Introduction
Recent advances in various surgical techniques and the development of more minimally invasive procedures have spurred an increase in outpatient procedures. With these developments, it requires that analgesic techniques keep pace with these surgical advancements. Studies have shown that peripheral nerve blocks are usually well-tolerated and provide regional analgesia superior to other modalities such as oral pain medications or general anesthesia.[1][2][3]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Anatomy and landmarks depend on the type of block being performed. Please refer below to techniques for specifics to the more common peripheral nerve blocks performed.
Indications
There is no strict set of guidelines for the use of peripheral nerve blocks. However, the general rationale is to implement regional blocks in cases where conservative measures have failed or to avoid the side effects and complications of general anesthesia and oral medications. The following include examples of where peripheral nerve blocks may be preferable:
- Patients who are at high risk of respiratory depression related to general anesthesia
- Patients who want to avoid systematic medications
- Patients intolerant or not responsive to oral medications
Contraindications
Absolute contraindications to the use of peripheral nerve blocks include allergy to local anesthetics, inability to cooperate, or patient refusal. It is advised to postpone or reconsider a nerve injection when there is an active infection at the injection site, pre-existing neural deficits along with the distribution of the block, and in patients with coagulopathies or on antithrombotic drugs.
Equipment
Equipment that is used is dependent upon the type of technique utilized. The following is a list of equipment used based on technique.
- Nerve stimulator guidance: peripheral nerve stimulator that delivers an adjustable electrical current to the tip of a hollow insulated disposable needle. The needle has specific tubing attached to a syringe that allows for aspiration and injection of a local anesthetic. A wire runs between the needle and an electrode and allows the electrical pulse to be transmitted to stimulate the nerve.
- Ultrasound guidance: portable ultrasound machines with both high and low-frequency probes that can identify superficial and deeper nerves
- Continuous catheter: numerous kits available, which usually contain a needle and catheter. A standard epidural kit can often be utilized.
Personnel
A well-versed medical professional that is highly familiar and experienced with the type of block being performed should be performing the specific injection.
Preparation
Taking a detailed medical history is necessary to determine conditions like coagulopathy or respiratory compromise that may impact the decision to perform a block. A thorough physical exam is prudent as well to determine preexisting sensory or motor deficits in the distribution of the block. Studies show that patients with preexisting sensory or motor deficits may be more likely to develop new deficits following a block than patients without preexisting deficits. Following the history and physical, the patient should be made familiar with the risks, benefits, and care needed during the recovery phase of the block.
For patients that are receiving a nerve block for a surgical procedure, they should follow the same fasting guidelines for the surgery as it may be necessary for deep sedation to be used in cases of an inadequate block. Also, intravenous access should be obtained due to the risk of potential complications like vasovagal events, local anesthetic toxicity, and the possible use of general anesthetics.
Technique or Treatment
The technique for peripheral nerve blocks is based on the type of block. A quick summary of some of the more common blocks is listed below.
- Interscalene block: anesthetizes nerve roots from the cervical plexus (C3, C4, supraclavicular nerve) and upper and middle trunks of the brachial plexus (C5-C7). For positioning, the patient is placed in a supine position with the head turned away from the side of the block. Sternal notch, the sternal and clavicular heads of the sternocleidomastoid muscle, and clavicle are identified and marked. A probe is placed in a transverse position with its long axis across the neck just above the clavicle if using ultrasound. The carotid artery and internal jugular vein are visualized. The subclavian artery is identified by directing the beam towards the first rib. Nerves are then traced to cephalad. At the C6 nerves of the brachial plexus are visualized in a vertical orientation within the interscalene groove. A needle is then placed in-plane or out-of-plane and directed toward the nerves. A needle tip is placed next to the nerve roots. A total of 12 cc to 30 cc of local anesthetic is injected.
- Supraclavicular block: the patient is placed in the supine position with arms by the sides and the head turned away from the side of the block. The probe is placed in a transverse position just above the clavicle using ultrasound. The carotid artery and internal jugular vein are visualized. The needle is inserted in-plane (parallel to the probe), and a local anesthetic is injected to hydro dissect between the nerves until the tip reaches an area bordered by the first rib, subclavian artery, and brachial plexus. 20 cc to 30 cc of local anesthetic is injected. Before injection, however, aspiration should be performed to ensure there is no blood.
- Infraclavicular block: the patient is placed in the supine position with the head turned away from the side of the block. The arm is abducted with the elbow flexed to identify the coracoid process. The axillary artery is identified, and the cords of the brachial plexus are visualized adjacent to the artery using ultrasound. The needle is placed adjacent to the axillary artery in the cranio-posterior quadrant, and 30 to 40 cc of local anesthetic is administered. Before injection, however, aspiration should be performed to ensure there is no blood
- Axillary block: block anesthetizes nerves of the brachial plexus at the level of the individual nerves and often requires multiple injections. The patient is positioned supine with the arm abducted 90 degrees, and the elbow is flexed. The transducer is placed transversely in the axilla using ultrasound. The needle is introduced perpendicular to the skin and advanced until the tip is next to each nerve.
- Intercostobrachial block: the patient is positioned supine with the arm abducted to expose the axillary fossa. The intercostobrachial nerve runs in the subcutaneous tissue of the medial upper arm. The needle is advanced subcutaneously across the medial aspect of the arm while injecting 5 cc to 10 cc of local anesthetic.
- Radial nerve block: radial nerve emerges between the brachioradialis tendon and the radius, just proximal to the styloid process. The needle is inserted subcutaneously, just proximal to the styloid process of the radius, aiming medially, and 3 cc to 5cc of local anesthetic is injected.
- The median nerve block is located between the tendons of the flexor palmaris longus and the flexor carpi radialis. The need is inserted between the two tendons until it penetrates the fascia and advanced until contact is made with bone. The needle should be redirected and local anesthetic injected in lateral and medial directions.
- Ulnar nerve block: ulnar nerve runs between the ulnar artery and flexor carpi ulnaris tendon. The tendon is just superficial to the ulnar nerve. A needle is placed under the tendon close to its attachment just above the styloid process of the ulna and advanced 5 mm to 10 mm, and 3 cc to 5 cc of local anesthetic is injected at this location.
- Lumbar plexus block: The patient is placed in the lateral decubitus position operative side up with the leg flexed at the hip and knee. It is placed longitudinally adjacent to the spine at the second to third lumbar level using the ultrasound probe. The needle is inserted at the cephalad edge using the in-plane technique. The length of the needle should be seen as it approaches the target structure, which is the posterior third of the psoas major muscle.
- Femoral nerve block: The patient is placed in a supine position. Using ultrasound, the nerve is visualized, which is lateral to the artery. An in-plane or out-of-plane approach can be used where the needle is inserted, and the tip is placed adjacent to the nerve, and 20 cc to 50 cc of local anesthetic is injected in 5 cc increments. Before injection, however, aspiration should be performed to ensure there is no blood.
- Fascia iliaca block: the patient is placed in a supine position where using ultrasound, the probe is placed transversely to the leg at the junction of the middle and lateral thirds (between the ASIS and pubic tubercle) to identify the fascia lata, iliacus muscle, and fascia iliaca. The needle is introduced in-plane inferior to the inguinal ligament and guided beneath the fascia iliaca, and 30 cc of local anesthetic is injected in 5 cc increments. Before injection, however, aspiration should be performed to ensure there is no blood.
- Obturator nerve block: the patient is placed in the supine position with the leg externally rotated. Using an ultrasound probe, it is placed in the inguinal crease, and the femoral vein is identified. The probe is then moved medially to visualize the pectineus and adductor longus muscles. The needle is inserted in-plane or out of plane and is directed to the fascial plane between the adductor brevis and magnus, and 5 cc to 10 cc of local anesthetic is injected. Before injection, however, aspiration should be performed to ensure there is no blood.
- Sciatic nerve block: can be approached anteriorly or posteriorly. The patient is placed in the lateral decubitus position with the hip flexed at 45 degrees and the knee at 90 degrees for the posterior approach. In the anterior approach, the patient is positioned in the same manner. Using an ultrasound probe, it is held transverse to the course of the nerve. The nerve is found lateral to the ischial tuberosity and deep to the gluteus maximus muscle. The needle is inserted in-plane from the lateral aspect of the transducer and positioned with the tip of the needle adjacent to the nerve. Approximately 20 cc of local anesthetic is injected in 5 cc increments with gentle aspirations between injections. Before injection, however, aspiration should be performed to ensure there is no blood.
- Popliteal nerve block: the patient can be placed in either prone, lateral decubitus or supine. There are two approaches. For the posterior approach, the biceps femoris and semitendinosus/semimembranosus tendons are palpated. The ultrasound probe is placed transverse to the thigh and in the popliteal crease. The popliteal artery is used as the landmark, and the tibial nerve is found superficial and lateral to the popliteal artery. The nerve is then followed cephalad to the point where the common fibular nerve joins the tibial nerve from the lateral side to form the sciatic nerve. The sciatic nerve is blocked proximal to this to ensure that both the common fibular and tibial nerves are anesthetized.
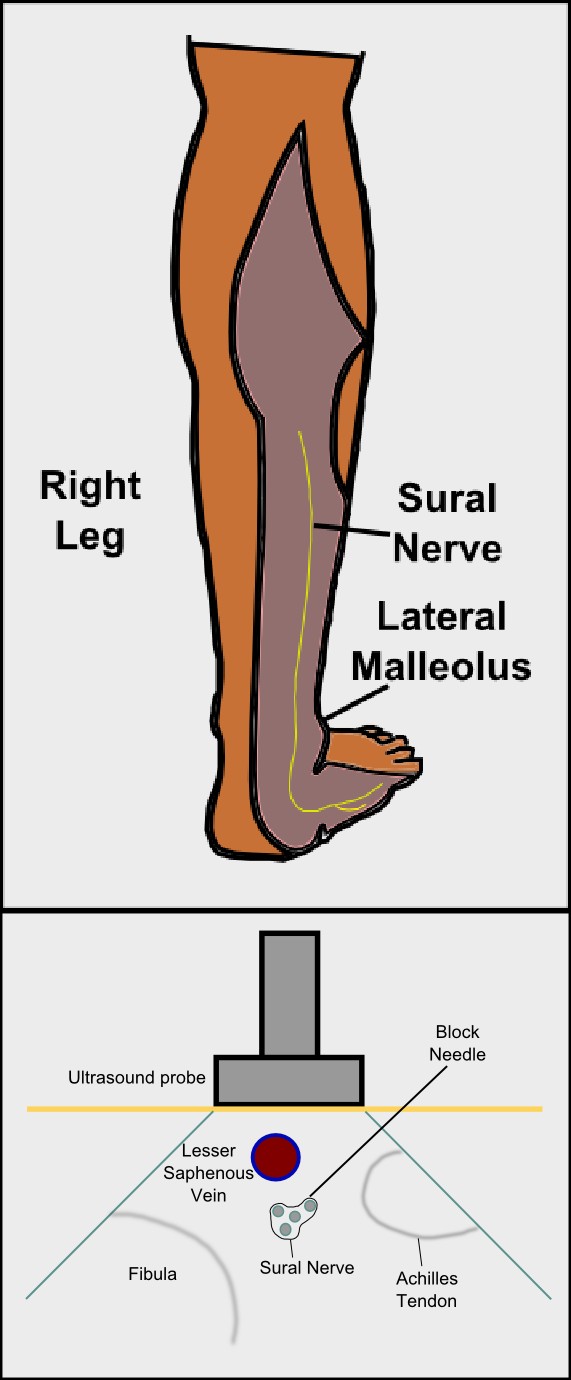
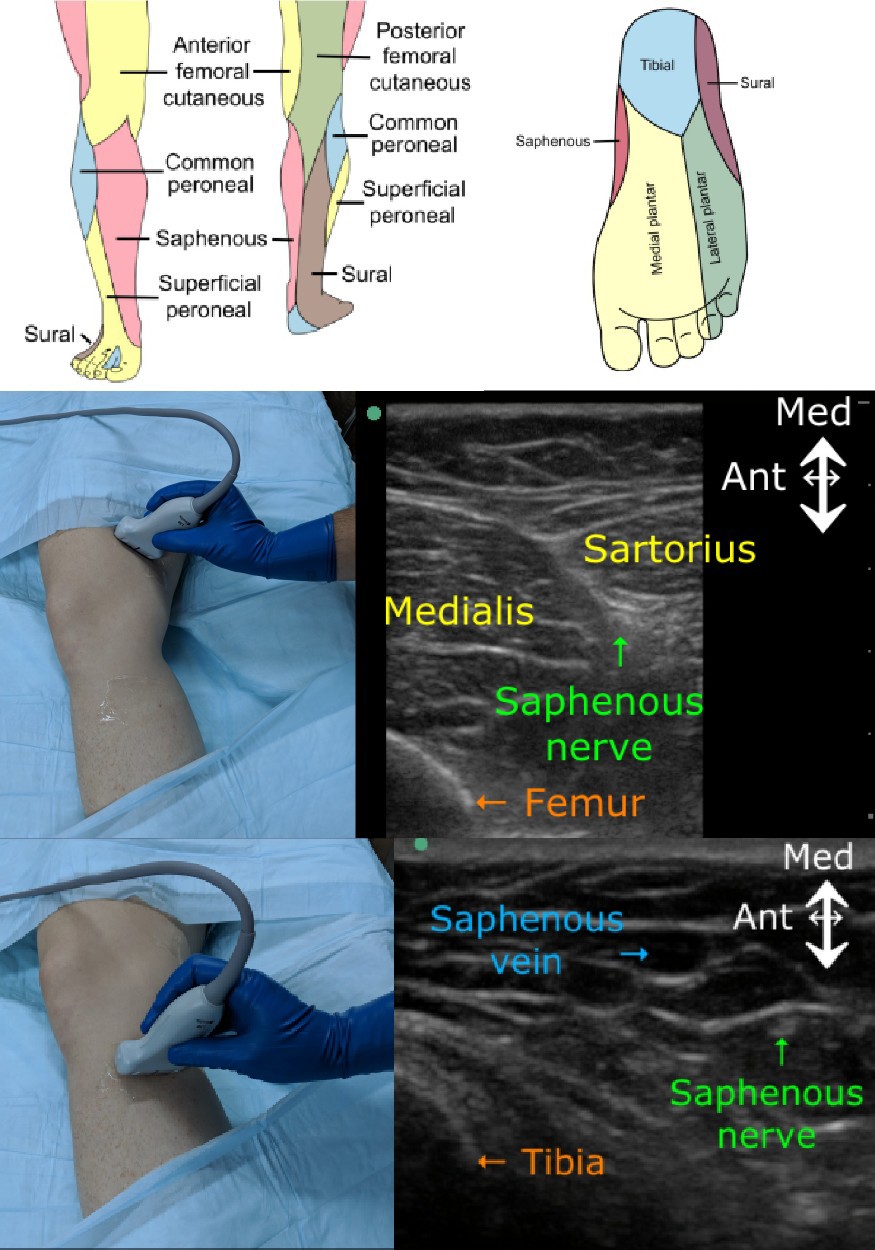
- Saphenous nerve block: the patient is positioned supine with the leg straight. Using the ultrasound probe, it is placed perpendicularly to the thigh at the midpoint between the anterior superior iliac spine and the distal end of the femur. The nerve is identified as it exits from the adductor canal adjacent to the femoral artery. As it is followed distally, it becomes more superficial, traveling with an arterial branch just deep to the sartorius muscle. Using an in-plane approach 10 cc of local anesthetic is injected deep into the sartorius muscle at the lateral border of the artery.
-
PENG block: The pericapsular nerve group (PENG) block is an interfascial plane block aiming to block articular branches supplied by femoral, obturator, and accessory obturator nerves. PENG block is indicated for anterior hip arthroplasties, lateral hip arthroplasties, and for hip fractures. It is performed in supine position by depositing 15-20 ml of local anesthetic in the plane between the psoas tendon and the pubic ramus under direct ultrasound visualization. Femoral nerve block, fascia iliaca compartment block, or lumbar plexus block have been used to manage post-operative analgesia in hip surgeries. These blocks result in weakness of quadriceps muscles and thus predispose to fall. These blocks also result in incomplete analgesia to the hip as here is sparing of few articular branches to the hip. The main advantage of PENG block is that it provides better analgesia of the hip without causing any muscle weakness. As there is no muscle weakness so the patient can participate in physical therapy early.
-
iPACK block: IPACK block is an acronym for infiltration of local anesthetic into the interspace between the popliteal artery and the posterior capsule of the knee. This technique was first introduced by Dr. Sanjay K Sinha at the American Society of Regional Anesthesia (ASRA) meeting in 2012. iPACK block is used for postoperative analgesia for total knee arthroplasty and cruciate ligament repair. Posterior knee pain is mediated by articular branches arising mainly from the tibial nerve with contributions from the obturator nerve. In iPACK block, 15-20 ml of local anesthetic is deposited under ultrasound guidance in tissue plane femoral artery and posterior aspect of the capsule of the knee joint. The main advantage of iPACK block is that it is a muscle strength sparing block and doesn't result in foot drop or loss of sensorimotor function of leg and foot.
Complications
Potential complications and side effects are dependent upon the type of block performed. However, complications include peripheral nerve injury (although not common, the rate may be as high as 8% to 10%), hematoma, local anesthetic systemic toxicity, allergic reaction, infection, and a secondary injury, which includes reduced sensation after nerve block.[4][5][6]
Enhancing Healthcare Team Outcomes
Peripheral nerve blocks are often performed by anesthesiologists, surgeons, and emergency department physicians. However, a dedicated nurse must monitor the patient's vital signs during the procedure. More important, resuscitation equipment must be in the room before starting the procedure. A protocol should be established to conduct a peripheral nerve block to ensure patient safety and improve patient outcomes.
Media
(Click Image to Enlarge)
(Click Video to Play)
(Click Video to Play)
Suprascapular Nerve Block, Video. Ultrasound-guided suprascapular nerve block at the level of the suprascapular notch.
Contributed by Eric Helm, MD
References
Kurita GP,Sjøgren P,Klepstad P,Mercadante S, Interventional Techniques to Management of Cancer-Related Pain: Clinical and Critical Aspects. Cancers. 2019 Mar 29; [PubMed PMID: 30934870]
Raj N, Regional anesthesia for sternotomy and bypass-Beyond the epidural. Paediatric anaesthesia. 2019 Mar 12; [PubMed PMID: 30861264]
Donado C,Solodiuk J,Rangel SJ,Nelson CP,Heeney MM,Mahan ST,Ullrich C,Tsegaye B,Berde CB, Patient- and Nurse-Controlled Analgesia: 22-Year Experience in a Pediatric Hospital. Hospital pediatrics. 2019 Feb; [PubMed PMID: 30655310]
Saranteas T,Koliantzaki I,Savvidou O,Tsoumpa M,Eustathiou G,Kontogeorgakos V,Souvaltzoglou R, Acute pain management in trauma: anatomy, ultrasound-guided peripheral nerve blocks and special considerations. Minerva anestesiologica. 2019 Feb 7; [PubMed PMID: 30735016]
Tran Q,Salinas FV,Benzon HT,Neal JM, Lower extremity regional anesthesia: essentials of our current understanding. Regional anesthesia and pain medicine. 2019 Jan 11; [PubMed PMID: 30635506]
Level 3 (low-level) evidenceHussain N,McCartney CJL,Neal JM,Chippor J,Banfield L,Abdallah FW, Local anaesthetic-induced myotoxicity in regional anaesthesia: a systematic review and empirical analysis. British journal of anaesthesia. 2018 Oct; [PubMed PMID: 30236244]
Level 1 (high-level) evidence