Introduction
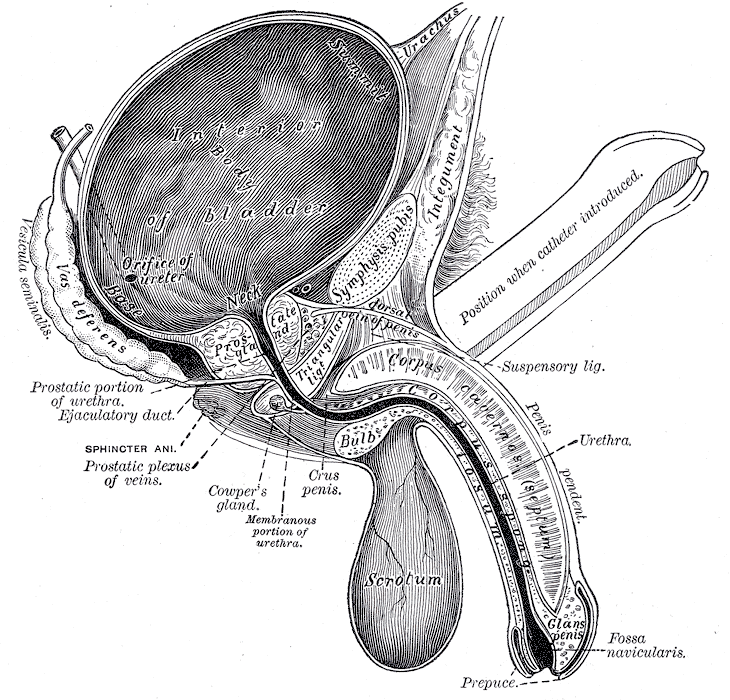
The penis is a male organ that is used for reproduction and urination which is located within the urogenital triangle between the perineal membrane superiorly and deep perineal fascia inferiorly. Its composition divides it into 3 parts: the glans, body, and root. Dorsally, it is composed of the paired corpora cavernosa and ventrally the corpus spongiosum which contains the urethra. The anatomical positions of the penis are according to the erect penis with the dorsal direction being closer to the head and ventral direction being closer to the feet. The tunica albuginea is a fibrous sheet which encapsulates the cavernous body. Buck's fascia, also known as deep fascia of the penis is superficial to the tunica albuginea and is the continuation of the deep perineal fascia which covers the corpora cavernosa and corpus spongiosum together. The spongy urethra is contained within the corpus spongiosum. The crura of the penis is between the 2 corpora cavernosa in the median plane externally. The corpora cavernosa is separated by the septum of the penis internally. The attachment of the penis consists of the bulb, crura, and ischiocavernosus and bulbospongiosus muscles, which collectively makes up the root of the penis. The bulb of the penis and crura contain erectile tissue. The middle portion of the penis is suspended and known as the body of the penis. The body of the penis lacks muscles and consists mostly of corpora cavernosa, corpus spongiosum, and spongy urethra with supporting skin, connective tissue, and blood, lymph, and fascia. The distal part of the penis is known as the glans penis. The proximal portion of the glans is termed the corona. The neck of the corona glans separates it from the body of the penis. The tip of the glans contains the opening to the urethra, known as the meatus. There is loose connective tissue between the thin skin of the penis and the tunica albuginea. The prepuce or foreskin is the second skin layer that covers the glans penis. The frenulum of the prepuce connects it to the urethral surface of the penis glans. The suspensory ligament of the penis is part of the deep fascia that arises from the anterior surface of the pubic symphysis. The fundiform ligament of the penis descends in the midline from the linea alba anterior to the pubic symphysis and splits to surround the penis and then unites and blends inferiorly with the dartos fascia forming the scrotal septum.[1][2][3][4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The 2 main functions of the penis are intercourse and urination. For intercourse, the penis must be erect. Erection occurs via parasympathetic innervation which allows engorgement of the corporal bodies. The bulbospongiosus and ischiocavernosus muscle compress the veins to prevent them from draining blood from the corpora cavernosa. The erectile tissue of the cavernosum becomes firm and enlarged when the erection occurs. The emission phase is due to the sympathetic response and occurs when semen exits the vas deferens to the ejaculatory ducts where fluid from the seminal glands are added. They then continue onto the prostatic urethra where the prostatic fluid is added. The ejaculation phase is due to the sympathetic response and is when semen exits from the urethra through the external urethral orifice. After ejaculation, the penis becomes flaccid again due to the sympathetic stimulation and constriction of the coiled helicine arteries and relaxation of the bulbospongiosus and ischiocavernosus muscles allowing blood to drain from the cavernous spaces.[5][6][7]
The other function of the penis is to drain urine from the body. Urine starts draining from the bladder into the bladder neck where the internal urethral sphincter will relax to allow urine to pass via involuntary control of the parasympathetic system. Urine will then pass into the prostatic urethra and the membranous urethra. The external sphincter will relax to allow urine to pass from the membranous urethra into the spongy penile urethra, then into the navicular fossa and out of the urethra through the external urethral orifice.
Embryology
The male penis is derived in the fetus from the genital tubercle. The genital tubercle starts developing to become the phallus due to the influence of androgens from the testis. The elongation process drags the urethral folds ahead to become the lateral walls, which belongs to the urethral groove. The epithelial lining, which is from the groove, develop into the urethral plate. The penile urethra is created when both the urethral folds enclose on top of the urethral plate. This process usually occurs towards the end of month three. The urethra's most distal part is created at the end of month 4 and ends at the external urethral meatus. The 2 urethral folds come together and fuse, this part will eventually become the spongy body. Then above the spongy body, there will be 2 cavernous bodies that arise, which will eventually become the corpora cavernosa.
Blood Supply and Lymphatics
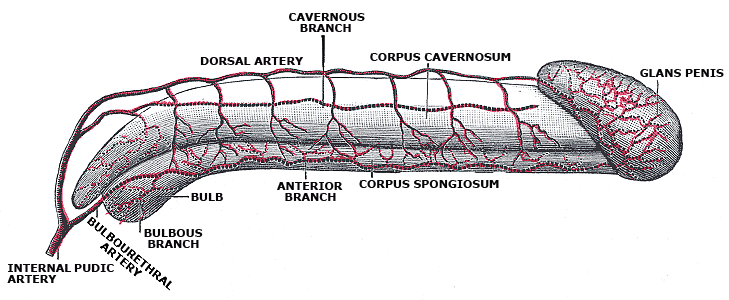
The branches of the internal pudendal arteries are the main supplier of blood to the penis. The dorsal arteries of the penis run along the dorsal vein between the corpora cavernosa to supply the fibrous tissue surrounding the corpora cavernosa, corpus spongiosum, spongy urethra, and penile skin. The deep arteries of the penis run in the center of each corpora cavernosa to supply the erectile tissue of the penis. The helicine arteries of the penis are branches of the deep arteries of the penis which are coiled when the penis is flaccid. The arteries of the bulb of the penis supply the bulbous part of the corpus spongiosum, urethra, and bulbourethral gland. The superficial and deep branches of the external pudendal arteries supply the penile skin.
The deep dorsal vein of the penis receives blood from the venous plexus which receives drained blood from the cavernous spaces. The superficial dorsal vein drains blood from the skin and subcutaneous tissue of the penis.
The skin of the penis and all of the perineum excluding the glans penis drain lymph to the superficial inguinal nodes. The lymphatics of the intermediate and proximal parts of the urethra and cavernous bodies drain into the internal iliac lymph nodes. The distal spongy urethra and glans penis drain to the deep inguinal nodes.
Nerves
The penis innervation is from spinal cord segments of the S2 to S4. These cord segments pass through the pelvic splanchnic nerves. The spinal ganglia of S2 to S4 passes through the pudendal nerves. The dorsal nerve provides sympathetic plus sensory innervation to the penis. The pudendal nerve branches to become the dorsal nerve of the penis. The nerve runs next to the dorsal artery and supplies the skin and glans penis also. The glans penis has a copious amount of sensory nerve endings. The root of the penis has innervation from the ilioinguinal nerve. The cavernous nerves have parasympathetic fibers that innervate the helicine arteries which supply erectile tissue.
Muscles
The bulbospongiosus muscles cross the pelvic outlet intersecting with the superficial transverse perineal muscles. These structures support the perineal body and pelvic viscera. The bulbospongiosus muscles compress the bulb of the penis and the corpus spongiosum which can aid in emptying the spongy urethra. The anterior fibers of the muscle surround the proximal part of the body of the penis. These fibers can increase the pressure on the erectile tissue in the root of the penis for erections. The bulbospongiosus muscle can compress the deep dorsal veins to prevent drainage of the cavernous spaces and help promote erection of the penis. The root of the penis contains the crura which is encircled by the ischiocavernosus muscle. The muscle can push blood to the distal parts of the corpora cavernosa and help with erections. The muscle can also lead to compression of the deep dorsal vein of the penis as it is leaving the crus of the penis and restrict venous outflow to help with erections.
Physiologic Variants
Hypospadias is a fairly common physiologic variant. The external urethral orifice opens on the ventral portion of the glans penis or the body of the penis. This is due to a failure of the urogenital folds to fuse correctly. This causes urine to be excreted through this opening instead of the external urethral meatus. Epispadias occurs less commonly and is a result of urethral meatus which is found on the dorsal side of the penis. Epispadia is most commonly associated with bladder exstrophy. Phimosis is when the prepuce fits too tightly over the glans and cannot be retracted. Micropenis is when the penis is 2.5 standard deviations below the mean in length measured along the dorsal surface from the pubis to the tip of the penis stretched. It is thought to be due to insufficient androgen stimulation during the fetal period. Chordee is another congenital anomaly that is fairly common. Chordee is the downward curvature of the head of the penis that occurs during the fetal period. This curvature is most notable during an erection. Some patients with chordee may also have hypospadias, but this is not always the case. Chordee is usually not painful and may be treated with minor surgery.[8][9][10]
Clinical Significance
Erectile dysfunction (ED), the inability to get or maintain an erection, is the most common penile disorder. This can be due to either psychological stress, organic disease, or a combination of both. Risk factors associated with erectile dysfunction include obesity, smoking, atherosclerotic disease, decreased activity, obstructive sleep apnea, diabetes, drugs as well as many other causes. Antidepressants and antihypertensive drugs are common drugs which lead to erectile dysfunction. The most common cause of erectile dysfunction is vascular issues. Thus the first line therapy is usually phosphodiesterase-5 inhibitors, such as sildenafil, vardenafil, and tadalafil. They work by increasing nitric oxide-induced vasodilation by increasing the cyclic guanosine monophosphate (GMP) levels. Phosphodiesterase inhibitors are contraindicated in patients taking nitrates due to vasodilatory effects of both drugs, which can lead to severe hypotension. Lifestyle modifications are usually indicated for the treatment of erectile dysfunction also. Weight loss, physical activity, and smoking cessation can improve erectile function. If initial therapy fails, there are second-line therapies such as vacuum-assisted mechanical devices, penile injections with alprostadil, or penile prosthesis.
Peyronie disease is an abnormal curvature of the penis that is normally a benign condition but may be associated with painful erections or erectile dysfunction. The condition can resolve spontaneously, become stable, or worse. The underlying pathogenesis of Peyronie disease is not known. However, it is believed that repeated microtrauma to the penis leads to fibrin deposition due to microvascular injury. The fibrous plaques contain excessive collagen that causes focal inelasticity leading to the curvature of the penis. Several conditions have been associated with Peyronie disease such as Paget disease and Dupuytren contracture. The diagnosis of Peyronie disease is usually a clinical diagnosis, but imaging may be helpful. Current medical management of oral therapy for Peyronie disease include pentoxifylline, vitamin E, potassium para-aminobenzoate, colchicine, tamoxifen, and carnitine. Pentoxifylline is usually the first-line therapy. Intralesional drug therapy includes verapamil, interferon alfa-2b, and collagenase. Other treatments include penile traction therapy, iontophoresis, extracorporeal shockwave therapy, surgical straightening procedures, penile prosthesis placement, and radiation.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Weech D, Ameer MA, Ashurst JV. Anatomy, Abdomen and Pelvis, Penis Dorsal Nerve. StatPearls. 2024 Jan:(): [PubMed PMID: 30247841]
Othmane Y, Touzani A. [Isolated male epispadias]. The Pan African medical journal. 2017:28():202. doi: 10.11604/pamj.2017.28.202.14220. Epub 2017 Nov 6 [PubMed PMID: 29610640]
Kim S, Dennis M, Holland J, Terrell M, Loukas M, Schober J. The anatomy of abdominal flap phalloplasty for transgender surgery. Clinical anatomy (New York, N.Y.). 2018 Mar:31(2):181-186. doi: 10.1002/ca.23020. Epub 2017 Dec 28 [PubMed PMID: 29178488]
Koifman L, Barros R, Schulze L, Ornellas AA, Favorito LA. Myiasis associated with penile carcinoma: a new trend in developing countries? International braz j urol : official journal of the Brazilian Society of Urology. 2017 Jan-Feb:43(1):73-79. doi: 10.1590/S1677-5538.IBJU.2016.0084. Epub [PubMed PMID: 24893913]
Tu LH, Spektor M, Ferrante M, Mathur M. MRI of the Penis: Indications, Anatomy, and Pathology. Current problems in diagnostic radiology. 2020 Jan-Feb:49(1):54-63. doi: 10.1067/j.cpradiol.2018.12.004. Epub 2018 Dec 11 [PubMed PMID: 30704768]
Lee SH, Ha TJ, Koh KS, Song WC. Ligamentous structures in human glans penis. Journal of anatomy. 2019 Jan:234(1):83-88. doi: 10.1111/joa.12896. Epub 2018 Nov 18 [PubMed PMID: 30450557]
Baskin L, Shen J, Sinclair A, Cao M, Liu X, Liu G, Isaacson D, Overland M, Li Y, Cunha GR. Development of the human penis and clitoris. Differentiation; research in biological diversity. 2018 Sep-Oct:103():74-85. doi: 10.1016/j.diff.2018.08.001. Epub 2018 Aug 23 [PubMed PMID: 30249413]
Alsowayan OS. Management of hypospadias in Saudi Arabia: A national survey. Urology annals. 2018 Oct-Dec:10(4):391-394. doi: 10.4103/UA.UA_88_18. Epub [PubMed PMID: 30386092]
Level 3 (low-level) evidenceLevey HR, Segal RL, Bivalacqua TJ. Management of priapism: an update for clinicians. Therapeutic advances in urology. 2014 Dec:6(6):230-44. doi: 10.1177/1756287214542096. Epub [PubMed PMID: 25435917]
Level 3 (low-level) evidenceFahmy MA, El Shennawy AA, Edress AM. Spectrum of penoscrotal positional anomalies in children. International journal of surgery (London, England). 2014:12(9):983-8. doi: 10.1016/j.ijsu.2014.08.001. Epub 2014 Aug 8 [PubMed PMID: 25110332]
Level 2 (mid-level) evidence