Anatomy, Bony Pelvis and Lower Limb: Posterior Tibial Artery
Anatomy, Bony Pelvis and Lower Limb: Posterior Tibial Artery
Introduction
The lower leg divides into four compartments. These four compartments are the anterior, lateral, superficial posterior, and deep posterior compartments. The anterior compartment contains the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius muscles, innervated by the deep peroneal nerve and supplied by the anterior tibial artery. The anterior compartment muscles function as the primary extensors of the ankle (dorsiflexion) and extensors of the toes. The lateral compartment of the lower limb contains the fibularis longus and brevis muscles and receive innervation from the superficial fibular nerve. The peroneal artery provides muscular branches to the lateral compartment but is, in fact, a posterior compartment structure. The lateral compartment muscles function primarily to evert the foot and weakly plantarflex the foot at the ankle. The superficial posterior compartment contains the gastrocnemius, soleus, and plantaris muscles. The deep posterior compartment contains the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles. The superficial and deep posterior compartment muscles are supplied by the posterior tibial artery and innervated by the tibial nerve, both of which course in the deep posterior compartment. The posterior compartment muscles serve as the primary flexors of the ankle (plantarflexion) and flexors of the toes. The arteries of the lower limb are susceptible to several pathologies, including atherosclerotic plaque buildup, compartment syndrome, trauma, and in rare instances, aneurysm. There have been only 33 documented cases of true infra-popliteal arterial aneurysms, twelve of which involve the posterior tibial artery.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
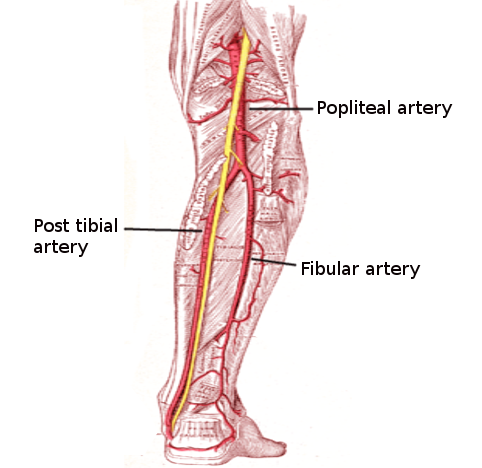
The blood supply of each of the four compartments of the lower limb originates at the common femoral artery, a branch of the external iliac artery, which eventually splits into deep and superficial branches. The deep branch (profunda femoris artery) continues to supply the posterior structures of the thigh through the medial circumflex femoral artery and lateral circumflex femoral artery. The superficial femoral artery continues inferiorly passing through the adductor hiatus into the popliteal fossa to become the popliteal artery posterior to the knee. The popliteal artery divides toward the distal end of the popliteal fossa to give rise to the tibioperoneal trunk and the anterior tibial artery. The tibioperoneal trunk then divides approximately 2.5 cm from its origin, into the peroneal and posterior tibial arteries.
The posterior tibial artery is the largest of the terminal branches of the popliteal artery. It travels with the tibial nerve in the deep posterior compartment of the leg along its fascial border with the superficial compartment. At the level of the ankle, its path is more superficial, and it is palpable posterior to the medial malleolus as it courses through the tarsal tunnel. It then gives off the distinct branches of the posterior medial malleolar artery and the artery of the tarsal canal, which is the dominant blood supply to the talar body. In the foot, the posterior tibial artery bifurcates into the medial and lateral plantar arteries after crossing the sustentaculum tali.[2]
Embryology
The limb buds of the embryo begin to form about five weeks after fertilization as the lateral plate mesoderm migrates into the limb bud region and condenses along the central axis to eventually form the vasculature and skeletal components of the lower limb.[3][4] Several factors influence the formation of the limb bud vasculature and musculature, including retinoic acid, sonic hedgehog (SHH), HOX genes, apical ectodermal ridge (AER) and the zone of polarizing activity (ZPA). Retinoic acid is a global organizing gradient that initiates the production of transcription factors that specify regional differentiation and limb polarization. The apical ectodermal ridge (AER) produces fibroblast growth factor (FGF), which promotes the outgrowth of the limb buds by stimulating mitosis.[3][4] The zone of polarizing activity (ZPA) manufactures SHH, which promotes the organization of the limb bud along the anterior-posterior axis. SHH activates specific HOX genes – Hoxd-9, Hoxd-10, Hoxd-11, Hoxd-12, Hoxd-13 – which are essential in limb polarization and regional specification.[3][4]
The earliest arterial supply of the lower limb bud is the axis artery and the terminal plexus, both of which come from the umbilical artery. The axis artery then gives off branches that form the anterior tibial artery and the posterior tibial artery.[3][4] The anterior tibial artery continues to form the dorsalis pedis artery, and the posterior tibial artery continues to form the medial and lateral plantar arteries. The second, separate arterial channel, is formed by the external iliac artery, which gives rise to the femoral artery of the lower limb that eventually connects to the axis artery.[3][4] While most of this artery regresses, it also gives rise to the inferior gluteal artery, sciatic artery, the proximal part of the popliteal artery, and the distal part of the peroneal artery.[3][4]
Physiologic Variants
Anatomical variations of the posterior tibial artery commonly arise from variations of the popliteal artery. The three most frequent variations in the branching of the popliteal artery are a high origin of the anterior tibial artery, the trifurcation of the anterior tibial artery, peroneal artery, and posterior tibial artery, and a hypoplastic or aplastic posterior tibial artery. The specific order and percentages of these variations differ slightly between literature reviews; however, they make up the top three anatomical variations in each review article.[5]
Surgical Considerations
The arteries of the lower limb are particularly susceptible to atherosclerotic plaque buildup and peripheral arterial disease where the arterial lumen of the lower extremities becomes progressively occluded by atherosclerotic plaque, which can lead to decreased arterial blood flow.[6] Initial management of PAD is with lifestyle changes and medications; however, if this fails, surgical intervention may be required.[6] Typical procedures for PAD include angioplasty, clot removal, and bypass surgery. Posterior tibial artery bypass surgery is possible for patients with critical limb ischemia characterized by rest pain and tissue loss in the form of ulceration and/or gangrene.[7]
Another surgical intervention involving the posterior tibial artery involves posterior tibial arterial aneurysm repair. Aneurysms of the infrapopliteal region are extremely rare, and most of them are reportedly associated with either infection or inflammatory processes.[8] Of the infra-popliteal blood vessels, there are only 12 reports of true dilation of the posterior tibial artery.[8] The management options for these aneurysms vary from conservative approaches to surgical excision, but due to the limited number of published cases, standard treatment remains undefined. The preferred treatment cited in the literature is surgical excision with reconstitution by primary repair or interposition vein graft.
Clinical Significance
The posterior tibial artery is superficial and readily palpable just behind the medial malleolus. For this reason, it is used during the physical exam to assess for peripheral vascular disease, which affects about 12% of the population.[9] It can be palpated by wrapping your fingers around the heel of the patient and pressing over the top of the medial malleolus. A weakened or absent posterior tibial artery pulse may be indicative of vascular insufficiency.[9]
The posterior tibial artery can also be involved in compartment syndrome. Compartment syndrome may occur acutely following blunt force injury or trauma, or as a chronic, exertional syndrome commonly seen in athletes.[10] The muscle groups of the lower limb divide into compartments formed by strong, inflexible fascial membranes. Compartment syndrome occurs when increased pressure within one of these compartments compromises circulation and function to the tissues within that space.[10] The posterior compartments contain muscles that primarily flex the foot at the ankle (plantar flexion), flex the toes, and are innervated and supplied by the tibial nerve and posterior tibial artery, respectively. Increased pressure in the posterior compartment can cause plantar paresthesias, weakness of toe flexion, and pain with passive extension of the toes.[10] Compartment syndrome constitutes a medical emergency that requires fasciotomy of the involved compartment.
Aneurysms of the posterior tibial artery, although rare, have been reported. False aneurysms (pseudoaneurysms) are more common and are commonly associated with trauma.[8] True aneurysms typically occur as a result of infection or inflammatory processes (Sagar 2014) and may present as an asymptomatic lump behind the ankle proximal to the medial malleolus. Doppler ultrasound can help to confirm the presence of a true aneurysm. There are only twelve reported cases of true posterior tibial arterial aneurysms. Consequently, there is no identified standard treatment at present. The published literature recommends early diagnosis and treatment in the form of excision to prevent further complications.[8]
Media
References
Tshomba Y, Papa M, Marone EM, Kahlberg A, Rizzo N, Chiesa R. A true posterior tibial artery aneurysm--a case report. Vascular and endovascular surgery. 2006 May-Jun:40(3):243-9 [PubMed PMID: 16703214]
Level 3 (low-level) evidenceChmielewski P, Warchoł Ł, Gala-Błądzińska A, Mróz I, Walocha J, Malczak M, Jaworek J, Mizia E, Walocha E, Depukat P, Bachul P, Bereza T, Kurzydło W, Gach-Kuniewicz B, Mazur M, Tomaszewski K. Blood vessels of the shin - posterior tibial artery - anatomy - own studies and review of the literature. Folia medica Cracoviensia. 2016:56(3):5-9 [PubMed PMID: 28275266]
Mróz I, Kielczewski S, Pawlicki D, Kurzydło W, Bachul P, Konarska M, Bereza T, Walocha K, Kaythampillai LN, Depukat P, Pasternak A, Bonczar T, Chmielewski P, Mizia E, Skrzat J, Mazur M, Warchoł Ł, Tomaszewski K. Blood vessels of the shin - anterior tibial artery - anatomy and embryology - own studies and review of the literature. Folia medica Cracoviensia. 2016:56(1):33-47 [PubMed PMID: 27513837]
Gros J, Tabin CJ. Vertebrate limb bud formation is initiated by localized epithelial-to-mesenchymal transition. Science (New York, N.Y.). 2014 Mar 14:343(6176):1253-6. doi: 10.1126/science.1248228. Epub [PubMed PMID: 24626928]
Level 3 (low-level) evidenceDay CP, Orme R. Popliteal artery branching patterns -- an angiographic study. Clinical radiology. 2006 Aug:61(8):696-9 [PubMed PMID: 16843754]
Level 2 (mid-level) evidenceOlin JW, Sealove BA. Peripheral artery disease: current insight into the disease and its diagnosis and management. Mayo Clinic proceedings. 2010 Jul:85(7):678-92. doi: 10.4065/mcp.2010.0133. Epub [PubMed PMID: 20592174]
El-Sayed HF. Bypass surgery for lower extremity limb salvage: vein bypass. Methodist DeBakey cardiovascular journal. 2012 Oct-Dec:8(4):37-42 [PubMed PMID: 23342187]
Sagar J, Button M. Posterior tibial artery aneurysm: a case report with review of literature. BMC surgery. 2014 Jun 16:14():37. doi: 10.1186/1471-2482-14-37. Epub 2014 Jun 16 [PubMed PMID: 24934412]
Level 3 (low-level) evidenceWalker HK, Hall WD, Hurst JW, Hill RD, Smith RB III. Examination of the Extremities: Pulses, Bruits, and Phlebitis. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250191]
Mabvuure NT, Malahias M, Hindocha S, Khan W, Juma A. Acute compartment syndrome of the limbs: current concepts and management. The open orthopaedics journal. 2012:6():535-43. doi: 10.2174/1874325001206010535. Epub 2012 Nov 30 [PubMed PMID: 23248724]