Percutaneous Transluminal Coronary Angioplasty
Percutaneous Transluminal Coronary Angioplasty
Introduction
Percutaneous transluminal coronary angioplasty (PTCA) also called percutaneous coronary intervention (PCI) is a minimally invasive procedure to open blocked or stenosed coronary arteries allowing unobstructed blood flow to the myocardium. The blockages occur because of lipid-rich plaque within the arteries, diminishing blood flow to the myocardium. The accumulation of lipid-rich plaque in the arteries is known as atherosclerosis. When atherosclerosis affects the coronary arteries, the disorder is known as coronary artery disease. Patients with CAD usually present with exertional chest pain, or with dyspnea with exertion. In acute myocardial infarction, there is plaque rupture with platelet aggregation, and acute thrombus formation, which results in a sudden occlusion of the coronary artery. These patients present with acute chest heaviness, diaphoresis, and nausea. Urgent PTCA is often required to limit myocardial damage.
Andreas Gruentzig first developed PCTA in 1977, and the procedure was performed in Zurich, Switzerland that same year.[1] By the mid-1980s many leading institutions adopted this procedure throughout the world as a treatment for coronary artery disease. PTCA is a hallmark procedure and basis of many other intracoronary interventions. It is one of the most common procedures performed in the United States making up 3.6% of all operating room procedures performed in 2011.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
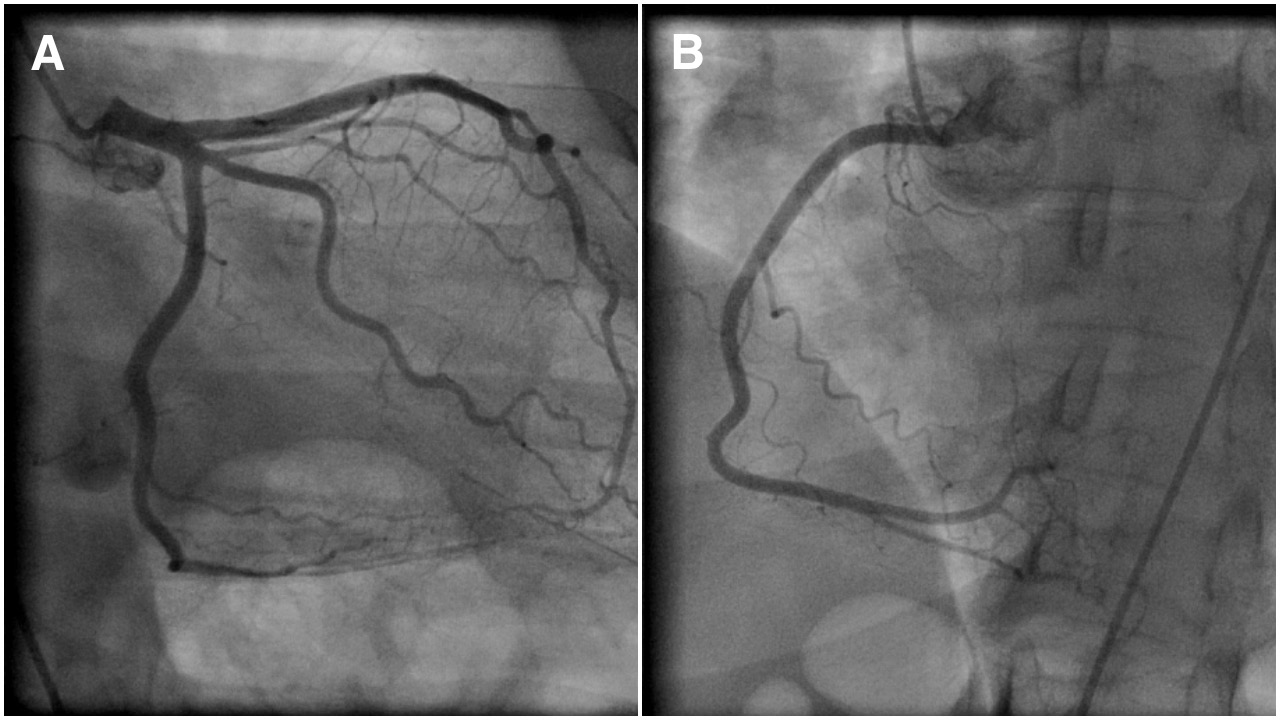
The 2, main coronary arteries supplying the heart are the right and left coronary arteries. The left coronary artery (LCA) divides into left anterior descending (LAD) and left circumflex artery (LCX) branches. LCA supplies blood to the left ventricle of the heart. See Image. Coronary Angiogram Showing Normal Epicardial Left (A) and Right (B) Coronary Arteries. The right coronary artery (RCA) divides into the right posterior descending (PDA) and a (PL) posterolateral branch. RCA supplies blood to the ventricles, right atrium, and sinoatrial node. Coronary arteries are end-arteries supplying the myocardium and blockage can lead to serious adverse effects. Coronary artery disease occurs due to the buildup of plaque within the coronary arteries with subsequent narrowing and blockage reducing blood flow to the myocardium.
Indications
Indications of PTCA depend on various factors. Patients with stable angina symptoms unresponsive to maximal medical therapy will benefit from PCI. It helps provide relief of persistent angina symptoms despite maximal medical therapy.[2] Emergency PTCA is indicated for acute ST-elevation myocardial infarction (STEMI) suggesting 100% occlusion of the coronary artery. With acute STEMI, patients are taken directly to the cath lab immediately upon presentation to help prevent further myocardial muscle damage. In non-ST-elevation myocardial infarction (NSTEMI), or unstable angina, (known as acute coronary syndromes), patients are taken to the cardiac cath lab within 24 to 48 hours.
Contraindications
PTCA has limited contraindications. Patients with left main CAD are poor candidates for the procedure due to the risk of acute obstruction or spasm of the left main coronary artery during the procedure. It is also not recommended for patients with hemodynamically insignificant (less than 70%) stenosis of the coronary arteries.
Equipment
Initially, PCI was performed using balloon catheters alone. However, due to subclinical outcomes and vessel re-stenosis, other devices were introduced including atherectomy devices and coronary stents. Atherectomy devices used alone resulted in poor outcomes. Coronary stents are the most widely used intracoronary devices in PTCA due to improved clinical outcomes. Various types of stents are available including traditional bare-metal stents (BMS) and drug-eluting stents (DES). DES has a polymer coating that prevents inflammation and endothelial cell proliferation. Most recent DES used in the United States use sirolimus, everolimus, and zotarolimus. The newer generation DES have reduced the incidence of late stent thrombosis.[3] The use of antiplatelet therapy is important during the first 12 months after PTCA, allowing appropriate duration for endothelial cell formation over the metallic stent to prevent stent thrombosis.
Personnel
A team made up of an interventional cardiologist, nurse, and radiology technologist performs PTCA. All team members must have specialized and extensive training in the procedure.
Preparation
An interprofessional team evaluates the patients and performs pre-procedural testing to determine candidacy for the procedure. The inquiry related to the past history of allergy to seafood or contrast agents is vital. Important pre-procedure laboratory tests include PT and PTT, serum electrolytes, BUN, and creatinine. The patient is required to be well hydrated. Medication review is essential including cessation of anticoagulants if possible. Also, common medications including NSAIDs, or ACEIs can be held to prevent worsening renal insufficiency. The diabetes medication metformin is held prior to cardiac catheterization to avoid worsening renal insufficiency and lactic acidosis. Fluids and food are restricted 6 to 8 hours before the procedure. When cases are performed via radial artery access, patients are often given intra-arterial calcium channel blocker, nitroglycerin, and heparin to prevent vasospasm. The health care provider should thoroughly explain the procedure and its associated risks and complications to the patient to obtain a signed informed consent.
Technique or Treatment
The procedure is performed under local anesthesia. Conscious sedation is routinely given to avoid stress and calm the patient. The most commonly used approach is the percutaneous femoral (Judkins) approach. Once the patient is anesthetized with a superficial injection of lidocaine to the skin, and subcutaneous tissues over the right femoral artery, a needle is inserted into the femoral artery (percutaneous access). Successful insertion of the needle is followed by insertion of a guidewire through the needle into the lumen of the blood vessel. The needle is then removed with the guidewire remaining in the vessel lumen. A sheath with an introducer is placed over the guidewire and into the femoral artery. Next, the guidewire and introducer is removed, leaving the sheath in the vessel lumen. This provides easy access to the femoral artery lumen. Next, a long narrow tube, known as the "diagnostic catheter," is advanced through the sheath with a long guidewire in the catheter lumen. The diagnostic catheter follows the guidewire and is passed retrograde through the femoral artery, iliac artery, descending aorta, over the aortic arch to the proximal ascending aorta. The guidewire is removed leaving the tip of the diagnostic catheter in the ascending aorta. The diagnostic catheter is attached to a manifold with a syringe. The manifold allows the ability to inject contrast, check inter-arterial pressure, and administer medications.
The diagnostic catheter is then manipulated into the ostium of the left main coronary artery, or right coronary artery. Contrast dye is injected, and cineangiography images are obtained in multiple views of both arteries. If severe stenosis exists in one of the arteries, PTCA can be performed. The diagnostic catheter is removed and exchanged for a similar guide catheter. Guide catheters have a larger luminal diameter for ease of passage of wires and balloons during angioplasty. After the guide catheter is placed in the ostium of the respective artery, a PTCA guidewire is advanced through the catheter and across the stenosis. Once the PTCA guidewire is passed across the stenosis, it is left in place until the end of the procedure. A balloon wire can be placed over the PTCA guidewire and advanced until the balloon is directly over the stenosis. The cardiologist controls the direction and movement of the PTCA guidewire, and balloon wire by twisting the part of guide wires that sit outside the patient. The balloon is then inflated and deflated repeatedly until the artery is patent. In most instances, a stent is required. The balloon wire is removed and exchanged for a stent. A stent is a latticed metal scaffold that is delivered crimped over a balloon of a balloon wire. The stent is then placed in the position of the stenosis, and the balloon is expanded. Once the stent is expanded, it cannot be removed from the artery. The balloon is deflated, and the stent remains in place. The stent can maintain long-term patency. Repeated injections of contrast media are utilized to check for patency of the artery.
Upon successful insertion of the stent and expansion of the vessel, the balloon wire is removed. Lastly, the PTCA guidewire is removed. During the procedure, anticoagulation is administered to prevent the formation of clots. The entire procedure can take from 30 minutes to 3 hours depending upon the technical difficulties of the case.
Complications
PTCA is widely practiced and has risks, but major procedural complications are rare. The mortality rate during angioplasty is 1.2%.[4] People older than the age of 65, with kidney disease or diabetes, women, and those with massive heart disease are at a higher risk for complications. Possible complications include hematoma at the femoral artery insertion site, pseudoaneurysm of the femoral artery, infection of skin over femoral artery, embolism, stroke, kidney injury from contrast dye, hypersensitivity to dye, vessel rupture, coronary artery dissection, bleeding, vasospasm, thrombus formation, and acute MI. There is a long-term risk of re-stenosis of the stented vessel.
Clinical Significance
PTCA is performed under local anesthesia and serves as an alternative to coronary artery bypass surgery (CABG). In comparison to CABG, PTCA is associated with lower morbidity and mortality, shorter convalescence, and lower cost. It can significantly improve blood flow through the coronary arteries in about 90% of patients with relief of anginal symptoms and improvement in exercise capacity. It effectively eliminates arterial narrowing in most cases. Different modeling studies presented different conclusions regarding the cost-effectiveness of PTCA and CABG in patients with myocardial ischemia that do not respond to medical therapy.[5][6][7]
Enhancing Healthcare Team Outcomes
PTCA is not an easy procedure, and despite the advances in technology, it has risks and complications. All patients need to be educated about the procedure and its potential complications. Maintaining a healthy diet, exercising, and reducing stress are important post-procedural measures to reduce the risk of recurrences and complications. The heart team illustrates an excellent example of patient-centered care. Experts from different fields of medicine come together to provide the best solution for each patient.[8]
Media
(Click Image to Enlarge)
References
Meier B, Bachmann D, Lüscher T. 25 years of coronary angioplasty: almost a fairy tale. Lancet (London, England). 2003 Feb 8:361(9356):527 [PubMed PMID: 12583964]
Level 3 (low-level) evidencePursnani S, Korley F, Gopaul R, Kanade P, Chandra N, Shaw RE, Bangalore S. Percutaneous coronary intervention versus optimal medical therapy in stable coronary artery disease: a systematic review and meta-analysis of randomized clinical trials. Circulation. Cardiovascular interventions. 2012 Aug 1:5(4):476-90. doi: 10.1161/CIRCINTERVENTIONS.112.970954. Epub 2012 Aug 7 [PubMed PMID: 22872053]
Level 1 (high-level) evidencePalmerini T, Benedetto U, Biondi-Zoccai G, Della Riva D, Bacchi-Reggiani L, Smits PC, Vlachojannis GJ, Jensen LO, Christiansen EH, Berencsi K, Valgimigli M, Orlandi C, Petrou M, Rapezzi C, Stone GW. Long-Term Safety of Drug-Eluting and Bare-Metal Stents: Evidence From a Comprehensive Network Meta-Analysis. Journal of the American College of Cardiology. 2015 Jun 16:65(23):2496-507. doi: 10.1016/j.jacc.2015.04.017. Epub [PubMed PMID: 26065988]
Level 1 (high-level) evidenceMovahed MR, Hashemzadeh M, Jamal MM, Ramaraj R. Decreasing in-hospital mortality of patients undergoing percutaneous coronary intervention with persistent higher mortality rates in women and minorities in the United States. The Journal of invasive cardiology. 2010 Feb:22(2):58-60 [PubMed PMID: 20124588]
Level 2 (mid-level) evidenceStroupe KT,Morrison DA,Hlatky MA,Barnett PG,Cao L,Lyttle C,Hynes DM,Henderson WG, Cost-effectiveness of coronary artery bypass grafts versus percutaneous coronary intervention for revascularization of high-risk patients. Circulation. 2006 Sep 19 [PubMed PMID: 16966588]
Level 1 (high-level) evidenceOsnabrugge RL, Magnuson EA, Serruys PW, Campos CM, Wang K, van Klaveren D, Farooq V, Abdallah MS, Li H, Vilain KA, Steyerberg EW, Morice MC, Dawkins KD, Mohr FW, Kappetein AP, Cohen DJ, SYNTAX trial investigators. Cost-effectiveness of percutaneous coronary intervention versus bypass surgery from a Dutch perspective. Heart (British Cardiac Society). 2015 Dec:101(24):1980-8. doi: 10.1136/heartjnl-2015-307578. Epub 2015 Nov 9 [PubMed PMID: 26552756]
Level 3 (low-level) evidenceZhang Z, Kolm P, Grau-Sepulveda MV, Ponirakis A, O'Brien SM, Klein LW, Shaw RE, McKay C, Shahian DM, Grover FL, Mayer JE, Garratt KN, Hlatky M, Edwards FH, Weintraub WS. Cost-effectiveness of revascularization strategies: the ASCERT study. Journal of the American College of Cardiology. 2015 Jan 6:65(1):1-11. doi: 10.1016/j.jacc.2014.09.078. Epub [PubMed PMID: 25572503]
Level 2 (mid-level) evidenceWelsh RC, Granger CB, Westerhout CM, Blankenship JC, Holmes DR Jr, O'Neill WW, Hamm CW, Van de Werf F, Armstrong PW, APEX AMI Investigators. Prior coronary artery bypass graft patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. JACC. Cardiovascular interventions. 2010 Mar:3(3):343-51. doi: 10.1016/j.jcin.2009.12.008. Epub [PubMed PMID: 20298996]
Level 1 (high-level) evidence