Introduction
Wound pressure injuries have been given various names over the last several years. In the past, they were referred to as pressure ulcers, decubitus ulcers, or bed sores; and now they are most commonly termed "pressure injuries." Pressure injuries are defined as the breakdown of skin integrity due to some types of unrelieved pressure. This can be from a bony area on the body coming into contact with an external surface which leads to pressure injury. These wounds represent the destruction of normal structure and function of the skin and soft tissue through a variety of mechanisms and etiologies. The wound healing process is affected by various factors including infection, the presence of chronic diseases like diabetes, aging, nutritional deficiency like vitamin C, medications like steroids, and low perfusion of oxygen and blood flow to the wound in cases of hypoxia and cold temperature. Pressure ulcers result from long periods of repeated pressure applied to the skin, soft tissue, muscle, and bone. In pressure ulcers, the external pressure exceeds capillary closing pressure.[1][2][3]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Elderly and bed-bound individuals are more prone to developing pressure (decubitus) ulcers. The hip and buttock region accounts for approximately two-thirds all pressure ulcers. Also, the skin underneath the nasogastric or endotracheal tubes might be affected by pressure ulcers. They are slightly more predominant in females than males. Pressure ulcers are caused by a prolonged period of repeated friction and shearing pressure of the skin overlying the bony prominences along with some of the following intrinsic causes:
- Loss of skin fragility
- Decreased blood flow
- Loss of muscle volume
- Spinal cord injuries
- Nutritional insufficiency
- Moisture due to fecal and/or urinary incontinence
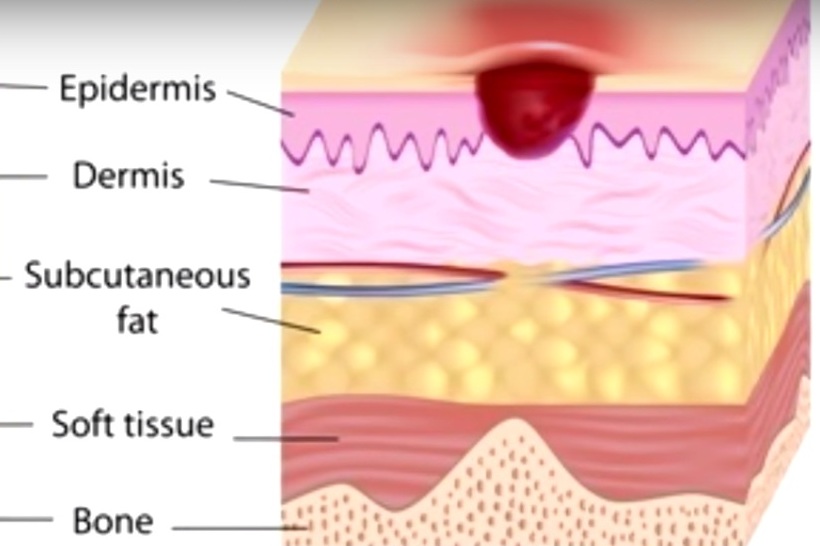
Understanding how a pressure injury happens requires a review of the basic layers of the skin. The epidermis is the most superficial layer. Just below the epidermis is the dermis, and then right below the dermis is the capillary bed which feeds, perfuses, and supplies the dermis and epidermis. Below the capillary bed is the fatty subcutaneous tissue, followed by muscle and then bone. Hence, in a patient who is sitting in the chair for a really long time, the coccyx bone which is obvious the bony prominence is going to place the patient at risk for developing a pressure injury by exerting upward pressure on bottom skin layers. In addition, there is the external hard surface of the chair that can also place pressure on the skin and bony prominences. If the pressure is prolonged, it can compromise blood supply to the skin.
It is very important to avoid friction and shear force injuries. These injuries may occur when the patient is sliding down in the bed. For example, when the coccyx bone is moving upwards and the skin is moving downward (i.e., the two forces move in opposite direction), the middle layer which supplies and perfuses the dermis and epidermis may tear, leading to decreased perfusion and eventually resulting in a pressure injury. There are various stages of pressure injury, all of which classify the injury based on the depth of skin injury. Pressure ulcers are categorized into four stages:
- Stage 1: just erythema of the skin
- Stage 2: erythema with the loss of partial thickness of the skin including epidermis and part of the superficial dermis
- Stage 3: full thickness ulcer that might involve the subcutaneous fat
- Stage 4: full thickness ulcer with the involvement of the muscle or bone
The most common sites for pressure injuries include the sacrum (tailbone) followed by the heels, trochanter (hip bone), and the ischium (sitting erect bone), especially in paraplegic patients.[4][5][6]
Indications
Before mentioning ways to treat pressure ulcers, it is important to discuss ways to prevent them; ironically, the ways to prevent ulcers are also ways to treat them. All hospitals use screening tools on admission to determine the risk of pressure sores.
Braden Scale
The Braden scale is a widely used screening too to determines the patients who are at risk. This assessment tool consists of six categories:
- Sensory perception
- Moisture
- Activity
- Mobility
- Nutrition
- Friction/shear
Number one through four on these categories indicates that there is no potential problem; however, receiving a one means the patient is at great risk. Friction and shear is the sixth category which often can disrupt skin integrity. The highest Braden score one can achieve is 23, and the lowest is 6; the lower the number, the higher the risk of developing an ulcer.
Norton Scale
The Norton scale is also used as an assessment tool for patients who are at great risk of developing pressure ulcers. This scale relies on these factors:
- Physical condition
- Mental condition
- Activity
- Mobility
- Continence
Each category has four grades (1-4), number 4 means the patient is healthy and number 1 means the patient is at great risk. The highest possible score is 20, and the lowest possible score is 5. The onset of risk = 16 or below; high risk = 12 or below.
Other simple prevention measures include proper nutrition, pressure relieving repositioning, hygiene and moisture control, special mattresses, and topical skin care. Adequate nutrition is needed for tissue metabolism and is necessary for the prevention and healing of pressure ulcers. The patient must be provided with sufficient calories, fluid, protein, vitamin C, and zinc. For those who are not able to eat, a feeding tube may be necessary, otherwise wound healing will not take place.
Contraindications
The use of harsh soaps, irritant solutions, aggressive debridement, and hard mattresses should be avoided in treating patients with pessure ulcers because it might aggravate the situation and lead to delayed healing, especially in elderly bed-bound patients.
Equipment
Different risk assessment tools that have been developed; the most widely used is the Braden and Norton Scales discussed above.
Personnel
The wound management team is responsible for taking care of any patient with pressure sores. This team usually includes the primary attending, dermatologist and/or plastic surgeon, nurse, nurse assistant, dietitian, and physical therapist. Daily skin check-up is required, especially for patients who are at a high risk for skin breakdown based on the Braden and Norton scales.
Technique or Treatment
Proper repositioning is essential in maintaining skin integrity and is needed in patients who are unable to do this for themselves. Pressure, friction, and shear forces should be avoided during positioning. The most effective way of repositioning is to move the patient every 2 hours so that the ischemic areas can recover. This can be done with the use of pillows or wedges to keep the patient on their side and placing pillows between their legs and under their calves helps take pressure off their back, buttocks, medial aspect of the knees, and heels. Hygiene and moisture reduction are very important, especially for patients who are incontinent; excess moisture is known to cause the skin to break down, and the patient must always be kept dry. This job falls on the nursing assistants who are responsible for making sure the patient is clean at all times. If patients develop skin breakdown due to moisture, the nurse is at fault for not properly delegating and overseeing the nursing assistants.
An air mattress is a pressure-relief device that is constantly being inflated with air to prevent skin breakdown and used to prevent ulcers in patients at high risk or in patients with existing ulcers. If the patient has a Braden score of 12 or less, they should be placed on an air mattress, and a proper skin assessment should be done at least once a day or every shift. For at-risk patients, the nurse must always make sure the patient is clean and dry. Soaps, alcohol-based lotions, and hot water should be avoided when bathing a patient because these can cause the skin to become dry and leave an alkaline residue which discourages the growth of normal skin bacteria. Initiating weekly rounds is a great way to assess the wound and skin integrity. Working as a team, the wound care doctor, nurse, and nursing assistant should fully assess all patients admitted to the floor. Bedsores are evaluated and proper care determined according to need. To prevent and treat pressure ulcers, it is important to know what they are and how to assess and treat them with help from the entire wound team. Debridement of necrotic tissues will accelerate healing by preventing the growth of pathogenic organisms.
Several reports on the therapeutic efficacy of laser sessions, ultrasound, recombinant platelet-derived growth factors, and hyperbaric oxygen have shown some improvement in the healing of pressure injuries, especially stage III and above; however, more clinical trials are needed.
Complications
Even with good nursing care in a high-standard medical facility, complications of pressure injuries still occur and can be life-threatening. All stages of pressure ulcers are prone to complications, especially stage III and stage IV. These complications include cellulitis, osteomyelitis, necrotizing fasciitis, gas gangrene, and septicemia.
Clinical Significance
Pressure ulcers are primarily diagnosed clinically. It is helpful to look at other lesions on the individual’s skin to see the body's response to physical trauma. It is also easier to diagnose pressure ulcers by inspection and palpation, which usually reveals erythematous macerated texture. History should also include assessing comorbid conditions like diabetes and spinal injuries. Prevention and treatment of pressure ulcers are very important to avoid the life-threatening complications mentioned.
Enhancing Healthcare Team Outcomes
The primary goal is to prevent pressure ulcers through various means including the use of air-fluidized or foam mattresses, improving the nutritional status of the patients, proper placing of patients in bed, changing position frequently, and treatment of the underlying diseases. A treatment plan involves the removal of all devitalized tissue that may serve as a reservoir for bacterial contamination (debridement). Also, it involves dressing by utilizing hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal. Treatment of underlying infection by topical or systemic antibiotic medications might be needed to help in the healing process, but tissue culture should be obtained before selecting the accurate drug. Pain and discomfort can be controlled by analgesics. A dietary consult should be made to ensure that the patient is receiving adequate calories. When possible, the patient should be out of bed to chair, and physical therapy should be consulted for ambulation and/or exercise. Wound care specialty trained nurses should assist in dressing changes, debridement of wounds, and provide close followup care. The nurses should also assist the clinician in the education of the patient and family. Pressure ulcers are very difficult to treat, it is crucial that the nurses and clinicians work together as an interprofessional team to provide the very best care including treatment, monitoring, and followup care. [7][8][9] (Level V)
Outcomes
Pressure injuries are common and often result in a prolonged hospital stay and increased healthcare costs. Each year nearly 60,000 people die because of complications associated with pressure wounds. The two most common causes of death linked to pressure injuries are amyloidosis and renal failure. Infection is another major complication of pressure injuries, which often lead to osteomyelitis and chronic non-healing wounds. Unfortunately, despite awareness of the problem, the rates of pressure wounds remain high in long-term care facilities and nursing homes, where a lack of staff and optimal care is not always possible.[10][11](Level V)
Media
(Click Image to Enlarge)
References
Cowan L,Garvan C,Rugs D,Barks L,Chavez M,Orozco T, Pressure Injury Education in the Department of Veterans Affairs: Results of a National Wound Provider Cross-sectional Survey. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society. 2018 Sep/Oct [PubMed PMID: 30188391]
Level 2 (mid-level) evidenceTappen RM,Newman D,Huckfeldt P,Yang Z,Engstrom G,Wolf DG,Shutes J,Rojido C,Ouslander JG, Evaluation of Nursing Facility Resident Safety During Implementation of the INTERACT Quality Improvement Program. Journal of the American Medical Directors Association. 2018 Oct [PubMed PMID: 30108035]
Level 2 (mid-level) evidenceCatania QN,Morgan M,Martin R, Activity-Based Restorative Therapy and Skin Tears in Patients with Spinal Cord Injury. Advances in skin [PubMed PMID: 30028373]
Level 3 (low-level) evidenceDincer M,Doger C,Tas SS,Karakaya D, An analysis of patients in palliative care with pressure injuries. Nigerian journal of clinical practice. 2018 Apr [PubMed PMID: 29607862]
Delmore B,Ayello EA,Smart H,Sibbald RG, Assessing Pressure Injury Knowledge Using the Pieper-Zulkowski Pressure Ulcer Knowledge Test. Advances in skin [PubMed PMID: 30134276]
Level 3 (low-level) evidenceLi D,Mathews C,Zhang F, The characteristics of pressure injury photographs from the electronic health record in clinical settings. Journal of clinical nursing. 2018 Feb [PubMed PMID: 29076271]
Rosen T,Reisig C,LoFaso VM,Bloemen EM,Clark S,McCarthy TJ,Mtui EP,Flomenbaum NE,Lachs MS, Describing visible acute injuries: development of a comprehensive taxonomy for research and practice. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2017 Oct [PubMed PMID: 27913598]
Edsberg LE,Black JM,Goldberg M,McNichol L,Moore L,Sieggreen M, Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society. 2016 Nov/Dec [PubMed PMID: 27749790]
Tadiparthi S,Hartley A,Alzweri L,Mecci M,Siddiqui H, Improving outcomes following reconstruction of pressure sores in spinal injury patients: A multidisciplinary approach. Journal of plastic, reconstructive [PubMed PMID: 27117674]
Odgaard L,Aadal L,Eskildsen M,Poulsen I, Nursing Sensitive Outcomes After Severe Traumatic Brain Injury: A Nationwide Study. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses. 2018 Jun [PubMed PMID: 29652735]
Stojmenski S,Merdzanovski I,Gavrilovski A,Pejkova S,Dzokic G,Tudzarova S, Treatment of Decubitis Ulcer Stage IV in the Patient with Polytrauma and Vertical Share Pelvic Fracture, Diagnosed Entherocollitis and Deep Wound Infection with {i}Clostridium Difficile{/i} with Combined Negative Pressure Wound Therapy (NPWT) and Faecal Management System: Case Report. Open access Macedonian journal of medical sciences. 2017 Jun 15 [PubMed PMID: 28698756]
Level 3 (low-level) evidence