Introduction
Heart disease represents a significant health problem and a leading cause of death worldwide. In 2016, nearly 300000 patients underwent cardiac surgery in the United States alone.[1] For a majority of these procedures, surgeons require an empty heart to operate on via the use of cardiopulmonary bypass (the "heart and lung machine"). To ensure the protection of the heart during cardiopulmonary bypass, administration and even distribution of cardioplegia solution to the myocardium is imperative. To accomplish this, a cardioplegia solution can be given anterograde, retrograde, or both. This article focuses on the relevant anatomy, applications, and complications of retrograde cardioplegia for cardiac surgery.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
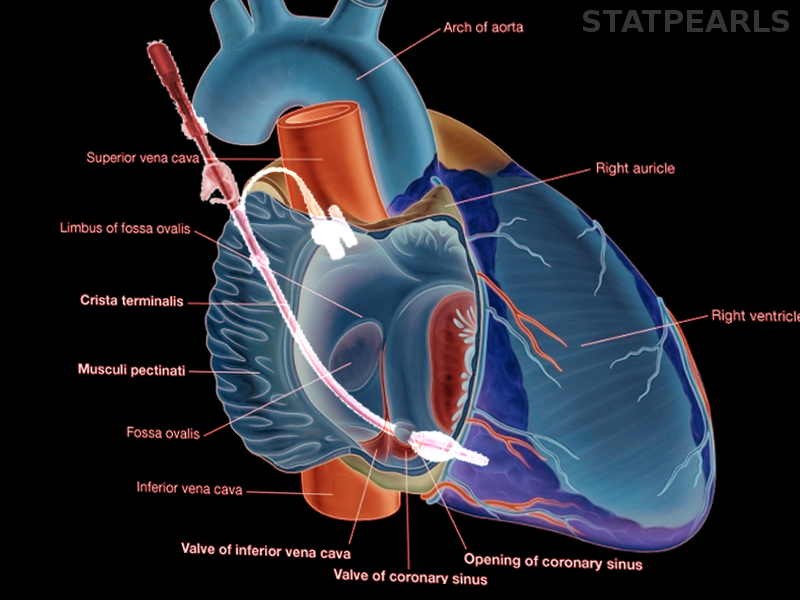
Originating from ostia in the aortic root, the coronary arteries supply freshly oxygenated blood to the myocardium. After utilization of this nutrient-rich blood, it is returned to the right side of the heart by three major routes.[2] The predominant avenue is the coronary sinus, which courses through the left atrial ventricular groove on the most posterior portion of the heart and drains directly into the right atrium. At the orifice of the coronary sinus as it opening into the right ventricle there is a valve known as the valve of Thebesius that must be crossed for placement of a coronary sinus catheter. The primary contributors to the coronary sinus are the small, middle, great and oblique cardiac veins. Other drainage routes of the myocardium include the anterior cardiac veins (which number between two and five) which drain into the right atrium, or the Thebesian veins, which carry blood from the myocardial wall back to the right ventricle.[3] On an even smaller scale, there also exist arteriovenous, venovenous, and venoluminal anastomoses, some of which originate from the myocardium of the right atrium and ventricle and do not drain directly into the coronary sinus.[4]
Indications
During the early era of surgery requiring cardiopulmonary bypass, cardioplegia was administered for myocardial protection only via the antegrade approach, through the aortic root or the coronary arteries directly. With experience, it became clear that coronary arterial stenoses limited the full spectrum of cardiologic protection desired.[5][6] Interest mounted in retrograde methods of preservation, that is, cardioplegia delivery by way of the coronary sinus. Technically, the aorta is first cannulated for arterial inflow. Then, the coronary sinus is accessed via a right atriotomy while the heart is still distended. A catheter housing a removable, malleable stylet is advanced through this atriotomy until resistance is met distally in the coronary sinus, and the stylet gently removed. Venous outflow cannulae are placed, the bypass is initiated, the aorta is cross-clamped, and cardioplegia delivered via the retrograde catheter.[7] There is a balloon near the distal tip of the retrograde cardioplegia catheter that is inflated before initial dosing to ensure cardioplegia travels in the retrograde direction. This is the reverse direction of normal flow of blood, hence the term retrograde. In specific circumstances (when there is no plan to enter the right atrium) a coronary sinus catheter can be placed percutaneously typically via a right internal jugular approach.
Contraindications
Before placement of a coronary sinus catheter to deliver retrograde cardioplegia it is important to review any imaging modalities available to ensure that there are no anatomical variants present. Specifically, a persistent left superior vena cava (PLSVC) can cause a significant problem with retrograde cardioplegia delivery. In PLSVC the left brachiocephalic vein does not develop and therefore the left arm/head/neck venous drainage returns through the PLSVC and into the coronary sinus. In patients with this anatomic variant, retrograde cardioplegia is not possible because the cardioplegia solution would not be traveling through just the coronary vessels and essentially given systemically.[8]
Equipment
A retrograde cardioplegia catheter is needed to provide retrograde cardioplegia. These catheters come in a variety of forms. They can be placed percutaneously (typically through a right internal jugular sheath) or via a right atriotomy by the surgeon. The catheter has an infusion port for the cardioplegia solution, a manometer to transduce pressures in the coronary sinus, and a balloon to occlude the coronary sinus to ensure that the cardioplegia runs retrograde.
Complications
The major complication of retrograde cardioplegia delivery is the risk of coronary sinus rupture. Despite this being a very rare event, it greatly increases the complexity of the original operation and extends a patients exposure to lengthened cardiopulmonary bypass times and increases their chances of poor cardiac protection during the procedure leading to potentially more adverse outcomes.
Clinical Significance
With growing experience using retrograde cardioplegia, numerous studies have shown that this technique (anterograde with retrograde cardioplegia) provides a superior return of myocardial function in the distribution of the occluded coronary vessels than with antegrade cardioplegia alone.[9][10] The analysis also shows that in this patient population that retrograde cardioplegia cools the myocardium more homogenously and may result in improved left ventricular systolic function in the early postoperative period.[11] Clearly established as the most vulnerable region of the myocardium to ischemia, the subendocardium is particularly vulnerable in the hypertrophied ventricle. Retrograde cardioplegia has been shown to be superior at protecting the hypertrophied subendocardium than antegrade cardioplegia alone.[12] Other advantages of the retrograde approach include an allowance for performing longer or more involved procedures with complete cardiac standstill. Through cannulation of the coronary sinus, clinicians can run a continuous infusion of cardioplegia and/or re-dose it at will; this is in contrast to antegrade cardioplegia, which may interrupt or interfere with the ongoing surgical intervention, specifically, those on the mitral valve, aortic valve or aortic root. During aortic valve procedures, retrograde cardioplegia allows flushing of debris from the coronary ostia, as well as de-airing of the coronaries and aortic root with the final dose.[13] During reoperations, old vein grafts may be severed and any distal embolic material flushed out of the coronaries and old grafts in a retrograde fashion.
Enhancing Healthcare Team Outcomes
In the operating room, retrograde cardioplegia monitoring is often via pressure monitoring. This pressure is displayed with the vital signs and often visible on a screen to all personnel in the operating room. All providers, nurses, techs, perfusionists, etc. should pay attention to this number at any time retrograde cardioplegia is in use. Since coronary sinus rupture being a catastrophic event, it is imperative to avoid such an outcome. It is essential to discuss the utilization of retrograde cardioplegia preoperatively so that the necessary equipment is available to include a catheter, cardioplegia solution, and monitoring equipment.
Media
References
D'Agostino RS, Jacobs JP, Badhwar V, Fernandez FG, Paone G, Wormuth DW, Shahian DM. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 Update on Outcomes and Quality. The Annals of thoracic surgery. 2018 Jan:105(1):15-23. doi: 10.1016/j.athoracsur.2017.10.035. Epub [PubMed PMID: 29233331]
Level 2 (mid-level) evidenceSingh JP, Houser S, Heist EK, Ruskin JN. The coronary venous anatomy: a segmental approach to aid cardiac resynchronization therapy. Journal of the American College of Cardiology. 2005 Jul 5:46(1):68-74 [PubMed PMID: 15992638]
Hochberg MS, Austen WG. Selective retrograde coronary venous perfusion. The Annals of thoracic surgery. 1980 Jun:29(6):578-8 [PubMed PMID: 6992722]
Level 3 (low-level) evidenceLazar HL. Coronary sinus interventions during cardiac surgery. The Annals of thoracic surgery. 1988 Oct:46(4):475-82 [PubMed PMID: 3052337]
Level 3 (low-level) evidenceHilton CJ, Teubl W, Acker M, Levinson HJ, Millard RW, Riddle R, McEnany MT. Inadequate cardioplegic protection with obstructed coronary arteries. The Annals of thoracic surgery. 1979 Oct:28(4):323-34 [PubMed PMID: 315762]
Level 3 (low-level) evidenceBecker H, Vinten-Johansen J, Buckberg GD, Follette DM, Robertson JM. Critical importance of ensuring cardioplegic delivery with coronary stenoses. The Journal of thoracic and cardiovascular surgery. 1981 Apr:81(4):507-15 [PubMed PMID: 7206757]
Level 3 (low-level) evidenceGundry SR,Sequiera A,Razzouk AM,McLaughlin JS,Bailey LL, Facile retrograde cardioplegia: transatrial cannulation of the coronary sinus. The Annals of thoracic surgery. 1990 Dec; [PubMed PMID: 2241379]
Fernando RJ, Johnson SD. Inability to Utilize Retrograde Cardioplegia due to a Persistent Left Superior Vena Cava. Case reports in anesthesiology. 2017:2017():4671856. doi: 10.1155/2017/4671856. Epub 2017 Dec 3 [PubMed PMID: 29333298]
Level 3 (low-level) evidenceGundry SR, Kirsh MM. A comparison of retrograde cardioplegia versus antegrade cardioplegia in the presence of coronary artery obstruction. The Annals of thoracic surgery. 1984 Aug:38(2):124-7 [PubMed PMID: 6465990]
Level 3 (low-level) evidenceHaan C, Lazar HL, Bernard S, Rivers S, Zallnick J, Shemin RJ. Superiority of retrograde cardioplegia after acute coronary occlusion. The Annals of thoracic surgery. 1991 Mar:51(3):408-12 [PubMed PMID: 1998417]
Level 3 (low-level) evidenceEhrenberg J,Intonti M,Owall A,Brodin LA,Ivert T,Lindblom D, Retrograde crystalloid cardioplegia preserves left ventricular systolic function better than antegrade cardioplegia in patients with occluded coronary arteries. Journal of cardiothoracic and vascular anesthesia. 2000 Aug; [PubMed PMID: 10972601]
Level 1 (high-level) evidenceGundry SR. Modification of myocardial ischemia in normal and hypertrophied hearts utilizing diastolic retroperfusion of the coronary veins. The Journal of thoracic and cardiovascular surgery. 1982 May:83(5):659-69 [PubMed PMID: 6210808]
Level 3 (low-level) evidenceEng J, Munsch C. Retrograde cardioplegia. Perfusion. 1992 Jan:7(1):7-12 [PubMed PMID: 10147698]
Level 3 (low-level) evidence