Introduction
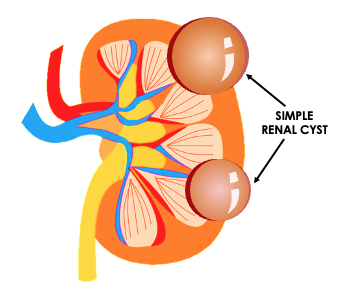
A simple kidney cyst is a pocket of fluid that originates from the surface of the kidney and is contained by a thin wall. One or more simple cysts may form within the kidneys.[1][2][3] The simple cyst is the most common type of renal cyst.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Simple renal cysts are acquired, not inherited.[4] The exact cause is unknown. Risk factors are advancing age and male sex. The presence of simple cysts increases after age 40. Renal cysts are most often identified at autopsy or incidentally in radiological studies.
Epidemiology
Simple renal cysts are extremely common, and the incidence increases with age. Approximately 25% of people who are 40 years or older and approximately 50% of people 50 years and older have simple kidney cysts. Simple renal cysts can double in size over 10 years. Solitary renal cysts are usually incidentally discovered and are typically asymptomatic. Multiple renal cysts are often seen in patients with chronic renal disease on dialysis.
Pathophysiology
The exact pathophysiology for renal cysts is unclear. Diverticula on the distal tubule of the nephron may be the starting point for cyst formation. The basal membrane involution with age, combined with a degree of urinary obstruction, may result in simple cyst formation.
Histopathology
Simple renal cysts are typically filled with serous fluid and have a simple epithelial lining. They can have a single layer of cuboidal or flattened epithelial. A simple cyst can have an atrophic epithelial layer.
History and Physical
Simple cysts typically do not cause any symptoms. They are most often detected incidentally during a radiological study performed for other reasons such as abdominal pain. Simple cysts usually do not interfere with kidney function and do not typically affect renal function tests. On rare occasions, simple cysts can lead to impaired renal function. Most people are not aware of having them. Rarely, a simple cyst can rupture and bleed, become infected, or grow so large that it causes a mass effect on other organs and abdominal pain and discomfort. There is an association between simple cysts and high blood pressure, but a causal relationship has not been proven.
Evaluation
Renal cysts are often detected incidentally during a CT scan or ultrasound. The sonographic features of a simple cyst are as follows: anechoic, thin imperceptible wall, and no internal septations or debris.[5][6][7]
On non-contrast, unenhanced CT scan, a simple cyst can be confidently diagnosed if the cyst measures simple fluid of 20 Hounsfield units or less, has no septations, and has no central or peripheral calcification, and has a thin wall. On a contrast-enhanced CT Scan, a simple cyst is diagnosed if there is no enhancement, it measures the simple fluid, has a thin wall, and contains no calcifications.[8][9]
MRI features of a simple cyst are as follows: homogeneously low signal intensity on T1 weighted imaged, homogeneously high signal intensity on T2 weighted images, and no demonstrable enhancement after IV contrast. Subtraction images can be helpful in difficult cases of questionable enhancement.
Treatment / Management
The majority of cysts do not need any intervention or follow-up. If a cyst becomes infected, antibiotics are necessary. If a cyst is so large that it is exerting mass effect or pressure on another organ, the two most common procedures for treating simple kidney cysts are (1) aspiration and sclerotherapy and (2) laparoscopic surgery to remove the cyst. Ethanol is most commonly used in sclerotherapy.[10][11]
Cyst aspiration without sclerotherapy has a high recurrence rate ranging from 20% to 80%. Simple cysts are not treated with surgical exploration.
Differential Diagnosis
Complex renal cysts need to be differentiated based on imaging criteria to assess the risk of malignancy. In 1986, Morton Bosniak developed a classification of renal cysts based on CT findings that have become the standard to ascertain which complex cysts have a high incidence of malignancy and require surgery or close follow-up imaging. The Bosniak classification is currently used by both radiologists and urologists to manage complex renal cysts. It was originally based on CT findings but has been expanded to MR imaging findings as well. Simple cysts fall into the Bosniak category 1 and do not require further workup or imaging.
To evaluate complex renal cysts by CT scan or MRI, it is imperative to obtain the scan through the kidneys before IV contrast and after IV contrast during the same exam with the same parameters. The Bosniak classification system is used to guide treatment.
Bosniak I Lesions
- Simple cysts
- Water density is 0 to 20 Hounsfield units
- Homogenous
- Have a thin wall
- No enhancement after IV contrast
Treatment: Bosniak lesions in category I are benign cysts and do not require further imaging or intervention.
Bosniak II Lesions
- Complex cysts
- It can have thin hairline septa and thin calcification in the septa or wall.
- No demonstrable enhancement after IV contrast on CT or MRI.
- It can have a homogenously high attenuation on CT scan
- It can have a uniformly high signal intensity on T1 weighted images and a uniformly low signal intensity on T2 weighted images.
- Lesions measure less than 3 cm in diameter.
Treatment: Bosniak lesions in category II are benign cysts and do not require further imaging or intervention.
Bosniak IIF lesions
- Complex renal cysts with multiple thin enhancing septations
- Can have thick nodular calcifications
- Can have minimal (10-15 Hounsfield unit) enhancement on CT scan after IV contrast
Treatment: For Bosniak lesions category IIF, the F stands for follow-up. Follow-up cross-sectional imaging with IV contrast is recommended at 6 months, 12 months, and then yearly for 5 years. If the lesions grow in size and develop internal enhancing soft tissue, they become category III lesions and require surgical treatment or ablation therapy.
Bosniak III lesions
- Renal lesions which show internal enhancement after IV contrast on CT scan
- Typically enhancing greater than 15 Hounsfield units
- Thick, irregular enhancing walls and/or
- Thick enhancing internal septations.
Treatment: Bosniak lesions category III require excision or can be treated with ablation therapy. They have a 50% to 80% chance of malignancy.
Bosniak IV lesions
- Distinctly malignant
- Clearly enhancing internal soft tissue
Treatment: Bosniak lesions category IV require excision or can be treated with ablation therapy. Bosniak category IV lesions have a greater than 90% chance of malignancy.
Surgical Oncology
Surgical exploration and treatment of simple renal cysts are no longer employed.
Radiation Oncology
Radiation therapy is not a treatment for simple cysts.
Prognosis
Simple cysts do not affect mortality or morbidity.
Complications
Rarely, simple cysts can become infected and require antibiotic treatment.
Also, simple cysts rarely become so large as to cause mass effect on other organs and block the flow of urine. This would require drainage of the cyst with sclerotherapy or laparoscopic removal with surgery.
Enhancing Healthcare Team Outcomes
The primary care provider and nurse practitioner may come across a patient with a renal cyst detected on an incidental imaging study. These patients should be referred to a urologist and radiologist for management. Most small asymptomatic cysts do not need treatment. Large cysts that affect renal function may be aspirated or removed via laparoscopic surgery. The outlook for most patients is excellent.[12]
Media
References
Rediger C, Guerra LA, Keays MA, Wayne C, Reddy D, Ksara S, Leonard MP. Renal cyst evolution in childhood: a contemporary observational study. Journal of pediatric urology. 2019 Apr:15(2):188.e1-188.e6. doi: 10.1016/j.jpurol.2019.01.006. Epub 2019 Feb 1 [PubMed PMID: 30808538]
Level 2 (mid-level) evidenceBrownstein AJ, Bin Mahmood SU, Saeyeldin A, Velasquez Mejia C, Zafar MA, Li Y, Rizzo JA, Dahl NK, Erben Y, Ziganshin BA, Elefteriades JA. Simple renal cysts and bovine aortic arch: markers for aortic disease. Open heart. 2019:6(1):e000862. doi: 10.1136/openhrt-2018-000862. Epub 2019 Jan 28 [PubMed PMID: 30774963]
Sanna E, Loukogeorgakis S, Prior T, Derwig I, Paramasivam G, Choudhry M, Lees C. Fetal abdominal cysts: antenatal course and postnatal outcomes. Journal of perinatal medicine. 2019 May 27:47(4):418-421. doi: 10.1515/jpm-2018-0311. Epub [PubMed PMID: 30763268]
Ferro F, Vezzali N, Comploj E, Pedron E, Di Serafino M, Esposito F, Pelliccia P, Rossi E, Zeccolini M, Vallone G. Pediatric cystic diseases of the kidney. Journal of ultrasound. 2019 Sep:22(3):381-393. doi: 10.1007/s40477-018-0347-9. Epub 2019 Jan 1 [PubMed PMID: 30600488]
Gimpel C, Avni EF, Breysem L, Burgmaier K, Caroli A, Cetiner M, Haffner D, Hartung EA, Franke D, König J, Liebau MC, Mekahli D, Ong ACM, Pape L, Titieni A, Torra R, Winyard PJD, Schaefer F. Imaging of Kidney Cysts and Cystic Kidney Diseases in Children: An International Working Group Consensus Statement. Radiology. 2019 Mar:290(3):769-782. doi: 10.1148/radiol.2018181243. Epub 2019 Jan 1 [PubMed PMID: 30599104]
Level 3 (low-level) evidenceKennedy-Snodgrass C, Keenan V, Katz DS. Infected Renal Cyst as a Complication of Dropped Gallstones during Laparoscopic Cholecystectomy. Case reports in gastrointestinal medicine. 2018:2018():2478245. doi: 10.1155/2018/2478245. Epub 2018 Sep 30 [PubMed PMID: 30405920]
Level 3 (low-level) evidenceNelson SM, Oettel DJ, Lisanti CJ, Schwope RB, Timpone VM. Incidental Renal Lesions on Lumbar Spine MRI: Who Needs Follow-Up? AJR. American journal of roentgenology. 2019 Jan:212(1):130-134. doi: 10.2214/AJR.18.20079. Epub 2018 Nov 7 [PubMed PMID: 30403526]
Eroglu FK, Kargın Çakıcı E, Can G, Güngör T, Yazılıtaş F, Kurt-Sukur ED, Celikkaya E, Üner Ç, Çakmakçı E, Bülbül M. Retrospective analysis of simple and stage II renal cysts: Pediatric nephrology point of view. Pediatrics international : official journal of the Japan Pediatric Society. 2018 Dec:60(12):1068-1072. doi: 10.1111/ped.13714. Epub [PubMed PMID: 30320940]
Level 2 (mid-level) evidenceLi Y, Dai C, Bian T, Zhou J, Xiang Z, He M, Huang J, Zhu Y, Hu X, Jiang S, Guo J, Wang H. Development and prospective validation of a novel weighted quantitative scoring system aimed at predicting the pathological features of cystic renal masses. European radiology. 2019 Apr:29(4):1809-1819. doi: 10.1007/s00330-018-5722-6. Epub 2018 Oct 11 [PubMed PMID: 30311030]
Level 1 (high-level) evidenceAl-Otaibi K. Complications of 411 laparoscopic urological procedures: A single surgeon experience. Urology annals. 2018 Jul-Sep:10(3):308-312. doi: 10.4103/UA.UA_190_17. Epub [PubMed PMID: 30089991]
Marte A, Pintozzi L. Laparoscopic treatment of symptomatic simple renal cysts in children: single-center experience. La Pediatria medica e chirurgica : Medical and surgical pediatrics. 2018 May 24:40(1):. doi: 10.4081/pmc.2018.168. Epub 2018 May 24 [PubMed PMID: 29871474]
Esposito C, Escolino M, Troncoso Solar B, Iacona R, Esposito R, Settimi A, Mushtaq I. Diagnosis and long-term outcome of renal cysts after laparoscopic partial nephrectomy in children. BJU international. 2017 May:119(5):761-766. doi: 10.1111/bju.13698. Epub 2016 Nov 14 [PubMed PMID: 27779799]