Introduction
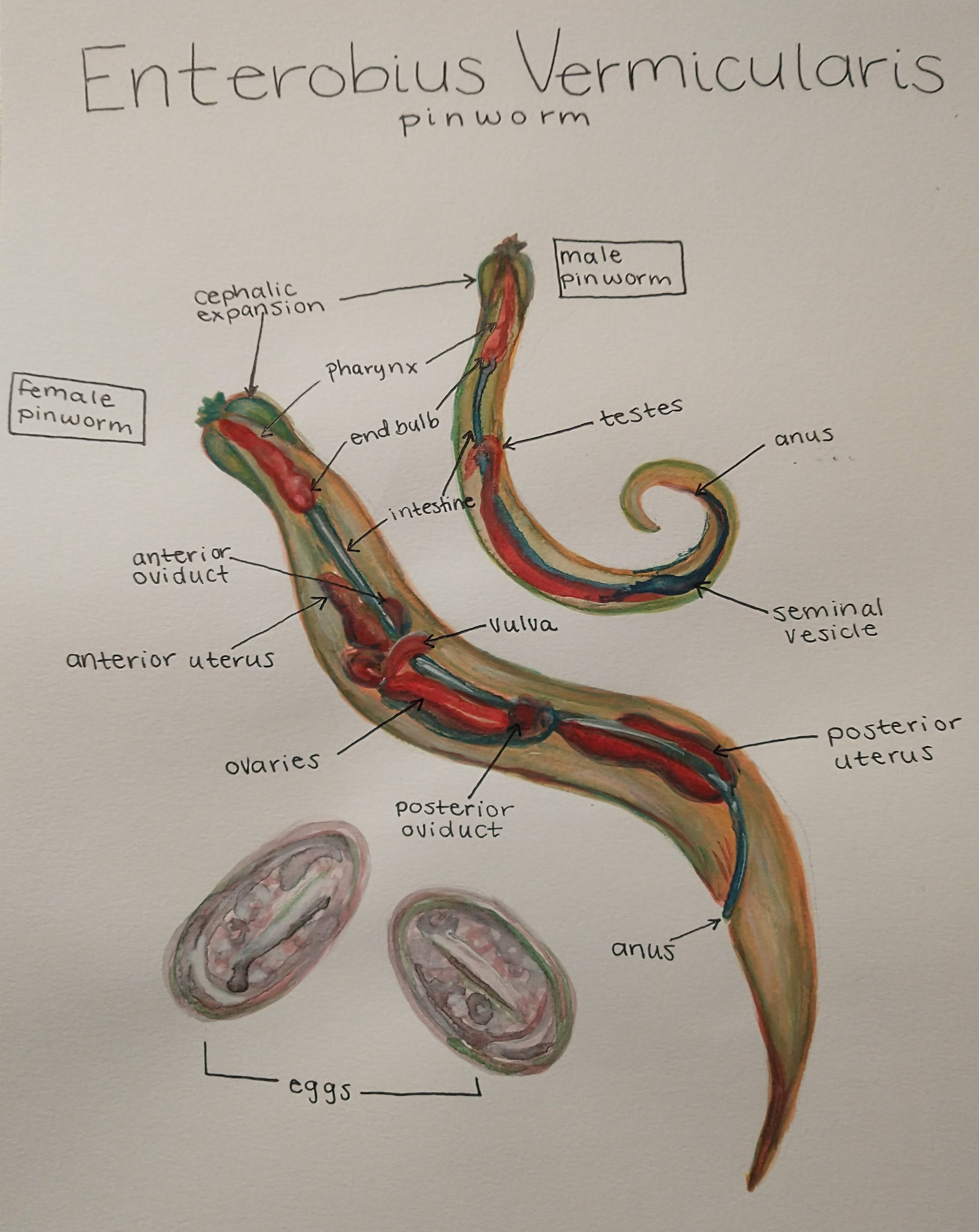
Enterobius vermicularis, also called pinworm, is one of the most common nematode infections in the world. Originally, E. vermicularis was named Oxyuris vermicularis. Humans are the only natural host for this infection. Transmission occurs in people who are living in crowded environments and usually occurs within families. The worms are tiny, thread-like, and whitish. The worm is named after the characteristic pin-like tail present on the posterior part of female worms.[1][2]
Pinworm infestation usually occurs in children. Transmission is via direct contact with contaminated items or even during sexual contact. Most infections are asymptomatic. While the cure rate is high, recurrences are common.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Infection most commonly occurs in children, but any individual is susceptible to E. vermicularis infection. People from tropical climates and school-aged children are the most vulnerable. Infection is caused by the ingestion of the pinworm eggs. Transmission is most commonly through the fecal-oral route.[3]
Risk factors for pinworms include poor hygiene, eating after touching contaminated items and living with an individual who is identified as egg positive.
Epidemiology
The male to female infection frequency is 2 to 1. However, a female predominance of infection is seen in those between the ages of 5 and 14 years. It most commonly affects children younger than 18 years of age. It is also commonly seen in adults who take care of children and institutionalized children. Center for Disease Control and Prevention data indicates that there are about 40 million people estimated to have been infected in the United States. Transmission can occur via contact with contaminated clothes, bedding, personal care products, and furniture. Fecal-oral is the most common mode of transmission. Rarely, transmission can occur via inhalation mode when eggs are inhaled and then subsequently swallowed.
Pathophysiology
Enterobius vermicularis is an organism that primarily lives in the ileum and cecum. Once E. vermicularis eggs are ingested, they take about 1 to 2 months to develop into adult worms which happens in the small intestine. These do not usually cause any symptoms when confined to the ileocecal area. The female adult worms and ova migrate to the anal area mostly at night time and deposit thousands of eggs in the perianal area. This migration causes pruritus. Eggs hatch near the anal area causing perianal pruritus. This leads to contamination of the fingers and results in ingestion of the eggs (autoinfection) and restarting of the life cycle of the worm. Occasionally, the larvae migrate back into the rectum and to the small intestine and begin the life cycle (retro infection).
History and Physical
Approximately a third of patients with Enterobius vermicularis are asymptomatic. The most common symptom associated with pinworm infestation is perianal itching. Perianal erythema may be seen due to the itching and scratching. Sometimes a superficial bacterial infection can occur at the scratching sites resulting in erythema and warmth. Persistent itching can cause disturbances in sleep and may lead to insomnia. Female genitourinary infections have also been reported in the literature. Watery diarrhea has been reported in some patients. Sometimes abdominal pain and other serious complications like appendicitis can occur due to worms blocking the lumen in the appendix or lead to inflammation around the appendix.[4] Sometimes tiny thread-like worms may be visible to the naked eye in the perianal area.
Evaluation
Enterobius can be diagnosed through a cellophane tape test or pinworm paddle test where an adhesive tape-like material is applied to the perianal area and then examined under a microscope. The examination might reveal characteristic ova which are 50 by 30 microns in size and have a flattened surface on one side or may reveal the worms. Female worms are around 8 to 13 mm long while male worms are 2 to 5 mm long. The examination is usually done in the early morning for higher diagnostic yield. If the examination is negative for five consecutive mornings, then the diagnosis is ruled out. Stool examination is not helpful in the diagnosis of E. vermicularis as they are only occasionally excreted in the stool usually. Sometimes analysis of the stool specimen is recommended to rule out other causes.
Treatment / Management
Treatment consists of the following antihelminthic medications:
Albendazole: Given on an empty stomach, a 400-mg, one-time dose followed by a repeat dose in 2 weeks
OR
Mebendazole: A 100-mg, one-time dose followed by a repeat dose in two weeks
OR
Pyrantel Pamoate: Available over the counter in the United States; Dose of 11 mg/kg up to a maximum 1 gm given 2 weeks apart
Other medications that have been used to treat enterobiasis are ivermectin and piperazine, although the latter has lower efficacy and higher toxicity.[5]
Enterobiasis can cause recurrent reinfection, so treating the entire household, whether symptomatic or not is recommended to prevent a recurrence.
Treatment of Enterobius infection in pregnancy should be reserved for patients who have significant symptoms. In pregnant patients, pyrantel pamoate is preferred over other medications.
Young pinworms tend to be resistant to treatment and hence two doses of medication, two weeks apart are recommended. At the same time, all members of the infected child must be treated. If a large number of children are infected in a class, everyone should be treated twice at 2-week intervals. Follow up is vital to ensure that a cure has been obtained.
Differential Diagnosis
- Pruritus ani
- Pruritus vulvae
- Atopic dermatitis
- Perirectal abscess
- Cellulitis
Toxicity and Adverse Effect Management
Pyrantel pamoate can cause adverse effects like nausea, vomiting, anorexia, abdominal cramps, diarrhea. It should be avoided in children younger than 2 years of age. Mebendazole and albendazole should be avoided in the first trimester of pregnancy and children younger than 1 year of age. Pregnant patients should consult their doctors before initiating any therapy.
Prognosis
Prognosis following a pinworm infection is excellent. Patients are recommended to follow up with their physicians after completion of the treatment to make sure they do not have any reinfection. Is symptoms recur then testing and treatment as above should be re-initiated.
Ectopic pinworm infections have been described in many organs including the vagina, inguinal area, genitals, peritoneum, liver, oral cavity, lungs, and pelvis. There are even reported cases of appendicitis caused by impaction of the organ by pinworms. While death is very rare, recurrences are common. Eradicating pinworms from institutions is very difficult and long term surveillance is required. To completely eradicate the pinworm, everyone in the classroom or in the family has to be treated.
Complications
Occasionally a superficial bacterial infection can occur at the scratching sites due to intense perianal pruritus. Other complications reported are female genitourinary infections like vulvovaginitis, urinary tract infection in young girls. Appendicitis has also been reported as a consequence of longstanding pinworm infestation.
Deterrence and Patient Education
Patients should be educated on the need to maintain hygiene and wash their hands regularly to prevent the spread of infection and reinfection.
Pearls and Other Issues
Preventive strategies recommended are:
- Washing hands regularly, particularly before eating and after changing diapers.
- Taking a bath early in the morning to prevent egg contamination should be encouraged in at-risk patients.
- Trimming of fingernails should be encouraged.
- Children should be advised to avoid sucking their fingers and touching their perianal area.
Enhancing Healthcare Team Outcomes
Enterobius vermicularis infection is usually treated by the primary care nurse practitioner, physician assistant, or primary care physician. Pharmacists have a role in explaining to the patients the side effects of these medications used to treat pinworms as one of the drugs, pyrantel pamoate is available over the counter in the United States. School nurses should also be aware of the manifestations of pinworm infection to prevent their spread in the schools and daycares.[6] Patient education is vital in a coordinated approach by nurses, pharmacists, and clinicians. Parents and caregivers need to be told that all clothes, linen, and towels must be washed with soap and hot water. Hand washing and good hygiene must be practiced at all times. A coordinated team approach to care and followup will provide the best results. [Level V]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Cook GC. Enterobius vermicularis infection. Gut. 1994 Sep:35(9):1159-62 [PubMed PMID: 7959218]
Level 3 (low-level) evidenceMarkell EK. Intestinal nematode infections. Pediatric clinics of North America. 1985 Aug:32(4):971-86 [PubMed PMID: 3895141]
Level 3 (low-level) evidenceAshford RW, Hart CA, Williams RG. Enterobius vermicularis infection in a children's ward. The Journal of hospital infection. 1988 Oct:12(3):221-4 [PubMed PMID: 2904463]
Level 3 (low-level) evidenceDahlstrom JE, Macarthur EB. Enterobius vermicularis: a possible cause of symptoms resembling appendicitis. The Australian and New Zealand journal of surgery. 1994 Oct:64(10):692-4 [PubMed PMID: 7945067]
Level 2 (mid-level) evidenceYang CA, Liang C, Lin CL, Hsiao CT, Peng CT, Lin HC, Chang JG. Impact of Enterobius vermicularis infection and mebendazole treatment on intestinal microbiota and host immune response. PLoS neglected tropical diseases. 2017 Sep:11(9):e0005963. doi: 10.1371/journal.pntd.0005963. Epub 2017 Sep 25 [PubMed PMID: 28945752]
Wang S, Yao Z, Hou Y, Wang D, Zhang H, Ma J, Zhang L, Liu S. Prevalence of Enterobius vermicularis among preschool children in 2003 and 2013 in Xinxiang city, Henan province, Central China. Parasite (Paris, France). 2016:23():30. doi: 10.1051/parasite/2016030. Epub 2016 Jul 26 [PubMed PMID: 27460881]