Introduction
Middle lobe syndrome (MLS) is a relatively uncommon clinical entity that is under-recognized in clinical practice. It was first identified clinically in 1948 by Graham et al. in a case series involving 12 patients with nontuberculous middle lobe atelectasis secondary to extensive compression by enlarged lymph nodes.[1] Recurrent or fixed right middle lobe opacification is almost pathognomonic for MLS; however, lingular involvement is common due to similar anatomic and physiological burdens. Though there has been no established definition of middle lobe syndrome, it has been recognized to involve two fundamentally different pathophysiological pathways that lead to recurrent middle lobe atelectasis: obstructive and nonobstructive.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The obstructive type of middle lobe syndrome usually results from extrinsic compression of the right middle lobe bronchus resulting from peribronchial lymphadenopathy or tumors that exploit the anatomic peculiarities of the right middle lobe bronchus[3]. It can classify into two subtypes: intraluminal or extraluminal obstruction.
Extrinsic compression may involve a plethora of tumors, including hamartomas, primary lung cancers, and distant metastasis from unknown primaries.[3][4] The most common etiology of the obstructive type is often subject to mediation by peribronchial lymphadenopathy secondary to granulomatous diseases, endemic fungal infections, and various mycobacterial species.[4][5][6][7][8] Other more exotic etiologies that cause an intraluminal obstruction, described in previous literature as isolated case reports, include sarcoidosis, aspiration, mucus plugs, and broncholiths.[9]
In the nonobstructive type, there is no identifiable obstruction on bronchoscopic evaluation, and the physiological basis of the recurrent atelectasis is poorly understood. The collateral ventilation of the middle lobe constitutes a zone of high resistance in comparison to the upper lobes, as a result of the higher ratio of pleural to the non-pleural surface area. The hypothesis is that ineffective collateral ventilation may play a significant role in the pathophysiology of middle lobe syndrome. Nonobstructive middle lobe syndrome is usually due to transient hypoventilation in the setting of chronic inflammatory and infectious changes (in conditions like cystic fibrosis) due to a wide array of infections, pulmonary infarcts, bronchopulmonary cysts, or disease processes that predispose to bronchiectasis.[10][9]
Epidemiology
Epidemiological data on middle lobe syndrome is very limited. There have been scattered case series and nationwide studies demonstrating a higher female to male ratio with women presenting later in age than their male counterparts.[9][11] Additionally, the poorly understood nonobstructive variant of middle lobe syndrome due to chronic inflammation is the most common etiology, accounting for over 60% of known cases.[3]
Pathophysiology
The pathophysiology of middle lobe syndrome varies by type. In obstructive middle lobe syndrome, there is a noticeable decrease in endoluminal diameter in the right middle lobe bronchus or left lingular bronchus due to extraluminal or intraluminal obstruction. The right middle lobe bronchus, in particular, is susceptible to near or total obstruction due to a smaller intraluminal diameter than other lobar bronchi.[12] Similarly, female patients have globally smaller intraluminal diameters compared to their male counterparts, thus providing anatomical evidence for a female predisposition epidemiologically.[12] Furthermore, the fissures of the middle lobe and lingula insulate these segments from collateral ventilation, thus reducing the likelihood of auto-correction of atelectasis and decreasing mucus clearance.[13][14]
History and Physical
A keen sense of awareness towards certain distinguishing features in the history and physical examination can raise the index of suspicion for diagnosis. The patients with middle lobe syndrome usually present with a constellation of symptoms such as chronic cough, hemoptysis, dyspnea, and features consistent with recurrent pneumonia. However, the most important aspect of history is an intrusive, recurrent, difficult to treat pneumonia. Physical exam findings would include wheezing, rhonchi, decreased breath sounds, tachypnea, and possibly diaphoresis during periods of concomitant pneumonia. In rare cases, features such as failure to thrive or cachexia may present as well, depending on the underlying etiology responsible for middle lobe syndrome.
Evaluation
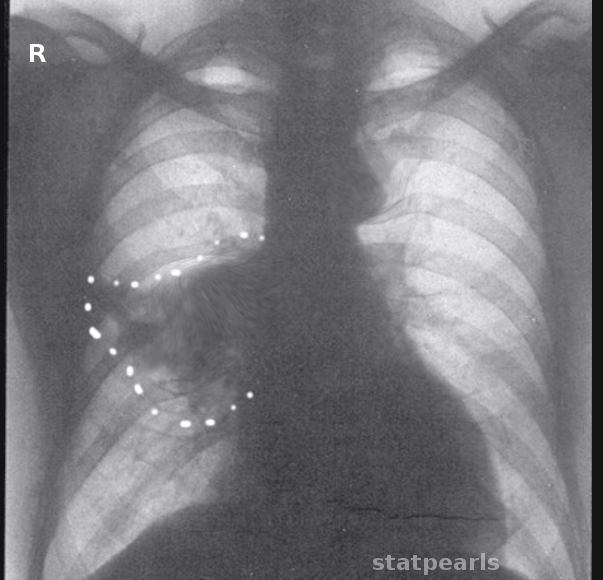
There is a myriad of tests and imaging modalities available to assist in the diagnosis of middle lobe syndrome; however, none is satisfactorily sensitive or specific enough to be considered the gold standard for diagnosis. Initial evaluation with a PA and lateral chest X-ray would seem appropriate; however, these plain films may be normal in patients who have intermittent obstructions or recurrent pneumonia.[2] The classic silhouette sign with the right heart border obscured by a right middle lobe infiltrate may be present in AP or PA projections.[13] Nevertheless, a radiographic evaluation may best focus on identifying the underlying cause of the condition. Bronchoscopy, complete blood count, and/or CT chest may further help elucidate the underlying disease process responsible for the syndrome.
Treatment / Management
Treatment for middle lobe syndrome, whether it is obstructive or non-obstructive, is directed at diagnosing and treating the underlying disease process. Agents directed towards optimizing pulmonary function (mucolytics, chest physiotherapy, bronchodilators, and antibiotics) are cornerstones of treatment and would most likely benefit all types of middle lobe syndrome irrespective of underlying etiology[15] Targeted antibiotic therapy towards Pseudomonas species is a strong recommendation, as the underlying structural changes associated with middle lobe syndrome enable it to be a viable medium for pseudomonal infections.(B2)
In obstructive type middle lobe syndrome, fiberoptic or rigid bronchoscopy would help remove foreign bodies or evaluate intrabronchial tumors. Clinicians have occasionally used insufflation with fiberoptic bronchoscopy for lobar collapse. However, there is no robust data regarding this approach, and it should only receive consideration on a case-by-case basis.[16][17] Ultimately, surgical intervention may play an essential role, if conservative and bronchoscopic management fails to produce favorable results. One study demonstrated that one-third of patients were successfully treated with conservative management, while one-third of patients went on to undergo surgical intervention.[18] The role of surgical intervention and possible lobectomy is only limited to obstructive MLS and data is limited to sporadic case reports in children. (B2)
Differential Diagnosis
Differentials include, but are not limited to cystic fibrosis, bronchiectasis, aspergillosis, pulmonary sequestration, tuberculosis infection, asthma, chronic obstructive pulmonary disease, immunodeficiency, ciliary disorders, and other rare causes.
Enhancing Healthcare Team Outcomes
Enhancing healthcare outcomes in middle lobe syndrome should primarily focus on the accurate detection of this condition. Pulmonologists should be actively involved in the management of patients with recurrent pneumonia or clinical suspicion of endobronchial obstruction, as their expertise with bronchoscopy may prove invaluable in the diagnosis and treatment of the underlying etiology. Patient education concerning pulmonary rehabilitation and chest physiotherapy may decrease the number of exacerbations.
Antibiotic stewardship is of particular importance in these patients as they often have infections with multidrug-resistant organisms that are difficult to treat; therefore, a pharmaceutical consult can be extremely helpful in this regard. Rapid de-escalation with appropriate cultures would be beneficial as it decreases the likelihood of subsequent multi-drug resistant infections. Coordination of pharmaceutical care with clinicians and pharmacists will result in better outcomes.
Nursing can assist the clinical team by providing patient counseling, monitor treatment progress, and report to the treating clinician any concerns. Nursing can also verify patient compliance with treatment, both drug and other therapies. Age-appropriate vaccinations and limiting exposure to caustic chemicals or smoking can help prevent this condition. This type of interprofessional team coordination is crucial to the successful treatment of middle lobe syndrome. [Level 5]
Media
References
GRAHAM EA, BURFORD TH, MAYER JH. Middle lobe syndrome. Postgraduate medicine. 1948 Jul:4(1):29-34 [PubMed PMID: 18874043]
Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: a review of clinicopathological features, diagnosis and treatment. Respiration; international review of thoracic diseases. 2012:84(1):80-6. doi: 10.1159/000336238. Epub 2012 Mar 1 [PubMed PMID: 22377566]
Wagner RB, Johnston MR. Middle lobe syndrome. The Annals of thoracic surgery. 1983 Jun:35(6):679-86 [PubMed PMID: 6344820]
Bertelsen S, Struve-Christensen E, Aasted A, Sparup J. Isolated middle lobe atelectasis: aetiology, pathogenesis, and treatment of the so-called middle lobe syndrome. Thorax. 1980 Jun:35(6):449-52 [PubMed PMID: 7434301]
Level 2 (mid-level) evidenceBradham RR, Sealy WC, Young WG Jr. Chronic middle lobe infection. Factors responsible for its development. The Annals of thoracic surgery. 1966 Jul:2(4):612-6 [PubMed PMID: 5934077]
Kim HC, Kim HS, Lee SJ, Jeong YY, Jeon KN, Lee JD, Hwang YS. Endobronchial tuberculosis presenting as right middle lobe syndrome: clinical characteristics and bronchoscopic findings in 22 cases. Yonsei medical journal. 2008 Aug 30:49(4):615-9. doi: 10.3349/ymj.2008.49.4.615. Epub [PubMed PMID: 18729304]
Level 3 (low-level) evidenceKinzy JD, Powers WP, Baddour LM. Case report: Blastomyces dermatitidis as a cause of middle lobe syndrome. The American journal of the medical sciences. 1996 Oct:312(4):191-3 [PubMed PMID: 8853069]
Level 3 (low-level) evidenceLambert GW, Baddour LM. Right middle lobe syndrome caused by Mycobacterium fortuitum in a patient with human immunodeficiency virus infection. Southern medical journal. 1992 Jul:85(7):767-9 [PubMed PMID: 1631699]
Level 3 (low-level) evidenceKwon KY, Myers JL, Swensen SJ, Colby TV. Middle lobe syndrome: a clinicopathological study of 21 patients. Human pathology. 1995 Mar:26(3):302-7 [PubMed PMID: 7890282]
Rua J, Marques R, Silva R, Gomes B, Fortuna J. Non-Obstructive Middle Lobe Syndrome: An Unusual Cause of Recurrent Pneumonia in an Elderly Woman. European journal of case reports in internal medicine. 2018:5(1):000737. doi: 10.12890/2017_000737. Epub 2018 Jan 31 [PubMed PMID: 30755973]
Level 3 (low-level) evidenceEinarsson JT, Einarsson JG, Isaksson H, Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: a nationwide study on clinicopathological features and surgical treatment. The clinical respiratory journal. 2009 Apr:3(2):77-81. doi: 10.1111/j.1752-699X.2008.00109.x. Epub [PubMed PMID: 20298381]
Level 2 (mid-level) evidenceMi W, Zhang C, Wang H, Cao J, Li C, Yang L, Guo F, Wang X, Yang T. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PloS one. 2015:10(4):e0123177. doi: 10.1371/journal.pone.0123177. Epub 2015 Apr 20 [PubMed PMID: 25894917]
McElvein RB, Mayo P. Middle lobe disease. Southern medical journal. 1967 Oct:60(10):1029-32 [PubMed PMID: 4863097]
Illamperuma C, Reid J, Kanthan R. Chyloptysis with right middle lobe syndrome complicated postoperatively by chylothorax: an unusual cause of right middle lobe syndrome. Canadian respiratory journal. 2009 Mar-Apr:16(2):e1-2 [PubMed PMID: 19399303]
Level 3 (low-level) evidencePriftis KN, Mermiri D, Papadopoulou A, Anthracopoulos MB, Vaos G, Nicolaidou P. The role of timely intervention in middle lobe syndrome in children. Chest. 2005 Oct:128(4):2504-10 [PubMed PMID: 16236916]
Level 2 (mid-level) evidencePaşaoğlu I, Doğan R, Demircin M, Hatipoğlu A, Bozer AY. Bronchoscopic removal of foreign bodies in children: retrospective analysis of 822 cases. The Thoracic and cardiovascular surgeon. 1991 Apr:39(2):95-8 [PubMed PMID: 1877059]
Level 2 (mid-level) evidenceWohlauer MV, Moore EE, Haenel JB, Burlew CC, Barnett CC Jr. Selective Intrabronchial Air Insufflation for Acute Lobar Collapse in the Surgical Intensive Care Unit. Journal of surgical radiology. 2011 Apr 1:2(2):178-180 [PubMed PMID: 21687834]
Livingston GL, Holinger LD, Luck SR. Right middle lobe syndrome in children. International journal of pediatric otorhinolaryngology. 1987 Jun:13(1):11-23 [PubMed PMID: 3623806]
Level 2 (mid-level) evidence