Introduction
Pulse oximetry is sometimes referred to as the fifth vital sign; it is a quick and non-invasive monitoring technique that measures the oxygen saturation in the blood by shining light at specific wavelengths through tissue, most commonly the fingernail bed. Deoxygenated and oxygenated hemoglobin absorb light at different wavelengths, 660 nm, and 940 nm, respectively. The absorbed light is processed by a proprietary algorithm in the pulse oximeter to display a saturation value. In most developed countries, pulse oximetry is the standard of care to use pulse oximetry to monitor oxygen saturation for patients receiving anesthesia.[1][2]
Pulse oximetry is also used in emergency departments, hospital wards, and ambulances to assess blood oxygenation in patients with respiratory difficulties or to monitor the potential respiratory depressant effects of pain medications. Since the widespread use of pulse oximetry in hospitals was instituted, the incidence of unrecognized oxygen desaturation has decreased significantly.[3]
In addition to hospital-grade pulse oximeters, newer and much smaller consumer-grade models are rapidly gaining popularity in sports, private aviation, mountain climbing, and other recreational activity communities. Because of the size and cost of consumer-grade models, many patients with chronic respiratory illnesses purchase these devices to monitor their oxygen saturation or to titrate their medications or oxygen flow at home. Of note, the Food and Drug Administration has not evaluated most consumer-grade devices regarding their reliability to diagnose or treat diseases.
Specimen Collection
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Specimen Collection
Pulse oximeters are well-tolerated medical devices that provide rapid data using noninvasive technology. The most commonly used sites for application are the fingernail and toenail beds. The machine algorithm detects arterial pulsations of very small caliber in arteriolar and capillary tissue beds. Consequently, a reliable signal may not easily be obtained in patients with low tissue perfusion or excessive movement of the extremities. Other sites, including the earlobe, forehead, nasal alar, and lips, have been utilized with success.[4]
In infants, the palm, foot, arm, cheek, tongue, penis, or nasal septum also may be used for probe placement. Site-specific sensors have been developed and calibrated and should be used for those applications whenever available. In addition to collecting light absorption spectra, most pulse oximeters also capture pulse wave activity and display the plethysmographic waves from which the clinician can gain additional valuable information.
Procedures
The spectrophotometry technique is used to determine the peripheral arterial blood oxygen saturation (SpO2) as a marker for the oxygenation of tissues using the Beer-Lambert Law. Pulse oximeter probes have two light emitters and one light detector or sensor aligned to capture the light on the other side of the tissue bed or the reflection of light from a site such as the forehead. Pulse oximeter probes come in single-use adhesive probes or multi-use clips.[5]
However, due to infection control concerns, single-use patient clips have been introduced to the market for specific anatomical sites. Different application sites have specific probes optimized for that site and should be used when available.
Indications
Pulse oximetry is a noninvasive means to rapidly and accurately determine oxygen saturation. This modality is one of the standard monitor parameters used in the critical care setting and during anesthesia cases and is recommended by the American Society of Anesthesiologists.[6]
In addition, pulse oximetry should be used for hospitalized patients receiving medications that may impair their respiration, such as opioids. All patients with acute respiratory disease should be monitored with pulse oximetry, regardless of the setting. Pulse oximetry is used to diagnose hypoxia rapidly and to titrate oxygen supplementation when used with ventilator support and in various disease states.[7]
Avoiding hyperoxia is essential as it may lead to increased morbidity and mortality.[8] Prior to the institution of pulse oximeters, arterial blood gas analysis was used to detect hypoxemia. This technique is painful, and complications may occur, including hematoma, vasospasm, occlusion, thrombus or air embolism, infection, needle-stick injury to the healthcare provider, vessel laceration, hemorrhage, pain, or vasovagal response.
Potential Diagnosis
Conventional pulse oximeters are used to diagnose hypoxia. Recent technological developments in certain pulse oximeters have allowed the assessment of other parameters such as methemoglobin and carboxyhemoglobin levels, total hemoglobin, and oxygen levels above 100% saturation. Pulse wave activity parameters can display volume status in intubated patients, and specific devices display respiratory rate by detecting pulse pressure variation within the respiratory cycle.[9]
The perfusion index (PI), which measures peripheral perfusion, has been used to diagnose the success of increased blood flow after a sympathectomy.[10] The PI can also be used as an indicator of pain in critically ill patients, and there is an apparent inverse relationship between painful stimuli and decreased PI.[11]
Normal and Critical Findings
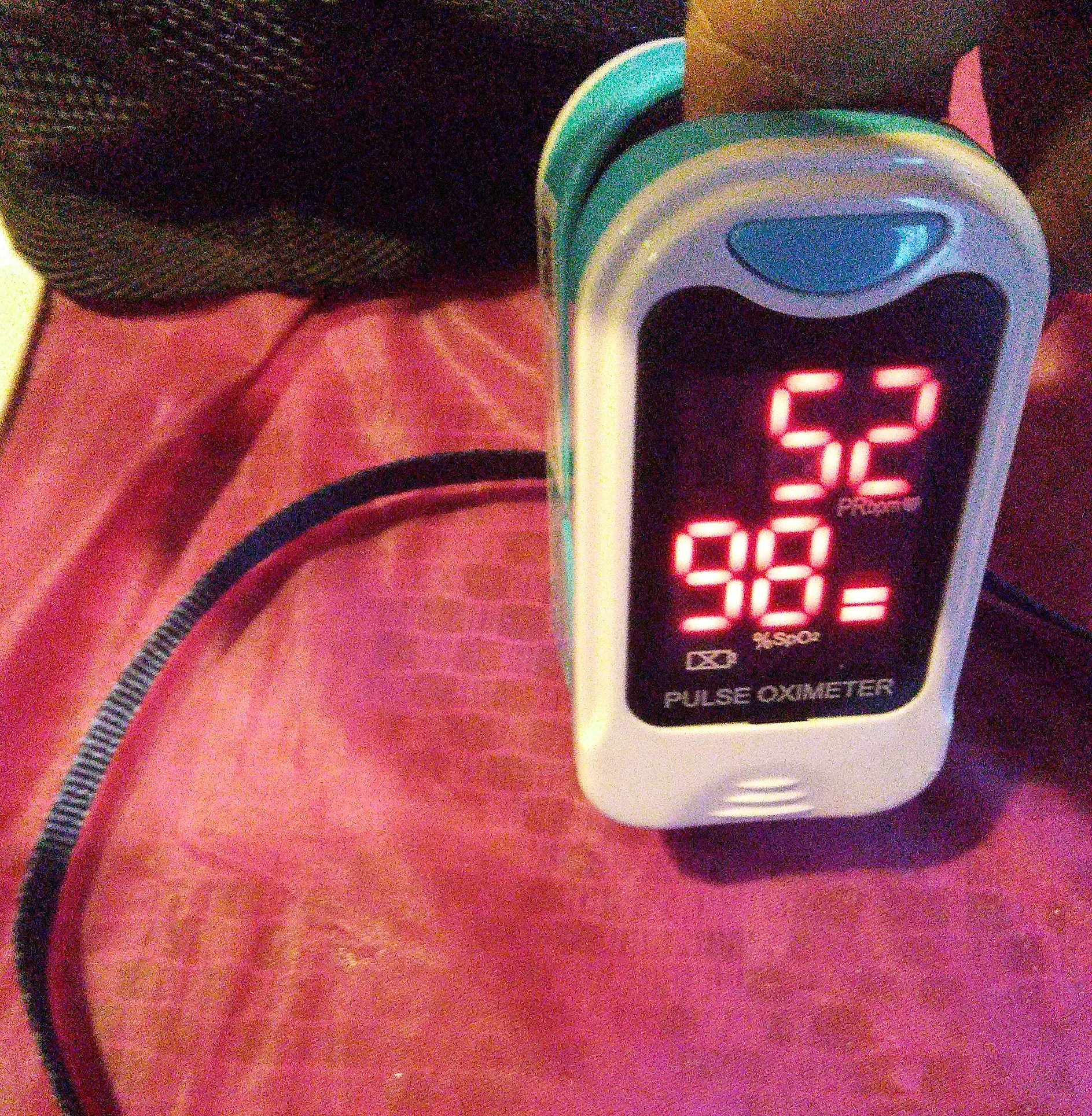
Oxygen saturation levels between 96% and 100% are considered normal at sea level. Healthy individuals living at higher elevations may have lower oxygen saturation levels. Pulse oximeters are usually calibrated to a range of saturation from 70% to 100% with an accuracy of between 2% and 4%, indicating a pulse oximeter reading lower than 70% may not be accurately compared to the gold standard invasive blood gas measurement.[8]
While a pulse oximeter may not demonstrate absolute accuracy, it usually still tracks oxygen saturation and will display lower numbers. Technical reasons exist for the 70% calibration; however, at that low number, patients usually will have clinical signs of hypoxemia that would not necessitate invasive clinical confirmation.
Treatment for that degree of hypoxia would not differ from that for a patient with a saturation of 70%. Critical findings prompting intervention for most patients likely would be in the mid to high 80% range at sea level as the partial pressure of oxygen would be in the 60 mmHg range. However, critical numbers requiring treatment for patients with hypoxic heart defects may be lower at higher altitudes where venous and arterial blood are mixed when entering the systemic circulation.
The normal oxygen levels displayed on a pulse oximeter commonly range from 95% to 100%. Hypoxemia is an oxygen saturation of less than 90%. Healthcare providers must pay attention to oxygenation trends and respond if readings are inconsistent with clinical findings. Because there are several contributing factors, there is no definitive oxygen saturation value below which hypoxia of tissues occurs, nor is there a standard value above which hyperoxia of tissues occurs.
Interfering Factors
Pulse oximetry relies on light absorption through a tissue bed with pulsating blood. Therefore factors that interfere with those parameters can interfere with the readings of pulse oximeters. Pulse oximeter readings may be less accurate at colder temperatures. A temperature of approximately 33 degrees Celsius (91.4 degrees Fahrenheit) should be maintained for reliable readings.
One commonly implicated interfering factor is black or blue nail polish or artificial fingernails, although some studies investigating this topic have been inconclusive.[12][13] If the sensor is placed on a finger with black or blue nail polish or an artificial nail and does not give a reading, placing the sensor sideways on the finger bed has been associated with some success. However, this will be outside that sensor's calibration.
The oxygen saturation of patients with dark skin tones may be overestimated by approximately 2% and varies depending on the device used. This may lead to increased rates of unrecognized hypoxemia.[14]
Intravenous dyes such as methylene blue or indocyanine green, sometimes used for surgical or diagnostic procedures, will color the serum in the blood and may interfere with the light absorption spectrum, resulting in falsely low readings.[15][16]
Dyshemoglobinemias, such as carboxyhemoglobinemia, methemoglobinemia, and others, will change blood color and absorption spectrum and lead to false readings. In these cases, confirmation with a co-oximeter should be obtained. In addition, some of the newer pulse oximeters that utilize multiple wavelengths may display methemoglobinemia.
Light pollution into the sensor of the probe due to ambient light or light from another probe may produce an inaccurate reading. This should be avoided by covering the site or the probe itself.
As stated, pulsating blood is necessary for an accurate pulse oximeter reading. The pulse amplitude in a tissue bed accounts only for 5% of available pulse oximeter signals for analysis. Decreased pulse wave amplitude due to severe hypotension, cold extremities, Raynaud disease, or excessive motion may interfere with an accurate reading.[17]
Hospital-grade pulse oximeters can read through perfusing cardiac arrhythmias such as atrial fibrillation and premature atrial or ventricular contractions. In addition to the oxygen saturation value, most pulse oximeters display the plethysmographic waveform, an additional parameter ensuring accuracy.
Pulse oximeter manufacturers are working to mitigate these factors using different strategies with hardware sensors and software algorithm improvements. Therefore, publications reporting limitations of certain pulse oximeters may be specific to that manufacturer or model.
If a healthcare provider believes the pulse oximeter reading is inaccurate or inconsistent with other clinical findings, the pulse oximeter probe can be placed on the provider's finder to ensure functioning equipment.
Complications
Pulse oximeters are a noninvasive device and are very well tolerated. They are used in all age groups ranging from neonates to geriatric populations. Energy transfer to patients is low. While heat blisters with prolonged use of specific sensors are possible, most complaints come from allergic reactions to the adhesives or the mechanical adhesive properties of the single-use sensors. Pressure injury from clip sensors is possible but rare and can be minimized using adhesive probes. Generally, pulse oximeters are very well tolerated and have a very low risk of complication compared with arterial blood gas measurements.
Patient Safety and Education
No specific patient education is needed beyond explaining the sensor measures the oxygen level in the patient’s blood. The risk with these devices is minimal, as mentioned above. However, the care provider should instruct patients to report any discomfort experienced.
Clinical Significance
Pulse oximetry is part of standard intra-operative monitoring and is recommended by the ASA, the World Federation of Societies of Anesthesiologists, and the World Health Organization.[18] With the use of pulse oximeters as a standard of care for all patients receiving anesthesia, for several categories of patients in emergency and urgent care settings, and to monitor a significant percentage of hospitalized patients, the rate of undiagnosed hypoxic events leading to adverse outcomes has decreased significantly as we can monitor oxygen saturation continuously.[19] Evidence suggests using pulse oximetry in children reduces mortality rates when used in conjunction with oxygen administration.[20]
Spot checks in hospitalized patients are less optimal, as breathing and oxygenation are dynamic processes and can change rapidly. One challenge with employing devices that continuously monitor parameters is that healthcare professionals must monitor the device. Fortunately, sophisticated monitoring stations are available that alarm when a critical value is reached and can notify the patient care provider by phone or pager. Individualized alarm settings should be used for pulse oximeter alarm parameters to minimize false alarms and associated alarm fatigue.
Limitations of pulse oximetry include the inability to detect hyperoxemia and the inability to measure ventilation or arterial oxygen tension.
Interestingly, no clinical trials show a definitive benefit on mortality or resource allotment when pulse oximetry is utilized.
Media
(Click Image to Enlarge)
References
Checketts MR. AAGBI recommendations for standards of monitoring during anaesthesia and recovery 2015. Anaesthesia. 2016 Apr:71(4):470-1. doi: 10.1111/anae.13421. Epub [PubMed PMID: 26994537]
Merchant R, Chartrand D, Dain S, Dobson J, Kurrek M, LeDez K, Morgan P, Shukla R, Canadian Anesthesiologists' Society. Guidelines to the Practice of Anesthesia Revised Edition 2012. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2012 Jan:59(1):63-102. doi: 10.1007/s12630-011-9609-0. Epub [PubMed PMID: 22183296]
Taenzer AH, Pyke JB, McGrath SP, Blike GT. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010 Feb:112(2):282-7. doi: 10.1097/ALN.0b013e3181ca7a9b. Epub [PubMed PMID: 20098128]
Level 2 (mid-level) evidenceAgashe GS, Coakley J, Mannheimer PD. Forehead pulse oximetry: Headband use helps alleviate false low readings likely related to venous pulsation artifact. Anesthesiology. 2006 Dec:105(6):1111-6 [PubMed PMID: 17122573]
Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respiratory medicine. 2013 Jun:107(6):789-99. doi: 10.1016/j.rmed.2013.02.004. Epub 2013 Mar 13 [PubMed PMID: 23490227]
Level 3 (low-level) evidenceJubran A. Pulse oximetry. Critical care (London, England). 2015 Jul 16:19(1):272. doi: 10.1186/s13054-015-0984-8. Epub 2015 Jul 16 [PubMed PMID: 26179876]
Rackley CR. Monitoring During Mechanical Ventilation. Respiratory care. 2020 Jun:65(6):832-846. doi: 10.4187/respcare.07812. Epub [PubMed PMID: 32457174]
Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Medical devices (Auckland, N.Z.). 2014:7():231-9. doi: 10.2147/MDER.S47319. Epub 2014 Jul 8 [PubMed PMID: 25031547]
Tusman G, Bohm SH, Suarez-Sipmann F. Advanced Uses of Pulse Oximetry for Monitoring Mechanically Ventilated Patients. Anesthesia and analgesia. 2017 Jan:124(1):62-71 [PubMed PMID: 27183375]
Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM. Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia. Acta anaesthesiologica Scandinavica. 2009 Sep:53(8):1018-26. doi: 10.1111/j.1399-6576.2009.01968.x. Epub 2009 Apr 24 [PubMed PMID: 19397502]
Level 1 (high-level) evidenceHasanin A, Mohamed SAR, El-Adawy A. Evaluation of perfusion index as a tool for pain assessment in critically ill patients. Journal of clinical monitoring and computing. 2017 Oct:31(5):961-965. doi: 10.1007/s10877-016-9936-3. Epub 2016 Sep 24 [PubMed PMID: 27665572]
Hakverdioğlu Yönt G, Akin Korhan E, Dizer B. The effect of nail polish on pulse oximetry readings. Intensive & critical care nursing. 2014 Apr:30(2):111-5. doi: 10.1016/j.iccn.2013.08.003. Epub 2013 Sep 17 [PubMed PMID: 24054173]
Yek JLJ, Abdullah HR, Goh JPS, Chan YW. The effects of gel-based manicure on pulse oximetry. Singapore medical journal. 2019 Aug:60(8):432-435. doi: 10.11622/smedj.2019031. Epub 2019 Mar 11 [PubMed PMID: 30854571]
Jamali H, Castillo LT, Morgan CC, Coult J, Muhammad JL, Osobamiro OO, Parsons EC, Adamson R. Racial Disparity in Oxygen Saturation Measurements by Pulse Oximetry: Evidence and Implications. Annals of the American Thoracic Society. 2022 Dec:19(12):1951-1964. doi: 10.1513/AnnalsATS.202203-270CME. Epub [PubMed PMID: 36166259]
Piñero A, Illana J, García-Palenciano C, Cañizarese F, Canteras M, Cañadillas V, Durán E, Parilla P. Effect on oximetry of dyes used for sentinel lymph node biopsy. Archives of surgery (Chicago, Ill. : 1960). 2004 Nov:139(11):1204-7 [PubMed PMID: 15546820]
Level 1 (high-level) evidenceSidi A, Paulus DA, Rush W, Gravenstein N, Davis RF. Methylene blue and indocyanine green artifactually lower pulse oximetry readings of oxygen saturation. Studies in dogs. Journal of clinical monitoring. 1987 Oct:3(4):249-56 [PubMed PMID: 3681358]
Level 3 (low-level) evidencePoorzargar K, Pham C, Ariaratnam J, Lee K, Parotto M, Englesakis M, Chung F, Nagappa M. Accuracy of pulse oximeters in measuring oxygen saturation in patients with poor peripheral perfusion: a systematic review. Journal of clinical monitoring and computing. 2022 Aug:36(4):961-973. doi: 10.1007/s10877-021-00797-8. Epub 2022 Feb 4 [PubMed PMID: 35119597]
Level 1 (high-level) evidenceGelb AW, Morriss WW, Johnson W, Merry AF, Abayadeera A, Belîi N, Brull SJ, Chibana A, Evans F, Goddia C, Haylock-Loor C, Khan F, Leal S, Lin N, Merchant R, Newton MW, Rowles JS, Sanusi A, Wilson I, Velazquez Berumen A, International Standards for a Safe Practice of Anesthesia Workgroup. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Anesthesia and analgesia. 2018 Jun:126(6):2047-2055. doi: 10.1213/ANE.0000000000002927. Epub [PubMed PMID: 29734240]
Callahan JM. Pulse oximetry in emergency medicine. Emergency medicine clinics of North America. 2008 Nov:26(4):869-79, vii. doi: 10.1016/j.emc.2008.08.006. Epub [PubMed PMID: 19059087]
Enoch AJ, English M, Shepperd S. Does pulse oximeter use impact health outcomes? A systematic review. Archives of disease in childhood. 2016 Aug:101(8):694-700. doi: 10.1136/archdischild-2015-309638. Epub 2015 Dec 23 [PubMed PMID: 26699537]
Level 1 (high-level) evidence