Introduction
Sacroiliac (SI) joint pain is a common etiology of low back pain. Studies have shown that 10% to 27% of mechanical low back pain is secondary to SI joint pain. [1][2] It can occur with or without lower extremity pain. Dysfunction of the SI joint occurs with degenerative conditions or with an imbalance between the SI joints. Patients with true and apparent leg length discrepancy, advanced age, inflammatory arthritis, pregnancy, trauma, and previous spine surgery are at increased risk of SI joint pain. [3][4][5] Classically, SI joint pain is often reported as pain below L5, and certain physical exam maneuvers such as FABER, Gaenslen’s, and compression tests can elicit pain stemming from SI joint dysfunction. If SI joint pain is bilateral and symmetric, then a suspicion for inflammatory causes such as ankylosing spondylitis should be raised. When indicated, a SI joint injection is used to aid the diagnosis and treat of SI joint pain. This procedure involves introducing a local anesthetic or a mixture of local anesthetic and corticosteroids into the SI joint. Once sustained and adequate pain relief is achieved, the patient can return to normal function or a physical therapy regimen can be implemented.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The human body has two SI joints, situated between the ilium and sacrum on each side of the body. The SI joint is auricular and has characteristics of both diarthrosis and synarthrosis joints. The ligaments form a capsule that follows its auricular margin, with an extracapsular articulation between the sacrum and ilia supported by the interosseous sacroiliac ligament. During pregnancy, relaxin is released, and this can cause the ligaments to loosen. The SI joint innervation is complex, and conflicting information exists. According to some sources, the sensory fibers constitute the lateral branches of the posterior rami of L5 through S4, which serve as the pain generators for the joint. [6] While the main purpose of the SI joint is to supply stability and to decrease the forces transmitted from the lower extremities, the SI joint does have limited motion, with an average range of 2 degrees in both planes, according to one analysis. [7] The SI joint motions include anterior and posterior innominate tilt of the pelvis on the sacrum. There is also the motion of nutation, where the sacrum moves anteriorly and inferiorly while the coccyx moves posteriorly relative to the ilium, and counternutation, where the sacrum moves posteriorly and superiorly while the coccyx moves anteriorly relative to the sacrum.
Indications
SI joint injection can be used for both the diagnosis and treatment of SI joint pain. A thorough history physical examination including provocative tests is performed for an accurate diagnosis. Typically, if a patient has a positive response to 3 or more SI joint provocative tests, a positive outcome of a diagnostic SI joint block can be predicted. If there is a high suspicion of SI joint pain, SI joint diagnostic injection is indicated.
In diagnostic blocks, an anesthetic is injected into the SI joint, and if the patient experiences 75% of pain relief while performing previously painful movements for the duration of the anesthetic, then the diagnosis of SI joint dysfunction can be established. [8]
Therapeutically, a local anesthetic is combined with corticosteroid medication to provide pain relief in the SI joint. Therapeutic SI joint injections can be intraarticular or periarticular, and increasing research suggests that intraarticular therapeutic injections are superior to periarticular injections.
Contraindications
Absolute contraindications of SI joint injections include:
- Patient-reported or documented history of allergic reaction to cortisone injections
- Local malignancy
Relative contraindications include:
- Coagulopathy or current/recent use of blood-thinning agents
- Pregnancy
- Systemic infection, septic joint, or osteomyelitis
- Diabetes Mellitus, Type II, with a history of poor glycemic control
Equipment
Ideally, fluoroscopic guided SI joint injections require a fluoroscopic C-arm device, local anesthetic (lidocaine or bupivacaine), corticosteroids (triamcinolone, methylprednisolone, betamethasone or dexamethasone), contrasts solution, sterile gloves, and drapes, betadine solution. The injection also requires a 25-gauge, 5-inch, styletted spinal needle. If the joint is degenerative and sclerotic, a 22-gauge needle may be utilized.
Personnel
Personnel includes a physician or physician-extender (i.e. Physician Assistant, Nurse Practitioner, Resident, Fellow, etc), an assistant, and a fluoroscopic C-arm operator. Staff members should be familiar with the handling of potential complications. If a CT-guided injection is being performed, then a CT technician plays a role in image acquisition.
Preparation
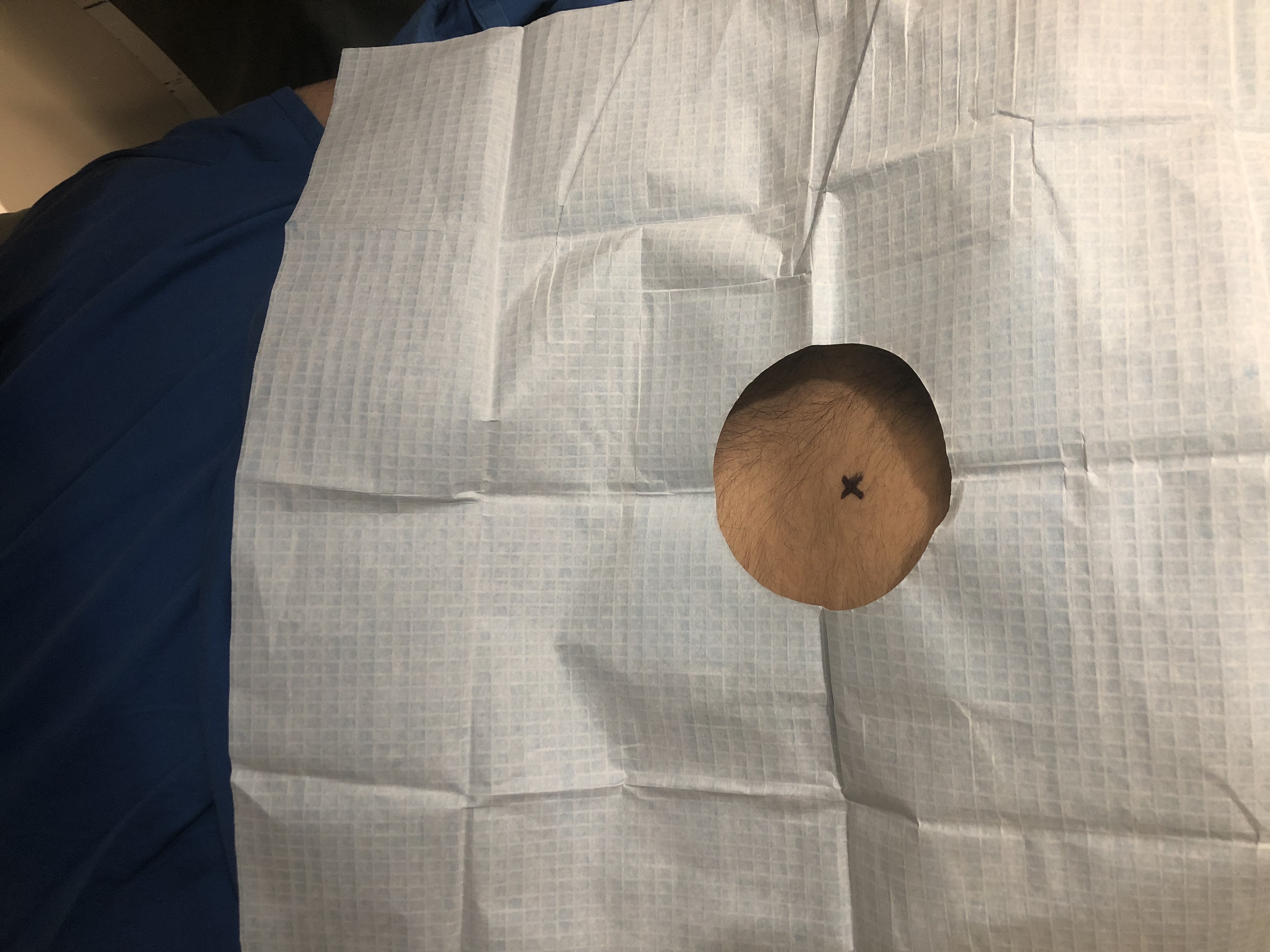
Patient consent of the injection is obtained after the risk and benefits are thoroughly explained and discussed with the patient. Time-out is used to verify the patient and site of injection prior to the procedure. The patient is to lie prone, and the identification of the SI joint may commence.
Technique or Treatment
Fluoroscopic Guidance
According to the practice guidelines from the International Spine Intervention Society (ISIS), a patient is prepped and placed in a prone position, and a pillow is placed under the abdomen at the level of the iliac crests. To visualize the inferior portion of the SI joint, the C-arm is initially placed in anterior-posterior (AP) view and maybe adjusted laterally or medially until the optimal image is obtained. When the bony planes of the inferior portion of the joints are parallel, the image is considered ideal.
The aforementioned identified area is then marked and sterilized and draped. With intermittent fluoroscopy, the spinal needle is advanced to the inferior part of the SI joint. Once the needle reaches the joint, a distinct popping sensation can be felt by the physician. Once optimal needle position is achieved within the inferior portion of the SI joint, 0.3 to 0.5 ml of contrast is injected into the joint. If the contrast material outlines the SI joint, the placement of the needle is confirmed. There is controversy on the maximum volume of injectate to be used; however, as a rule of thumb, the injectate should be used until there is a firm end-point, extra-capsular escape, or a maximum volume of 2.5 ml is reached.
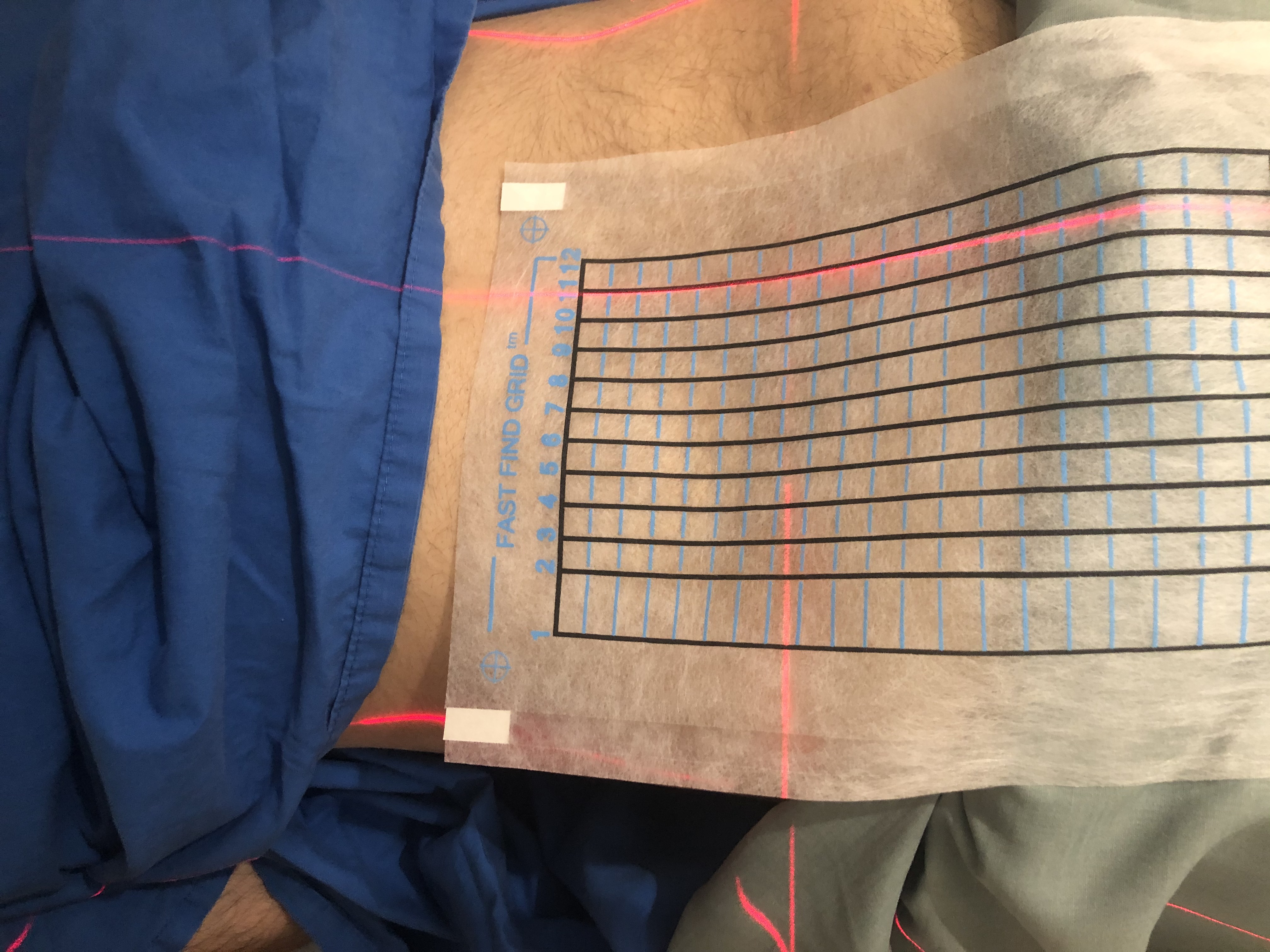
CT Guidance
CT guidance is also performed with the patient in a prone position. An initial CT scan is performed and the most direct route to the SI joints bilaterally is identified. The overlying skin is marked. The skin is prepped and draped in a sterile fashion. Local anesthesia with approximately 5 mL of 1% lidocaine is administered. Using CT guidance, a 22 gauge spinal needle is inserted into the lower posterior aspect of the SI joints. After confirming the satisfactory placement of the spinal needles, 0.5 mL of Kenalog 40 (20 mg) mixed with 0.5 mL of 0.25% bupivacaine is injected into each SI joint. The needles were removed and hemostasis is achieved with compression.
Complications
According to a systematic review, a minority of patients experienced immediate transient reactions, such as vasovagal reactions. [9] The most common being increased pain and soreness. [10] Rarer, but more serious, complications include trauma to the nerves, accidental intervertebral foraminal injection, hematoma, sciatic palsy, meningitis, abscess, and systematic infection. There is also a reported case of pyogenic sacroiliitis and a case of herpes simplex.[11] There may also be a risk posed by the administration of steroids and local anesthetics. A technically unsuccessful rate of 10% has been reported by several studies.[12][13][14][15]
Clinical Significance
Where there is suspicion for SI joint pain, SI joint blocks are used to diagnose and treat SI joint pain. While SI joint injections can be performed without imaging guidance, according to various studies, there is only a 12% to 22% chance of the needle reaching the SI joint without imaging guidance. Other imaging guidance modalities include ultrasound or CT. When compared to ultrasound guidance, fluoroscopy can confirm injectate being placed intraarticularly, and fluoroscopy is better than CT imaging at visualizing the medicine’s spread from the joint to the surrounding structures.
With diagnostic SI joint injections, when there is more than 75% pain relief while performing previously painful movements, the SI block is deemed successful. Certain physicians may decide also to perform a controlled (dual) local anesthetic block to rule out false positives. [16] There is systematic review evidence that offers moderate support for the use of SI joint injection in chronic low back pain and/or lower extremity pain below the L5 vertebra. Therapeutic SI joint injection can provide prolonged pain relief for patients suffering from SI joint dysfunction. According to one study, SI joint injection with triamcinolone was given to patients with SI joint dysfunction with spondyloarthropathy, demonstrated to reduce pain for more than 6 weeks for 66.7% of participants, and the overall mean duration of pain reduction in these responders was 36.8 plus or minus 9.9 weeks. [17] If steroid injection does not alleviate pain adequately, other interventions may be considered, including prolotherapy, radiofrequency ablation, viscosupplementation, or minimally invasive SI joint fusion.
Enhancing Healthcare Team Outcomes
SI joint injection may be performed by an interprofessional team that includes a pain specialist, radiologist, orthopedic surgeon, rheumatologist and sports physician. It is important to be aware of the anatomy of the SI joint and utilize imaging modalities to achieve higher success. Patients should be educated that the SI injection is not curative and repeat injections may be required. All healthcare workers who perform SI injections should know how to manage the complications that may arise during and after the procedure.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Navani A, Manchikanti L, Albers SL, Latchaw RE, Sanapati J, Kaye AD, Atluri S, Jordan S, Gupta A, Cedeno D, Vallejo A, Fellows B, Knezevic NN, Pappolla M, Diwan S, Trescot AM, Soin A, Kaye AM, Aydin SM, Calodney AK, Candido KD, Bakshi S, Benyamin RM, Vallejo R, Watanabe A, Beall D, Stitik TP, Foye PM, Helander EM, Hirsch JA. Responsible, Safe, and Effective Use of Biologics in the Management of Low Back Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain physician. 2019 Jan:22(1S):S1-S74 [PubMed PMID: 30717500]
Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR, Colson JD, Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain physician. 2007 Jan:10(1):165-84 [PubMed PMID: 17256029]
Level 1 (high-level) evidenceHuynh P, Hsu D. Comparison of Lateral Branched Pulsed Radiofrequency Denervation and Intraarticular Depot Methylprednisolone Injection for Sacroiliac Joint Pain: Inquiry for Additional Investigation. Pain physician. 2019 Jan:22(1):E53-E54 [PubMed PMID: 30700079]
Kim DK,McKenzie GA, Accessory Sacroiliac Joint Injection for Relief of Buttock Pain. Pain medicine (Malden, Mass.). 2019 Jan 8; [PubMed PMID: 30624698]
Kancherla VK, McGowan SM, Audley BN, Sokunbi G, Puccio ST. Patient Reported Outcomes from Sacroiliac Joint Fusion. Asian spine journal. 2017 Feb:11(1):120-126. doi: 10.4184/asj.2017.11.1.120. Epub 2017 Feb 17 [PubMed PMID: 28243380]
Cox RC, Fortin JD. The anatomy of the lateral branches of the sacral dorsal rami: implications for radiofrequency ablation. Pain physician. 2014 Sep-Oct:17(5):459-64 [PubMed PMID: 25247902]
Goode A, Hegedus EJ, Sizer P, Brismee JM, Linberg A, Cook CE. Three-dimensional movements of the sacroiliac joint: a systematic review of the literature and assessment of clinical utility. The Journal of manual & manipulative therapy. 2008:16(1):25-38 [PubMed PMID: 19119382]
Level 1 (high-level) evidencePolly D, Cher D, Whang PG, Frank C, Sembrano J, INSITE Study Group. Does Level of Response to SI Joint Block Predict Response to SI Joint Fusion? International journal of spine surgery. 2016:10():4. doi: 10.14444/3004. Epub 2016 Jan 21 [PubMed PMID: 26913224]
Kennedy DJ, Schneider B, Casey E, Rittenberg J, Conrad B, Smuck M, Plastaras CT. Vasovagal rates in flouroscopically guided interventional procedures: a study of over 8,000 injections. Pain medicine (Malden, Mass.). 2013 Dec:14(12):1854-9. doi: 10.1111/pme.12241. Epub 2013 Oct 4 [PubMed PMID: 24118835]
Level 2 (mid-level) evidencePlastaras CT, Joshi AB, Garvan C, Chimes GP, Smeal W, Rittenberg J, Lento P, Stanos S, Fitzgerald C. Adverse events associated with fluoroscopically guided sacroiliac joint injections. PM & R : the journal of injury, function, and rehabilitation. 2012 Jul:4(7):473-8. doi: 10.1016/j.pmrj.2012.02.001. Epub 2012 Apr 28 [PubMed PMID: 22543036]
Level 2 (mid-level) evidenceMeydani A, Schwartz RA, Foye PM, Patel AD. Herpes simplex following intra-articular sacroiliac corticosteroid injection. Acta dermatovenerologica Alpina, Pannonica, et Adriatica. 2009 Sep:18(3):135-7 [PubMed PMID: 19784528]
Level 3 (low-level) evidenceHong SH, Chung H, Lee CH, Kim YH. A Prospective Randomized Noninferiority Trial Comparing Upper and Lower One-Third Joint Approaches for Sacroiliac Joint Injections. Pain physician. 2018 May:21(3):251-258 [PubMed PMID: 29871369]
Level 1 (high-level) evidencePolly DW Jr. The Sacroiliac Joint. Neurosurgery clinics of North America. 2017 Jul:28(3):301-312. doi: 10.1016/j.nec.2017.03.003. Epub [PubMed PMID: 28600004]
Nagpal G, Flaherty JP, Benzon HT. Diskitis, Osteomyelitis, Spinal Epidural Abscess, Meningitis, and Endocarditis Following Sacroiliac Joint Injection for the Treatment of Low-Back Pain in a Patient on Therapy for Hepatitis C Virus. Regional anesthesia and pain medicine. 2017 Jul-Aug:42(4):517-520. doi: 10.1097/AAP.0000000000000608. Epub [PubMed PMID: 28492440]
Kurosawa D, Murakami E, Ozawa H, Koga H, Isu T, Chiba Y, Abe E, Unoki E, Musha Y, Ito K, Katoh S, Yamaguchi T. A Diagnostic Scoring System for Sacroiliac Joint Pain Originating from the Posterior Ligament. Pain medicine (Malden, Mass.). 2017 Feb 1:18(2):228-238. doi: 10.1093/pm/pnw117. Epub [PubMed PMID: 28204687]
Jung MW, Schellhas K, Johnson B. Use of Diagnostic Injections to Evaluate Sacroiliac Joint Pain. International journal of spine surgery. 2020 Feb:14(Suppl 1):30-34. doi: 10.14444/6081. Epub 2020 Feb 10 [PubMed PMID: 32123655]
Scholten PM, Patel SI, Christos PJ, Singh JR. Short-term efficacy of sacroiliac joint corticosteroid injection based on arthrographic contrast patterns. PM & R : the journal of injury, function, and rehabilitation. 2015 Apr:7(4):385-91. doi: 10.1016/j.pmrj.2014.10.007. Epub 2014 Oct 29 [PubMed PMID: 25452127]
Level 2 (mid-level) evidence