Introduction
The normal pericardium is 1 to 2 mm thick and is comprised of an outer fibrous layer and an inner serous layer (which further subdivides into a visceral layer, or epicardium, and a parietal layer). A potential space that contains approximately 15 to 35 ml of lubrication fluid separates the visceral and parietal layers. The pericardium is a rigid, avascular, fibrous sac and its primary function is minor anchoring, lubrication, preventing distention of cardiac chambers, and optimizing diastolic filling.[1] Normally the pericardium lacks any calcium deposits, and calcification may be a sign of underlying inflammation or a more sinister etiology. Pericardial calcification is a radiological finding most often discovered while performing chest computed tomography (CT).[2]
Often pericardial calcification is an incidental finding noted during chest or cardiac CT and as such remains asymptomatic. However, signs and symptoms associated with pericardial calcification usually develop secondary to constrictive physiology caused by the rigid pericardium. However, a significant point to keep in mind is that pericardial calcification may not be present in up to 20% of cases of constrictive pericarditis (CP), and it may be present in the absence of constrictive physiology. Interestingly, there have been recent reports of the development of CP after cardiac transplantation, an unusual presentation, as the transplanted heart is believed to be free of any pericardial tissue.[3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pericardial calcification is the sequelae of inflammation, fibrosis, and necrosis. The most common etiologies of such inflammation include viral infections, chest radiation exposure, and following cardiac surgery.[5] Historically, tuberculosis had been a significant cause of CP in the US and accounted for almost half of the cases, but now it is found more commonly in developing nations.[2] Other known etiologies include uremic pericarditis, trauma, malignancy, rheumatologic and connective tissue diseases.[5] Pericardial calcification has also been reported following asbestos exposure.[6] Despite these known associations, however, more than 50% of cases of pericardial calcification are thought to be idiopathic.[7]
Epidemiology
Given that pericardial calcification can be an asymptomatic incidental finding, its true prevalence is unknown. However, it is found to be more likely to occur following trauma, purulent pericarditis, and when acute pericarditis or pericardial effusions are associated with malignancy and connective tissue diseases.[8]
For idiopathic and viral constrictive pericarditis, an incidence of 0.76 cases per 1000 person-years has been reported in a series of 500 consecutive patients; this contrasts with the connective tissue disease, neoplasms, tuberculosis, and purulent CP in which the incidence was noted to be 4.40, 6.33, 31.65, and 52.74 cases per 1000 person-years, respectively.[9]
Tuberculous pericarditis, caused by Mycobacterium tuberculosis, is found in approximately 1% of all autopsied cases of TB and 1 to 2% of instances of pulmonary TB. Most constrictive tuberculosis caused by TB is subacute so calcifications of the pericardium are rare.[10]
A study by Ling et al. suggests that calcified CP is more common in males.[6]
Pathophysiology
Varying degrees of pericardial calcification are present in about 80 to 98% of the cases of CP.[2][6] These changes typically occur over a period of months to years after the initial insult. Pericardial calcification in CP may or may not be associated with pericardial thickening, and about 18% of CP cases have no pericardial thickening.[8] Constrictive pericarditis occurs when a normal thin compliant pericardium is replaced by a thick, calcified, non-compliant pericardium that interferes with ventricular filling, which in turn lowers cardiac output.[6]
History and Physical
Pericardial calcification is generally asymptomatic; symptoms usually develop with cardiac hemodynamic compromise such as in the setting of constrictive pericarditis. Symptoms of right heart failure or low output states such as dyspnea on exertion, orthopnea, bendopnea, and fatigue may develop. Of these, exertional dyspnea and lower extremity edema are the most common findings.[11] Physical examination findings include hepatomegaly, ascites, peripheral edema (usually bilateral), hepatojugular reflux, Kussmaul’s sign, jugular venous distention (with prominent x and y descents), and pulsus paradoxus. In advanced disease, there can be cachexia.[8] Atrial arrhythmias namely atrial fibrillation and flutter have been noted to be more common in CP with pericardial calcification. [6]
Evaluation
Pericardial calcification is an anatomical finding with significance in the presence of constrictive physiology. This is why imaging for the same is two-pronged, involving the identification of calcification in the pericardium and hemodynamic consequences of the same.[12] Chest radiography may identify pericardial calcification; however, it suffers from low sensitivity. The laboratory workup may show an elevation of liver enzymes (especially alkaline phosphatase) and serum creatinine. In addition, B-type natriuretic peptide and N terminal pro-brain natriuretic peptide are frequently used to differentiate CP from restrictive cardiomyopathy.[13]
CT provides excellent anatomic details of the heart and the pericardium. The normal pericardial thickness on the CT scan should be less than 2 mm.[14] Although the pericardial thickness of more than 4 mm on CT scan is predictive of constrictive pericarditis, up to 20% of patients with normal pericardial thickness can have evidence of pericardial calcification and develop CP.[15] In a cohort of patients with CP and pericardial calcification, calcification was noted to more commonly involve the diaphragmatic and anterior portions of the pericardium, with apical and left atrial involvement being found less commonly.[6] However, CT suffers from lower temporal resolution compared to echocardiography and cardiac magnetic resonance imaging (MRI) and cannot reliably demonstrate constrictive physiology.[16] In addition, pericardial calcification has also been demonstrated on 99m Tc-methylene diphosphonate bone scintigraphy, which can be another useful imaging option to help visualize pericardial calcification where CT imaging may be challenging.[17]
To evaluate the functional significance of pericardial calcification, two-dimensional (2-D) echocardiography and tissue Doppler imaging are probably the essential tools for diagnosing CP. 2-D echocardiography demonstrates septal motion abnormalities, enhanced interventricular interdependence, and plethoric inferior vena cava. Tissue Doppler of the mitral annulus reveals increased medial early diastolic velocities (e').[7] In healthy individuals, mitral lateral e' velocity is usually greater than the medial e' velocity, but in CP, due to the tethering effect of the lateral annulus to the surrounding calcified pericardium, this velocity becomes lower, a phenomenon called 'annulus reversus' and a hallmark feature of CP.[7] Cardiac MRI can be utilized not only to delineate cardiac anatomy and pericardial thickness, but it can also provide information on ventricular septal motion demonstrating the so-called 'septal bounce' and 'septal shudder.'[7]
While cardiac MRI is not as sensitive as CT in identifying pericardial calcification, it is a useful tool in assessing the extent of edema and scarring, which helps understand the progression of the disease and predict which patients are more likely to develop CP.[18] An invasive hemodynamic assessment with cardiac catheterization is possible in some cases where the diagnosis is unclear. Typically, an equalization of end-diastolic pressures in all four cardiac chambers is noted. Furthermore, with the 'match-up' study, by placing high fidelity catheters in the right and left ventricle and recording pressures simultaneously, discordant respirophasic changes in the ventricular filling patterns are noted (a catheterization equivalent of ventricular interdependence, in which one ventricle fills at the expense of the other depending on the respiratory cycle.[19]
In the past, an endomyocardial biopsy was also used to differentiate CP from restrictive cardiomyopathy, although it was found to have a low yield.[8]
Treatment / Management
Pericardial calcification in the absence of symptoms does not require any treatment. Subacute cases of constrictive pericarditis with underlying inflammation may respond to anti-inflammatory therapy (such as colchicine, corticosteroids, and non-steroidal anti-inflammatory drugs).[4][20] However, anti-inflammatory agents are usually unable to reverse fibrosis and calcification but are mainly meant to decrease the progression of inflammation and further scarring. Cardiac MRI can often help concurrently visualize scar and edema to determine which patients are more likely to benefit from anti-inflammatory therapy.[21]
Diuretics have been used in the early stages of constrictive pericarditis to improve pulmonary and systemic congestion. These must be used cautiously because any drop in intravascular volume may cause a corresponding drop in cardiac output.[22] Surgical pericardiectomy is the gold standard for CP and is potentially curative.[20] Pericardiectomy usually has a high success rate (70-80%) but also has a high perioperative mortality rate of 5 to 10%. Perioperative cardiovascular outcomes are usually influenced by New York Heart Association heart failure class, with NYHA Class I and II heart failure patients having better postoperative outcomes than NYHA Class III and IV heart failure. The presence and extent of pericardial calcification usually do not affect perioperative outcomes.[23]
Differential Diagnosis
Constrictive pericarditis must be ruled out when pericardial calcification is present on imaging modalities. Unusual forms of CP such as transient constriction (which responds to anti-inflammatory therapy) and effusive constrictive pericarditis (developing in patients with cardiac tamponade and developing immediately after pericardiocentesis), or occult constrictive pericarditis (which manifests after a fluid challenge) must be ruled out as well [7]. Other differentials of calcification of pericardium include pericardial scarring due to recurrent pericarditis. Additionally, mimickers of CP include restrictive cardiomyopathy (which occurs due to abnormal myocardium), and severe tricuspid regurgitation must be ruled out.[8]
Prognosis
The presence of pericardial calcification and its extent by itself does not affect prognosis. Patients with poor cardiovascular outcomes after pericardectomy were those that developed long-term sequelae of constrictive physiology, including myocardial atrophy, or had concurrent cardiomyopathy. Prognosis is worse for patients diagnosed with NYHA Class III and IV heart failure as they have higher operative mortality.[23]
Long-term survival after pericardiectomy for constrictive pericarditis depends on the underlying etiology. In a cohort of 163 patients, idiopathic CP had the best 7-year survival (88%), followed by postsurgical (66%) and post-radiation CP (27%).[24] Patients with advanced age, prior radiation exposure, pulmonary hypertension, renal dysfunction, and liver failure also had poor outcomes despite pericardectomy.[8][25]
Complications
Pericardial calcification in the presence of symptoms should be evaluated further as constrictive pericarditis, if present, could be potentially curative. Without surgical pericardiectomy, constrictive pericarditis portends a very poor prognosis due to complications associated with heart failure and the low output state. Renal failure, organomegaly, shock, and death are other potential complications.[23]
Deterrence and Patient Education
Early recognition and diagnosis of pericardial calcification and ruling out constrictive pericarditis is imperative to ensure timely management and optimal clinical outcomes. This diagnosis is often an incidental finding. The increased use of cardiac CT for calcium scoring has led to the detection of pericardial calcifications in many asymptomatic patients.
Enhancing Healthcare Team Outcomes
Pericardial calcification in the absence of symptoms is a benign condition. However, constrictive pericarditis must be ruled out in such patients. Diagnosis of CP can be challenging and requires multimodal imaging with an interprofessional approach involving invasive and non-invasive cardiologists, radiologists, and cardiothoracic surgeons. The condition is often identified by primary care and emergency providers. CP carries a grave prognosis if missed, and most patients die with medical management alone. Pericardiectomy is potentially curative and carries acceptable mid and long-term outcomes depending on the etiology. Coordination of evaluation by the team will lead to improved outcomes. [Level 5]
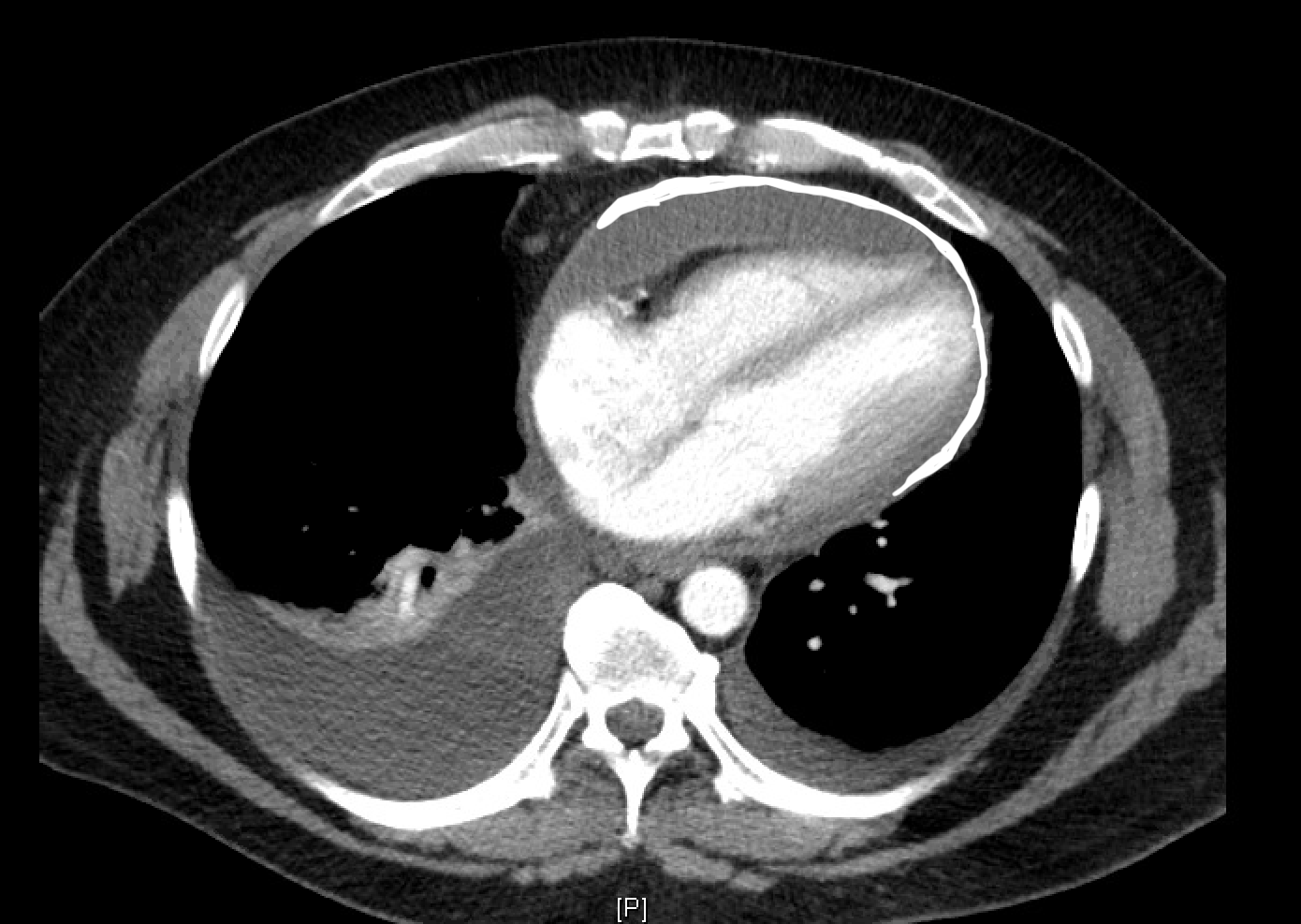
Media
(Click Image to Enlarge)
References
Watkins MW,LeWinter MM, Physiologic role of the normal pericardium. Annual review of medicine. 1993; [PubMed PMID: 8476238]
Level 3 (low-level) evidenceNguyen T,Phillips C,Movahed A, Incidental findings of pericardial calcification. World journal of clinical cases. 2014 Sep 16; [PubMed PMID: 25232549]
Level 3 (low-level) evidenceUmer A,Khalid N,Chhabra L,Spodick DH, Role of Pericardiectomy in Postcardiac Transplant Constrictive Pericarditis. The Annals of thoracic surgery. 2015 Dec; [PubMed PMID: 26652564]
Umer A,Khalid N,Chhabra L,Memon S,Spodick DH, Constrictive pericarditis complicating cardiac transplantation. Journal of cardiothoracic surgery. 2015 Aug 25; [PubMed PMID: 26302865]
Cameron J,Oesterle SN,Baldwin JC,Hancock EW, The etiologic spectrum of constrictive pericarditis. American heart journal. 1987 Feb; [PubMed PMID: 3812191]
Level 2 (mid-level) evidenceLing LH,Oh JK,Breen JF,Schaff HV,Danielson GK,Mahoney DW,Seward JB,Tajik AJ, Calcific constrictive pericarditis: is it still with us? Annals of internal medicine. 2000 Mar 21; [PubMed PMID: 10733443]
Level 2 (mid-level) evidenceMiranda WR,Oh JK, Constrictive Pericarditis: A Practical Clinical Approach. Progress in cardiovascular diseases. 2017 Jan - Feb; [PubMed PMID: 28062267]
Welch TD,Oh JK, Constrictive Pericarditis. Cardiology clinics. 2017 Nov; [PubMed PMID: 29025545]
Imazio M,Brucato A,Maestroni S,Cumetti D,Belli R,Trinchero R,Adler Y, Risk of constrictive pericarditis after acute pericarditis. Circulation. 2011 Sep 13; [PubMed PMID: 21844077]
Level 2 (mid-level) evidenceStrang JI,Kakaza HH,Gibson DG,Girling DJ,Nunn AJ,Fox W, Controlled trial of prednisolone as adjuvant in treatment of tuberculous constrictive pericarditis in Transkei. Lancet (London, England). 1987 Dec 19; [PubMed PMID: 2891992]
Level 1 (high-level) evidenceLing LH,Oh JK,Schaff HV,Danielson GK,Mahoney DW,Seward JB,Tajik AJ, Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy. Circulation. 1999 Sep 28; [PubMed PMID: 10500037]
Kim JS,Kim HH,Yoon Y, Imaging of pericardial diseases. Clinical radiology. 2007 Jul [PubMed PMID: 17556030]
Diaz-Arocutipa C,Saucedo-Chinchay J,Imazio M,Argulian E, Natriuretic peptides to differentiate constrictive pericarditis and restrictive cardiomyopathy: A systematic review and meta-analysis. Clinical cardiology. 2021 Dec 30 [PubMed PMID: 34967020]
Level 1 (high-level) evidenceBull RK,Edwards PD,Dixon AK, CT dimensions of the normal pericardium. The British journal of radiology. 1998 Sep; [PubMed PMID: 10195005]
Talreja DR,Edwards WD,Danielson GK,Schaff HV,Tajik AJ,Tazelaar HD,Breen JF,Oh JK, Constrictive pericarditis in 26 patients with histologically normal pericardial thickness. Circulation. 2003 Oct 14; [PubMed PMID: 14517161]
Level 2 (mid-level) evidenceWang ZJ,Reddy GP,Gotway MB,Yeh BM,Hetts SW,Higgins CB, CT and MR imaging of pericardial disease. Radiographics : a review publication of the Radiological Society of North America, Inc. 2003 Oct [PubMed PMID: 14557510]
Burns N,Shriki JE,Farvid AM,El-Sherief KE,Cunningham MJ,Colletti PM,Shinbane J, Calcific constrictive pericarditis demonstrated on 99mTc-MDP bone scintigraphy. Journal of radiology case reports. 2009; [PubMed PMID: 22470658]
Level 3 (low-level) evidenceAl-Mallah MH,Almasoudi F,Ebid M,Ahmed AM,Jamiel A, Multimodality Imaging of Pericardial Diseases. Current treatment options in cardiovascular medicine. 2017 Oct 12; [PubMed PMID: 29027095]
Talreja DR,Nishimura RA,Oh JK,Holmes DR, Constrictive pericarditis in the modern era: novel criteria for diagnosis in the cardiac catheterization laboratory. Journal of the American College of Cardiology. 2008 Jan 22; [PubMed PMID: 18206742]
Haley JH,Tajik AJ,Danielson GK,Schaff HV,Mulvagh SL,Oh JK, Transient constrictive pericarditis: causes and natural history. Journal of the American College of Cardiology. 2004 Jan 21; [PubMed PMID: 14736448]
Chang SA, Oh JK. Constrictive Pericarditis: A Medical or Surgical Disease? Journal of cardiovascular imaging. 2019 Jul:27(3):178-186. doi: 10.4250/jcvi.2019.27.e28. Epub 2019 Apr 30 [PubMed PMID: 31161752]
Inglessis I I,Dec GW, Constrictive Pericarditis. Current treatment options in cardiovascular medicine. 1999 Jun [PubMed PMID: 11096470]
Depboylu BC,Mootoosamy P,Vistarini N,Testuz A,El-Hamamsy I,Cikirikcioglu M, Surgical Treatment of Constrictive Pericarditis. Texas Heart Institute journal. 2017 Apr [PubMed PMID: 28461794]
Bertog SC,Thambidorai SK,Parakh K,Schoenhagen P,Ozduran V,Houghtaling PL,Lytle BW,Blackstone EH,Lauer MS,Klein AL, Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. Journal of the American College of Cardiology. 2004 Apr 21; [PubMed PMID: 15093882]
Goland S,Caspi A,Malnick SD, Idiopathic chronic pericardial effusion. The New England journal of medicine. 2000 May 11; [PubMed PMID: 10809614]
Level 3 (low-level) evidence