encompass a broad spectrum and exhibit various classifications and subtypes. These injuries span from simple, minimally displaced fractures of the sacrum or pubis, which can often be managed conservatively, to high-energy disruptions of the bony or ligamentous ring, which necessitate emergency medical intervention due to their life-threatening nature.[1][2]
Ligamentous Anatomy of the Pelvic Ring
- The anterior symphyseal ligaments resist external rotation.
- Pelvic floor ligaments include sacrospinous ligaments, which resist external rotation, and sacrotuberous ligaments, which resist shear and flexion.
- The posterior sacroiliac complex comprises the strongest ligaments in the body, providing greater stability to the pelvic ring than their anterior counterparts.
- This complex includes the following ligaments:
- The anterior sacroiliac ligaments resist external rotation subsequent to the failure of the pelvic floor and anterior structures.
- The interosseous sacroiliac ligament resists anterior-posterior translation of the pelvis.
- The posterior sacroiliac ligaments resist cephalad-caudad displacement of the pelvis.
- The iliolumbar ligament resists rotation and augments posterior sacroiliac ligaments.
- This complex includes the following ligaments:
The bony ring, with its ligamentous tight structures, provides a stable compartment for the hollow viscera and the following neurological and vascular structures.
Neurological structures:
- The lumbosacral trunk passes anterior to the sacral ala and sacroiliac joint.
- The L5 nerve root courses anterior to the cranial part of the sacral ala.
- The S1 nerve root exits from the anterior sacral foramina between the first and second sacral segments.[3]
Vascular structure:
- The external iliac artery passes anteriorly along the pelvic brim and terminates as the common femoral artery distal to the inguinal ligament.
- The internal iliac artery curves posteriorly approximate to the sacroiliac joint and divides into anterior and posterior divisions, terminating as obturator and superior gluteal arteries.
- Corona mortis is an anastomosis between the obturator artery and the external iliac artery or the deep inferior epigastric artery. The anastomosis is at a mean distance of 6.2 cm from the pubic symphysis.[4]
- The venous plexus in the posterior pelvis is the main source of hemorrhage associated with pelvic ring injuries.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pelvic ring injuries in young individuals are usually associated with high-energy trauma, including falls from height and motor vehicle collisions. High-force impact implies an increased incidence of associated injuries to other body regions.[5][3] Conversely, pelvic ring injuries in older populations commonly occur due to low-energy falls. Anterior-posterior compression injuries are frequently observed following equestrian saddle horn injuries and motorcycle accidents. Lateral compression injuries often occur when the pelvis is impacted by a vehicle. Vertical pelvis injuries usually result from falls or injuries involving an axial load. While mortality rates range from 1% to 15% in closed fractures, they can escalate to 50% in open fractures, with hemorrhage being the primary cause of death. Closed head injuries are notably the most common cause of mortality in lateral compression injuries.
Epidemiology
Key epidemiological points regarding pelvic ring injuries include:
- These injuries are prevalent across all age groups, accounting for approximately 3% of all skeletal fractures.
- Individuals between the age groups of 18 and 44 are most commonly affected.
- Men experience these injuries more frequently than women.
- The incidence rate is approximately 0.82 per 100,000 individuals, associated with a high overall injury severity score ranging from 25 to 48.[6][7]
Pathophysiology
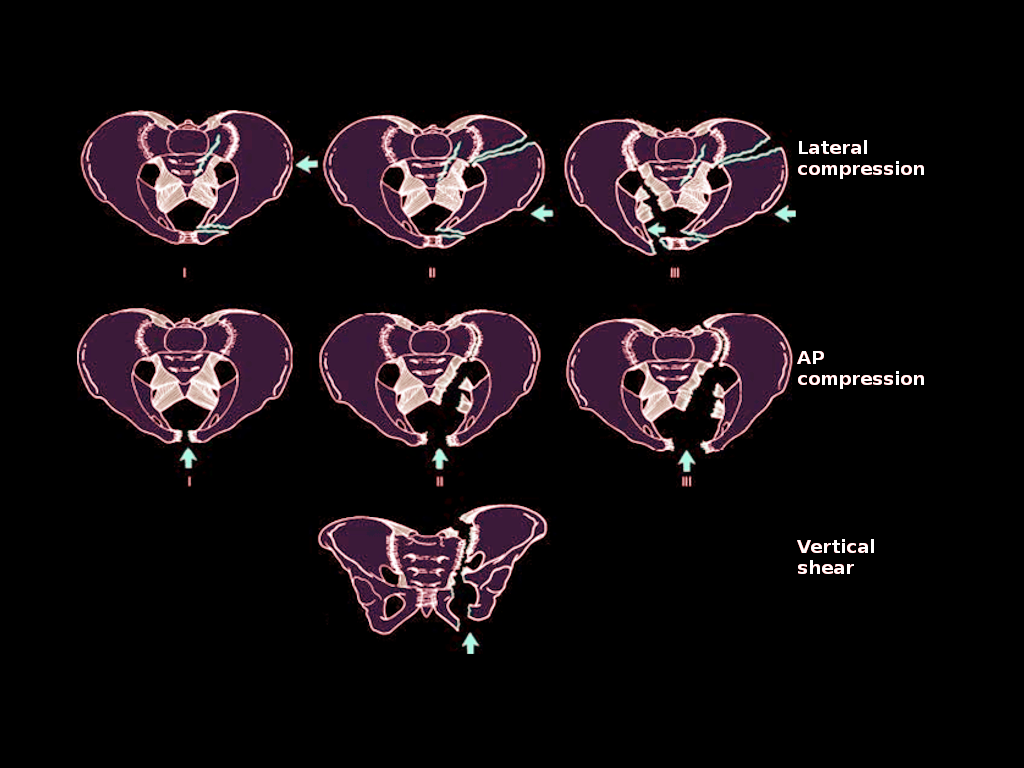
The pelvic ring suffers disruption due to direct trauma to the pelvis or indirect trauma through compression or distraction of the spine and/or femur. The pelvic ring fails in predictable patterns, as described in the classification section. Depending on the degree of injury, stabilizing ligaments of the pelvis may be disrupted, requiring stabilization (see Image. Pelvic Ring Injuries).
History and Physical
Due to the high-energy nature of pelvic ring injuries, associated morbidities require a thorough assessment. Incidence of associated trauma includes:
- Chest trauma: 63%
- Long bone fractures: 50%
- Head injuries: 40%
- Visceral organ damage: 40%
- Spinal fractures: 25%
- Intestinal injuries: 14%
- Genitourinary injuries: 6% to 15%
- Open fractures: 5%
- Mortality of open pelvis fractures is around 50%; urgent antibiotic administration is necessary.
- Rectal and vaginal exams should be performed, and breaks in the skin around the perineum should be looked for.
A pelvic ring injury can pose a life-threatening risk or may be linked to life-threatening injuries, necessitating a comprehensive examination. This examination typically includes:
- Advanced trauma life support
- Motor and sensory exam
- Physical examination of the pelvis, incorporating the push/pull test and lateral compression test
- Examination for leg length inequality not accounted for by limb fractures
- Observation for a high-riding prostate or blood at the urethral meatus, which may indicate a genitourinary injury
- Rectal and/or vaginal examination
- Assessment of the perineum, which may reveal swollen and/or mobile genitalia
Destot sign: The Destot sign refers to a palpable hematoma in the perineum above the inguinal ligament or proximal thigh, which may indicate a pelvic fracture with active bleeding.
Grey Turner sign: The Grey Turner sign is characterized by flank bruising, which is indicative of retroperitoneal bleeding.
Morel-Lavallée lesion: Morel-Lavallée lesion is an internal degloving injury resulting from skin shear during trauma, which may necessitate intervention and influence surgical planning. Clinically, it manifests as significant soft tissue abrasions, ecchymosis, or subdermal hematoma. Additionally, it can be identified on a computed tomography (CT) scan by assessing soft tissues.[1][2]
Evaluation
Evaluation of pelvic ring injuries involves various imaging modalities to assess the extent of damage and guide treatment decisions accurately. These modalities include x-rays, CT scans, and occasionally magnetic resonance imaging (MRI), each serving specific purposes in delineating the injury and its associated complications.
Imaging
- X-rays: Standard x-rays of the chest (CXR) and anteroposterior (AP) pelvis provide initial evaluation, while additional views, such as the inlet and outlet views, are crucial for assessing anterior or posterior translation and coronal plane deformities. Flamingo views aid in chronic pelvic ring instability assessment.
- CT scan: This scanning technique is essential for all pelvic ring injuries. CT scans offer detailed visualization of bony structures and help evaluate the extent of sacral injury.
- MRI: Although rarely indicated in acute pelvic ring trauma, MRI may be utilized for specific cases to characterize soft tissue injuries further.[8]
Classification
Type A: Stable
- A1: Fractures not involving the pelvic ring
- A2: Stable minimally displaced fractures of the pelvic ring
Type B: Rotationally unstable, but vertically stable
- B1: Open book
- B2: Lateral compression ipsilateral
- B3: Lateral compression contralateral
Type C: Rotationally and vertically unstable
- C1: Unilateral
- C2: Bilateral
- C3: Associated with an acetabular fracture [1]
The Young and Burgess classification: This classification system categorizes pelvic ring injuries into 4 main mechanisms.
- Lateral compression (LC)
- LC1: Anterior sacral compression fracture +/- pubic rami fractures (typically stable)
- LC2: Crescent fracture +/- pubic rami fracture (unstable)
- LC3: LC 1 or LC2 with a contralateral AP compression injury
- Anterior-posterior compression (APC)
- APC1: Minor symphysis widening or distracted ramus fracture
- APC2: Opening of symphysis greater than 2.5 cm, with disruption of sacrospinous and anterior sacroiliac ligaments, assumes posterior sacroiliac ligaments remain intact
- APC3: Complete disruption of the symphysis and sacroiliac joint
- Vertical shear (VS): Vertical displacement of the hemipelvis represents complete instability
- Combined Mechanism (CM): Any combination [9]
The Denis classification of sacral fractures: Sacral fractures are categorized into 3 zones according to the Denis classification, as mentioned below.
- Zone 1: Lateral to the sacral foramen
- Zone 2: Entering sacral foramen
- Zone 3: Medial to sacral foramen – Highest incidence of neurologic injury, including nerve root or cauda equina [2]
Lumbopelvic dissociation: Lumbopelvic dissociation refers to a fracture pattern that disrupts the continuity between the base of the spine and the pelvis, necessitating fixation. This topic is beyond the scope of this activity. Notably, bilateral sacral fractures often present with lumbopelvic dissociation, emphasizing the importance of carefully reviewing CT scans for coronal plane sacral disruptions.[10]
Treatment / Management
As recognizing a pelvic ring injury may represent a life-threatening emergency, healthcare professionals should collaborate as a team to resuscitate critically injured patients.
Advanced Trauma Life Support
Healthcare providers should avoid assuming that a patient with a pelvic ring injury does not have another source of hemorrhage. A pelvic ring injury should serve as a reminder to all clinicians of high-energy trauma and prompt them to conduct a comprehensive assessment of all body systems. Before attributing a patient's hemorrhage to a pelvic ring injury, it is essential to exclude thoracic and abdominal bleeding through thorough evaluation.
Hemorrhage Associated with High-Energy Trauma and Pelvic Ring Disruption
Pelvic ring injuries can cause significant blood loss from various sources, which include:[9] (A1)
- Pelvic venous plexus is a common source of hemorrhage in 80% of cases and can lead to a retroperitoneal hematoma, which can hold up to 4 L of blood.
- Osseous blood supply includes nutrient arteries and bleeding cancellous bone.
- Arterial injury, although less common (occurring in 10% to 20% of cases), may involve arteries such as the superior gluteal artery, which is most frequently affected in APC injuries, as well as the internal pudendal and obturator arteries in LC injuries.
Initial Management and Resuscitation
Resuscitation: In cases requiring massive transfusion, ideally, a transfusion ratio of packed red blood cells:fresh frozen plasma:platelets at 1:1:1 has been shown to improve mortality rates.
Pelvic binder/circumferential sheet placement: Temporary intervention to partially reduce the displacement of a pelvic ring injury should be placed at the level of the greater trochanters. Adding stability will help with clot formation within the pelvis and limit hemorrhage. The effect of added stability on pelvic volume is a matter of controversy.
- Indications:
- Hemodynamically unstable pelvic ring injuries, including APC and VS injuries
- LC injuries treated with a binder may risk over-compression, potentially causing harm to other pelvic structures.[11]
- Contraindications:
- Acetabular fractures
- The intervention may mask an injury from being identified:
- When the patient is hemodynamically stable upon arrival without radiographic evidence of a pelvic ring injury, the binder should be removed, and repeat imaging should be obtained.[12]
Angiography/embolization:
- Pelvic ring injuries that remain hemodynamically unstable after transfusion and binder placement should undergo further intervention. At most centers, the next step is angiography and embolization.[13] At some centers, external fixation and open pelvic packing are considered the subsequent steps; however, this approach remains controversial. Peritoneal pelvic packing in this scenario was reported to be associated with higher rates of inpatient venous thromboembolism events and sequelae compared with angioembolization.[14]
- CT angiography confirms the presence or absence of ongoing arterial hemorrhage with 98% to 100% negative predictive value.
- Ongoing bleeding after selective embolization indicates bilateral temporary internal iliac embolization, which can be effective. On the other hand, it can be complicated by gluteal necrosis and impotence.
External fixation:
- Pelvic clamp or traditional frames.
- Indicated as a temporary or definitive fixation for unstable injuries with hemodynamic instability, injuries with external rotation component, and symphyseal widening with fecal or urinary contamination.[15]
- The external fixation facilitates improving ventilation, especially in patients with chest trauma.
- Pin positions for frames: Pin positions for frames include the gluteal pillar, anterosuperior (into the iliac crest), or anteroinferior (supraacetabular). Under fluoroscopic guidance, supraacetabular pin placement offers the advantage of significantly increased sacroiliac joint stability.[16] Conversely, the lateral femoral cutaneous nerve injury risk is higher with supraacetabular pin placement.[17] (A1)
- The intervention is contraindicated in the ilium and acetabular fractures.
Anterior subcutaneous pelvic fixator (INFIX): The INFIS is a new technique to avoid complications associated with pelvic external fixation, including pin site infection. Despite yielding comparable functional outcomes, the INFIX offers advantages, including shorter operative time and reduced blood loss, when compared to symphyseal plating.[18][19] (A1)
Diverting colostomy: A diverting colostomy may be necessary in cases of open pelvic ring injury accompanied by perineal trauma.
Definitive Management
Non-operative: Indicated for stable fractures such as APC1 and LC injuries. Pubic rami fractures are managed conservatively as surgical dissection necessary for fixation outweighs the benefits.[20]
Operative: Indicated in unstable fractures such as APC, LC types 2 and 3, and VS injuries. Operative intervention is relatively indicated in APC1 and LC injuries if significant displacement is indicated by lower limb rotational deformity resulting in complete loss of rotation or leg length discrepancy of 1.5 cm or more. Other relative indications include associated trauma necessitating laparotomy, tilt fracture protruding into the perineum, and refractory pain.[21]
Open reduction internal fixation (ORIF):
- ORIF results in improved quality of reduction and better biomechanical stability compared to external fixation.
- Plates and screws across the symphysis can support the anterior ring.[22]
- Parasymphyseal pubic ramus fracture is treatable with open plating or percutaneous screw fixation.
- Sacroilial dislocation or sacral fracture can be treated with sacroiliac, transiliac transacral, or transiliac screws percutaneously.[23] A thorough understanding of pelvic ring osseous fixation pathways is necessary to perform these techniques safely. Sacral dysmorphism is common and can complicate safe percutaneous fixation of the posterior pelvic ring.[24] (B3)
- Open plating of sacroiliac joints or sacral fractures may be necessary if a closed reduction is unobtainable or the fracture pattern is not amenable to percutaneous fixation.
- ORIF approaches may include Pfannenstiel, Stoppa, or ilioinguinal approaches, which can be used to access anterior structures. In cases of inadequate reduction of the sacroiliac joint or associated sacral fractures, posterior approaches are indicated.
Percutaneous fixation: Iliosacral screw fixation is a popular technique for addressing instability of the posterior ring, particularly in cases with traumatized posterior skin that could deteriorate with ORIF.[25][26] The most common complications associated with this procedure include nerve root injury, incorrectly placed screws, and loss of reduction.[27]
Triangular osteosynthesis: Lumbosacral pedicle screw fixation combined with a sacroiliac fixation for management of lumbopelvic discontinuity. Absolute indications are still unclear.[10]
The timing for definitive fixation remains controversial. Early definitive fixation offers advantages such as pain relief, supportive care, improved reduction quality, bleeding control, and early mobility. However, it comes with the potential drawbacks of increased bleeding risk and a possible second hit in trauma patients who are not fully resuscitated.[28][29][26](B2)
Pertinent Studies and Ongoing Trials
In their 2011 study published in the Journal of Orthopaedic Trauma, Sagi et al assessed pelvic ring injuries using dynamic fluoroscopy in the operating room. They discovered that a subset of pelvic ring injuries exhibited greater instability than anticipated based on fracture pattern alone. Clarification regarding which patients necessitate examination under anesthesia (EUA) is still needed. EUA proves effective during the fixation of pelvic ring injuries, aiding in determining the extent of required fixation.[30][31]
Treatment Planning
Treatment Plans
- Advanced trauma life support:
- Healthcare providers can administer 2 large-bore intravenous (IVs) for fluid resuscitation to patients.
- Inserting a Foley catheter can be considered unless contraindicated by the presence of blood at the urethral meatus.
- Indications for conducting a retrograde cystourethrogram in male patients include symphysis disruptions, hematuria, blood at meatus, inability to void, ecchymosis or hematoma of the perineum, or high-riding or boggy prostate.
- A rectal and vaginal examinations are conducted as part of the assessment.
- Hemodynamic instability can be managed by initiating fluid resuscitation initially, and transitioning to immediate blood products, as necessary, can be considered.
- CXR: In cases of high-energy trauma, a chest X-ray (CXR) may reveal findings such as a widened mediastinum or pneumothorax.
- AP pelvis:
- Healthcare providers should aim to differentiate between APC and LC/VS/CM injury patterns.
- In cases where the symphysis has significantly widened, it likely indicates an APC pattern.
- If the symphysis is wide and the patient exhibits hemodynamic instability, applying a pelvic binder or circumferential sheet is recommended.
- For pelvis fractures or disruptions not indicative of an APC pattern, healthcare providers should consider other interventions before applying a pelvic binder.
- Traction may be considered for managing a VS injury.
- In cases where the symphysis has significantly widened, it likely indicates an APC pattern.
- Healthcare providers should aim to differentiate between APC and LC/VS/CM injury patterns.
- CT head, neck, chest, abdomen, and pelvis: Healthcare providers should order CT scans of the head, neck, chest, abdomen, and pelvis of the patient. Fine cuts with a thickness of 2 mm should be obtained specifically for the pelvis. Importantly, they should also consider the possibility of other injuries, including hemorrhage in the head, neck, chest, abdomen, and pelvis, when evaluating a patient.
- In cases where the patient remains hemodynamically unstable:
- If an identifiable source of bleeding outside the pelvis is identified, healthcare providers should control the bleeding by other means according to general surgery recommendations.
- If no other source of bleeding is identified apart from the pelvic ring injury, interventional radiology embolization is typically the preferred course of action in most centers. However, this approach remains controversial when it comes to emergent pelvic external fixation and pelvic packing.
- After the patient is hemodynamically stable:
- Once the patient achieves hemodynamic stability, healthcare providers should obtain inlet and outlet X-rays of the pelvis, primarily for surgical planning purposes.
- If the patient presents with polytrauma, it may necessitate delaying definitive surgical intervention. In such cases, temporary external fixation following damage control orthopedic principles is recommended.
- Once the patient is deemed stable, with corrected lactate levels, definitive fixation should be pursued.
Prognosis
Mortality rates associated with pelvic ring injuries, particularly in cases of hemodynamic instability, remain high due to factors such as rapid exsanguination, challenging hemostasis, and the severity of associated injuries.[32][9][33][34] Recent advancements have shown a notable improvement in mortality rates related to pelvic ring injuries compared to earlier years, with a reduction from 9.1% to 4.9%.[35] This improvement is even more significant when considering factors such as the patient's age and Abbreviated Injury Severity (AIS) score for the brain, chest, and abdomen.
The Young and Burgess classification has predictive value for mortality in pelvic ring injuries. When combining the classification into stable (LC1 and APC1) versus unstable (LC2, LC3, APC 2, and APC 3) categories, stable injuries exhibit a mortality rate of 7.9%, whereas unstable injuries have a mortality rate of 11.5%.[36] Furthermore, reducing the posterior ring within 1 cm has been associated with improved long-term outcomes.
Additionally, the return-to-work rate following pelvic ring injuries is highly variable, with the majority of patients reporting some degree of persistent impairment, as discussed below.[37]
- 24% of patients lose their jobs
- 34% of patients return to work but with modified duties
- 46% of patients are unable to perform their pre-injury duties
Male gender and older populations are associated with higher mortality rates in pelvic ring injuries. However, females who undergo symphysis fixation can still have safe vaginal deliveries, provided that both the front and back of the pelvis are not restrained by fixation.[38][39]
Complications
The complications associated with pelvic ring injuries are discussed below.
Malunion
- Controversy exists surrounding the definition or measurement of displacement and malunion in pelvic ring injuries.
- Patients who achieve anatomic reductions tend to have better outcomes, although displacements less than 1 cm are often considered tolerable.
- Distinguishing stable patterns from unstable patterns can sometimes be challenging.
- In select cases or to guide treatment during surgery, manipulation under anesthesia may be considered to determine stability.
- Nonoperative treatment of complete sacral fractures with ipsilateral rami fractures may lead to displacement over time in 39% of cases, while the rate increases to 68% for those with bilateral rami fractures.[40][41]
Hardware Failure
- Micromotion is present in a well-aligned and healed pelvic ring. Therefore, hardware failure rates tend to be high over time. However, if the pelvic ring has fully healed, no displacement will occur in the event of hardware failure, and this alone does not necessitate hardware removal.
- Plating across the symphysis exhibits a hardware failure rate of 43% at 1 year, with 97% of these failures being asymptomatic.[42]
Neurological Dysfunction
Denis 3 fractures of the sacrum have approximately a 50% rate of neurologic dysfunction of lumbosacral nerve roots.
Sexual Dysfunction
- Erectile dysfunction occurs in 46% of males after pelvic ring injury.
- Dyspareunia occurs in 56% of females after pelvic ring injury, 91% with APC injuries, and 79% of patients treated with symphysial plating.[43][44]
Chronic Pain and Disability
Refer to the Prognosis section for more information.
Infections
- Infections can occur in up to 16% of cases when utilizing a posterior approach to the sacrum.
- Obesity has been identified as a factor that increases the risk of complications and the likelihood of requiring reoperation.[45]
Deep Vein Thrombosis/Pulmonary Embolism
In cases of pelvic ring injury, the need for an inferior vena cava (IVC) filter may arise to prevent deep vein thrombosis (DVT) or pulmonary embolism.[46]
Combined Injuries
Combined injuries involving both the acetabulum and pelvic ring are often associated with high rates of complications. Specifically, hip dislocation has been linked to an increased rate of complications.[47]
Postoperative and Rehabilitation Care
Depending on the specific injury and treatment method, the patient may require a period of weight-bearing restrictions to one or both extremities. Nursing and therapy are necessary to assist with a patient's return to function. DVT prophylaxis postoperatively is paramount.
Deterrence and Patient Education
Clinicians are advised to address patient expectations early in the encounter. This includes having conversations about realistic outcomes and the possibility of experiencing chronic discomfort to some degree. Additionally, discussing intimate issues such as erectile dysfunction or dyspareunia is crucial for ensuring the overall well-being of the patient. Referrals to OB-GYN or urology specialists should be made as deemed necessary.
Enhancing Healthcare Team Outcomes
Given the complexity and high mortality rate associated with these injuries, a multidisciplinary approach is imperative for their management, encompassing resuscitation, bleeding control, and bone injury management, particularly in the initial hours post-injury.[48] Effective interprofessional communication is essential, alongside active patient involvement in their care. Typically, patients with pelvic ring injuries necessitate the collaborative efforts of multiple clinicians.
The roles of the interprofessional team are briefly described below.
- A urologist is necessary if a urethral injury is present, with patients often requiring suprapubic catheterization. It is essential to avoid placing the catheter in a manner that obstructs diverting ileostomy creation for the general surgeon or interferes with pelvic incisions for the orthopedic surgeon. To minimize interference with surgical interventions on the pelvis, diverting ileostomy/colostomy or suprapubic catheters should be positioned as cephalad as possible.
- A general surgeon may be required to divert the fecal flow by creating a diverting ileostomy or colostomy.
- A radiologist is critical in localizing injuries and assessing their extent. Additionally, an interventional radiologist may be required for arterial embolization in cases of uncontrolled hemorrhage. Patients with these injuries are often managed in the trauma or surgery intensive care unit (ICU) and require close monitoring by nursing staff. DVT and pressure sore prophylaxis are also essential for these patients. As most patients cannot consume an oral diet for a few days or weeks, a dietary consultation for total parenteral nutrition may be necessary, especially for patients with stomas. Furthermore, a stoma nurse is needed to educate the patient and their family about stoma care, dietary modifications, hygiene maintenance, and reporting any issues back to the clinicians.
- Pain control and antimicrobial therapy may be necessary, and a pharmacist is responsible for overseeing medication reconciliation and dosing. They should also inform the team of any potential interactions or dosing issues.
As these patients are frequently bedridden for extended periods, it is crucial to involve physical and occupational therapy to exercise muscles and maintain function. These therapists can provide valuable insights into the patient's progress or lack thereof as they undergo rehabilitation. Additionally, a mental health nurse should assess the patient before discharge, as depression and anxiety are common following pelvic trauma. Recognizing that the road to recovery is often lengthy and unpredictable is crucial.
Following discharge, most patients with pelvic ring injuries require extensive rehabilitation and ongoing follow-up with their specialists and primary care clinicians. In summary, managing pelvic ring injuries or fractures necessitates an interprofessional team approach, involving physicians, specialists, specialty-trained nurses, and pharmacists collaborating across disciplines to achieve optimal patient outcomes. Pelvic trauma represents a significant event in patients' lives; despite receiving optimal care, it is associated with high morbidity rates. Many patients experience ongoing disability post-injury and struggle to return to work. Daily living activities often become challenging, necessitating assistance with ambulation. The long-term prognosis for most patients with pelvic ring injuries remains guarded.
Media
(Click Image to Enlarge)
References
Berger-Groch J, Thiesen DM, Grossterlinden LG, Schaewel J, Fensky F, Hartel MJ. The intra- and interobserver reliability of the Tile AO, the Young and Burgess, and FFP classifications in pelvic trauma. Archives of orthopaedic and trauma surgery. 2019 May:139(5):645-650. doi: 10.1007/s00402-019-03123-9. Epub 2019 Feb 4 [PubMed PMID: 30715568]
Beckmann NM, Chinapuvvula NR. Sacral fractures: classification and management. Emergency radiology. 2017 Dec:24(6):605-617. doi: 10.1007/s10140-017-1533-3. Epub 2017 Jun 27 [PubMed PMID: 28656329]
Durkin A, Sagi HC, Durham R, Flint L. Contemporary management of pelvic fractures. American journal of surgery. 2006 Aug:192(2):211-23 [PubMed PMID: 16860634]
Tornetta P 3rd, Hochwald N, Levine R. Corona mortis. Incidence and location. Clinical orthopaedics and related research. 1996 Aug:(329):97-101 [PubMed PMID: 8769440]
Pohlemann T, Tscherne H, Baumgärtel F, Egbers HJ, Euler E, Maurer F, Fell M, Mayr E, Quirini WW, Schlickewei W, Weinberg A. [Pelvic fractures: epidemiology, therapy and long-term outcome. Overview of the multicenter study of the Pelvis Study Group]. Der Unfallchirurg. 1996 Mar:99(3):160-7 [PubMed PMID: 8685720]
Level 2 (mid-level) evidencePapakostidis C, Giannoudis PV. Pelvic ring injuries with haemodynamic instability: efficacy of pelvic packing, a systematic review. Injury. 2009 Nov:40 Suppl 4():S53-61. doi: 10.1016/j.injury.2009.10.037. Epub [PubMed PMID: 19895954]
Level 1 (high-level) evidenceGrotz MR, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury. 2005 Jan:36(1):1-13 [PubMed PMID: 15589906]
Benjamin ER, Jakob DA, Myers L, Liasidis P, Lewis M, Fu Y, Demetriades D. The trauma pelvic X-ray: Not all pelvic fractures are created equally. American journal of surgery. 2022 Jul:224(1 Pt B):489-493. doi: 10.1016/j.amjsurg.2022.01.009. Epub 2022 Jan 31 [PubMed PMID: 35131085]
Cullinane DC, Schiller HJ, Zielinski MD, Bilaniuk JW, Collier BR, Como J, Holevar M, Sabater EA, Sems SA, Vassy WM, Wynne JL. Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture--update and systematic review. The Journal of trauma. 2011 Dec:71(6):1850-68. doi: 10.1097/TA.0b013e31823dca9a. Epub [PubMed PMID: 22182895]
Level 1 (high-level) evidenceAcklin YP, Zderic I, Richards RG, Schmitz P, Gueorguiev B, Grechenig S. Biomechanical investigation of four different fixation techniques in sacrum Denis type II fracture with low bone mineral density. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2018 Jun:36(6):1624-1629. doi: 10.1002/jor.23798. Epub 2017 Dec 5 [PubMed PMID: 29106756]
Ghaemmaghami V, Sperry J, Gunst M, Friese R, Starr A, Frankel H, Gentilello LM, Shafi S. Effects of early use of external pelvic compression on transfusion requirements and mortality in pelvic fractures. American journal of surgery. 2007 Dec:194(6):720-3; discussion 723 [PubMed PMID: 18005760]
Swartz J, Vaidya R, Hudson I, Oliphant B, Tonnos F. Effect of Pelvic Binder Placement on OTA Classification of Pelvic Ring Injuries Using Computed Tomography. Does It Mask the Injury? Journal of orthopaedic trauma. 2016 Jun:30(6):325-30. doi: 10.1097/BOT.0000000000000515. Epub [PubMed PMID: 26709813]
Wiley M, Black S, Martin C, Barnwell J, Starr A, Sathy A. Complications After Pelvic Arteriography in Patients With Pelvic Ring Disruptions. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Nov 1:26(21):765-772. doi: 10.5435/JAAOS-D-17-00198. Epub [PubMed PMID: 30106762]
Patterson JT, Wier J, Gary JL. Preperitoneal Pelvic Packing for Hypotension Has a Greater Risk of Venous Thromboembolism Than Angioembolization: Management of Refractory Hypotension in Closed Pelvic Ring Injury. The Journal of bone and joint surgery. American volume. 2022 Oct 19:104(20):1821-1829. doi: 10.2106/JBJS.22.00252. Epub 2022 Aug 12 [PubMed PMID: 35939780]
Wojahn RD, Gardner MJ. Fixation of Anterior Pelvic Ring Injuries. The Journal of the American Academy of Orthopaedic Surgeons. 2019 Sep 15:27(18):667-676. doi: 10.5435/JAAOS-D-17-00839. Epub [PubMed PMID: 30889037]
Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M. Effect of pin location on stability of pelvic external fixation. Clinical orthopaedics and related research. 1999 Apr:(361):237-44 [PubMed PMID: 10212618]
Level 1 (high-level) evidenceWong JM, Bucknill A. Fractures of the pelvic ring. Injury. 2017 Apr:48(4):795-802. doi: 10.1016/j.injury.2013.11.021. Epub 2013 Dec 2 [PubMed PMID: 24360668]
Vaidya R, Woodbury D, Nasr K. Anterior Subcutaneous Internal Pelvic Fixation/INFIX: A Systemic Review. Journal of orthopaedic trauma. 2018 Sep:32 Suppl 6():S24-S30. doi: 10.1097/BOT.0000000000001248. Epub [PubMed PMID: 30095678]
Patel S, Aggarwal S, Jindal K, Kumar V, Sharma S. Outcomes and complications of the INFIX technique for unstable pelvic ring injuries with high-velocity trauma: a systematic review and meta-analysis. Archives of orthopaedic and trauma surgery. 2022 May:142(5):787-803. doi: 10.1007/s00402-020-03742-7. Epub 2021 Jan 11 [PubMed PMID: 33426606]
Level 1 (high-level) evidenceTile M. Pelvic ring fractures: should they be fixed? The Journal of bone and joint surgery. British volume. 1988 Jan:70(1):1-12 [PubMed PMID: 3276697]
Olson SA, Pollak AN. Assessment of pelvic ring stability after injury. Indications for surgical stabilization. Clinical orthopaedics and related research. 1996 Aug:(329):15-27 [PubMed PMID: 8769432]
Langford JR, Burgess AR, Liporace FA, Haidukewych GJ. Pelvic fractures: part 2. Contemporary indications and techniques for definitive surgical management. The Journal of the American Academy of Orthopaedic Surgeons. 2013 Aug:21(8):458-68. doi: 10.5435/JAAOS-21-08-458. Epub [PubMed PMID: 23908252]
Ziran N, Collinge CA, Smith W, Matta JM. Trans-sacral screw fixation of posterior pelvic ring injuries: review and expert opinion. Patient safety in surgery. 2022 Jul 27:16(1):24. doi: 10.1186/s13037-022-00333-w. Epub 2022 Jul 27 [PubMed PMID: 35897108]
Level 3 (low-level) evidenceLucas JF, Routt ML Jr, Eastman JG. A Useful Preoperative Planning Technique for Transiliac-Transsacral Screws. Journal of orthopaedic trauma. 2017 Jan:31(1):e25-e31. doi: 10.1097/BOT.0000000000000708. Epub [PubMed PMID: 27661733]
Zarei M, Moosavi M, Saghebdoust S, Shafizadeh M, Rostami M. Percutaneous iliosacral screw insertion with only outlet and inlet fluoroscopic view for unstable pelvic ring injuries: Clinical and radiological outcomes. Surgical neurology international. 2022:13():455. doi: 10.25259/SNI_616_2022. Epub 2022 Sep 30 [PubMed PMID: 36324935]
Tile M. Acute Pelvic Fractures: II. Principles of Management. The Journal of the American Academy of Orthopaedic Surgeons. 1996 May:4(3):152-161 [PubMed PMID: 10795050]
Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Posterior screw fixation in rotationally unstable pelvic ring injuries. Injury. 2011 Oct:42(10):992-6. doi: 10.1016/j.injury.2011.04.005. Epub 2011 May 6 [PubMed PMID: 21529802]
Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. The Journal of trauma. 2010 Sep:69(3):677-84. doi: 10.1097/TA.0b013e3181e50914. Epub [PubMed PMID: 20838139]
Enninghorst N, Toth L, King KL, McDougall D, Mackenzie S, Balogh ZJ. Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: a feasible option. The Journal of trauma. 2010 Apr:68(4):935-41. doi: 10.1097/TA.0b013e3181d27b48. Epub [PubMed PMID: 20386287]
Level 2 (mid-level) evidenceSagi HC, Coniglione FM, Stanford JH. Examination under anesthetic for occult pelvic ring instability. Journal of orthopaedic trauma. 2011 Sep:25(9):529-36. doi: 10.1097/BOT.0b013e31822b02ae. Epub [PubMed PMID: 21857421]
Level 2 (mid-level) evidenceAvilucea FR, Archdeacon MT, Collinge CA, Sciadini M, Sagi HC, Mir HR. Fixation Strategy Using Sequential Intraoperative Examination Under Anesthesia for Unstable Lateral Compression Pelvic Ring Injuries Reliably Predicts Union with Minimal Displacement. The Journal of bone and joint surgery. American volume. 2018 Sep 5:100(17):1503-1508. doi: 10.2106/JBJS.17.01650. Epub [PubMed PMID: 30180059]
Arvieux C, Thony F, Broux C, Ageron FX, Rancurel E, Abba J, Faucheron JL, Rambeaud JJ, Tonetti J. Current management of severe pelvic and perineal trauma. Journal of visceral surgery. 2012 Aug:149(4):e227-38. doi: 10.1016/j.jviscsurg.2012.06.004. Epub 2012 Jul 20 [PubMed PMID: 22818970]
Magnone S, Coccolini F, Manfredi R, Piazzalunga D, Agazzi R, Arici C, Barozzi M, Bellanova G, Belluati A, Berlot G, Biffl W, Camagni S, Campanati L, Castelli CC, Catena F, Chiara O, Colaianni N, De Masi S, Di Saverio S, Dodi G, Fabbri A, Faustinelli G, Gambale G, Capponi MG, Lotti M, Marchesi G, Massè A, Mastropietro T, Nardi G, Niola R, Nita GE, Pisano M, Poiasina E, Poletti E, Rampoldi A, Ribaldi S, Rispoli G, Rizzi L, Sonzogni V, Tugnoli G, Ansaloni L. Management of hemodynamically unstable pelvic trauma: results of the first Italian consensus conference (cooperative guidelines of the Italian Society of Surgery, the Italian Association of Hospital Surgeons, the Multi-specialist Italian Society of Young Surgeons, the Italian Society of Emergency Surgery and Trauma, the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care, the Italian Society of Orthopaedics and Traumatology, the Italian Society of Emergency Medicine, the Italian Society of Medical Radiology -Section of Vascular and Interventional Radiology- and the World Society of Emergency Surgery). World journal of emergency surgery : WJES. 2014 Mar 7:9(1):18. doi: 10.1186/1749-7922-9-18. Epub 2014 Mar 7 [PubMed PMID: 24606950]
Level 3 (low-level) evidencePerkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. The bone & joint journal. 2014 Aug:96-B(8):1090-7. doi: 10.1302/0301-620X.96B8.33383. Epub [PubMed PMID: 25086126]
Level 2 (mid-level) evidenceMarchand LS, Sepehri A, Hannan ZD, Zaidi SMR, Bangura AT, Morrison JJ, Manson TT, Slobogean GP, O'Hara NN, O'Toole RV. Pelvic Ring Injury Mortality: Are We Getting Better? Journal of orthopaedic trauma. 2022 Feb 1:36(2):81-86. doi: 10.1097/BOT.0000000000002210. Epub [PubMed PMID: 34128497]
Manson T, O'Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? Journal of orthopaedic trauma. 2010 Oct:24(10):603-9. doi: 10.1097/BOT.0b013e3181d3cb6b. Epub [PubMed PMID: 20871246]
Level 2 (mid-level) evidenceAprato A, Joeris A, Tosto F, Kalampoki V, Rometsch E, Favuto M, Stucchi A, Azi M, Massè A. Are work return and leaves of absence predictable after an unstable pelvic ring injury? Journal of orthopaedics and traumatology : official journal of the Italian Society of Orthopaedics and Traumatology. 2016 Jun:17(2):169-73. doi: 10.1007/s10195-015-0379-2. Epub 2015 Sep 28 [PubMed PMID: 26416030]
Vallier HA, Cureton BA, Schubeck D. Pregnancy outcomes after pelvic ring injury. Journal of orthopaedic trauma. 2012 May:26(5):302-7. doi: 10.1097/BOT.0b013e31822428c5. Epub [PubMed PMID: 22048182]
Level 2 (mid-level) evidenceCannada LK, Barr J. Pelvic fractures in women of childbearing age. Clinical orthopaedics and related research. 2010 Jul:468(7):1781-9. doi: 10.1007/s11999-010-1289-5. Epub [PubMed PMID: 20333494]
Level 2 (mid-level) evidenceBruce B, Reilly M, Sims S. OTA highlight paper predicting future displacement of nonoperatively managed lateral compression sacral fractures: can it be done? Journal of orthopaedic trauma. 2011 Sep:25(9):523-7. doi: 10.1097/BOT.0b013e3181f8be33. Epub [PubMed PMID: 21857419]
Level 2 (mid-level) evidenceStine S, Washington A, Sen RK, Nasr K, Vaidya R. Pelvic Malunion: A Systematic Review, Dichotomy of Definitions and Treatment. Medicina (Kaunas, Lithuania). 2022 Aug 14:58(8):. doi: 10.3390/medicina58081098. Epub 2022 Aug 14 [PubMed PMID: 36013565]
Level 1 (high-level) evidenceMorris SA, Loveridge J, Smart DK, Ward AJ, Chesser TJ. Is fixation failure after plate fixation of the symphysis pubis clinically important? Clinical orthopaedics and related research. 2012 Aug:470(8):2154-60. doi: 10.1007/s11999-012-2427-z. Epub [PubMed PMID: 22707071]
Level 2 (mid-level) evidenceCeylan HH, Kuyucu E, Erdem R, Polat G, Yιlmaz F, Gümüş B, Erdil M. Does pelvic injury trigger erectile dysfunction in men? Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2015:18(4):229-31 [PubMed PMID: 26764545]
Vallier HA, Cureton BA, Schubeck D. Pelvic ring injury is associated with sexual dysfunction in women. Journal of orthopaedic trauma. 2012 May:26(5):308-13. doi: 10.1097/BOT.0b013e31821d700e. Epub [PubMed PMID: 22011632]
Jaeblon T, Perry KJ, Kufera JA. Waist-Hip Ratio Surrogate Is More Predictive Than Body Mass Index of Wound Complications After Pelvic and Acetabulum Surgery. Journal of orthopaedic trauma. 2018 Apr:32(4):167-173. doi: 10.1097/BOT.0000000000001102. Epub [PubMed PMID: 29315199]
Dashe J, Parisien RL, Pina M, De Giacomo AF, Tornetta P 3rd. Is the Caprini Score Predictive of Venothromboembolism Events in Orthopaedic Fracture Patients? Journal of orthopaedic trauma. 2019 Jun:33(6):269-275. doi: 10.1097/BOT.0000000000001451. Epub [PubMed PMID: 31124908]
Cunningham B, Pearson J, McGwin G, Gardner W, Kiner D, Nowotarski P, Spitler CA. What are the risk factors for complications after combined injury of the pelvic ring and acetabulum? European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2023 Feb:33(2):341-346. doi: 10.1007/s00590-021-03189-5. Epub 2022 Jan 26 [PubMed PMID: 35079877]
Biffl WL, Smith WR, Moore EE, Gonzalez RJ, Morgan SJ, Hennessey T, Offner PJ, Ray CE Jr, Franciose RJ, Burch JM. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Annals of surgery. 2001 Jun:233(6):843-50 [PubMed PMID: 11407336]