Introduction
Sinus arrhythmia is a commonly encountered variation of normal sinus rhythm. Sinus arrhythmia characteristically presents with an irregular rate in which the variation in the R-R interval is greater than 0.12 seconds. Additionally, P waves are typically monoform and in a pattern consistent with atrial activation originating from the sinus node. During respiration, intermittent vagus nerve activation occurs, which results in beat-to-beat variations in the resting heart rate. When present, sinus arrhythmia typically indicates good cardiovascular health.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Sinus arrhythmia is a common rhythm variation. It is seen more often in children and young adults. Respirations lead to vagal stimuli, resulting in R-R interval variations. Typically, its presence is an indicator of good cardiovascular health. Loss of sinus arrhythmia may indicate underlying heart failure or structural heart disease.
Epidemiology
Sinus arrhythmia is most typically present in young, healthy individuals. Studies have attempted to establish an increased prevalence in patients with underlying hypertension, obesity, and diabetes. A published study in 2002 in the Journal of the American College of Cardiology suggested that sinus arrhythmia appeared less prominent in older individuals. The study evaluated 2 groups of healthy individuals without underlying cardiovascular disease. The first group evaluated patients between 50 and 71; the second was patients under 31. Investigators found that the prevalence of respiratory sinus arrhythmia in older individuals was less than 20 percent of that in those less than 31 years of age. Some suspect this is due to age-related changes in the compliance of arterial walls and diminished vagal responses.[1]
Pathophysiology
Investigation of the pathogenesis of sinus arrhythmia continues, but 3 main theorized mechanisms exist now. These include respiratory-phasic, nonrespiratory-nonphasic, and nonrespiratory-ventriculophasic sinus arrhythmia.
Respiratory-Phasic
Respiratory sinus arrhythmia is a common finding. It is a normal alteration in cardiac rhythm generated from the vagus nerve stimulation and changes in cardiac filling pressures during respiration. Recently, there has been controversy regarding the underlying pathogenesis of sinus arrhythmia. Some studies have begun to associate sinus rhythm with obesity, diabetes mellitus, and hypertension, while others continue to support a reduction in sinus arrhythmia when these conditions are present. Some studies suggest there may be some relationship between heart failure and other systemic conditions.
One study attempted to evaluate the influences of vagal and sympathetic efferent activity on sinus arrhythmia by administering hyoscine butylbromide and atenolol. Administration of hyoscine butylbromide reduced sinus arrhythmia, while atenolol reduced vagal tone, prolonging the mean R-R and increasing sinus arrhythmia. The study suggested that mediation of sinus arrhythmia occurs through vagal stimulation.[2] During the respiratory cycle, inspiration inhibits vagal tone, increasing sinus rate, while expiration increases vagal tone, resulting in a decreased rate. This concept was supported by a later study that successfully mimicked the respiratory cycle via stimulation of baroreceptors in the carotid artery with cycles of phased neck suction at the frequency of normal respiration. The study suggested that baroreceptor signaling is important in generating respiratory sinus arrhythmia.[3] More recently, investigators have evaluated the effects of diabetes mellitus on sinus arrhythmia. They found that in patients with diabetes, there is a reduction in sinus arrhythmia, which investigators attributed to the autonomic effects of the disease.[4]
Nonrespiratory
In nonrespiratory sinus arrhythmia, electrocardiograms appear similar to the respiratory type. The 2 differ because nonrespiratory sinus arrhythmia is unrelated to the respiratory cycle. While it can occur within healthy individuals, this type often correlates with underlying pathology.[5] Some have reported this finding with underlying heart disease or associated with digitalis overdose. One case report associated the finding with a traumatic intracerebral hemorrhage, which authors associated with vasospasm, hypoxia, or increased intracranial pressure.[6]
Ventriculophasic
When present, ventriculophasic sinus arrhythmia typically occurs in patients with third-degree AV block. However, it demonstrates correlations between premature ventricular contractions. Currently, theorized mechanisms suggest that ventriculophasic sinus arrhythmia results from prolonged cardiac filling and increased stroke volume. The increased stroke volume triggers a carotid baroreceptor response. On EKG, this is represented by an interval shortening between the QRS and subsequent P wave.
History and Physical
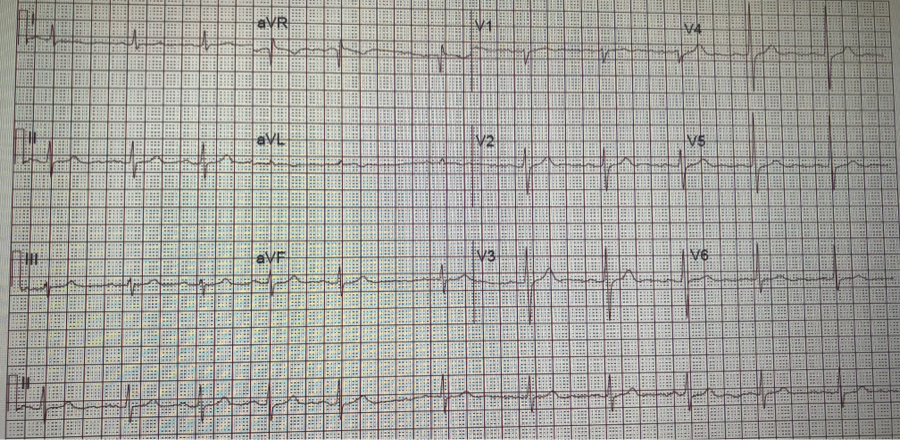
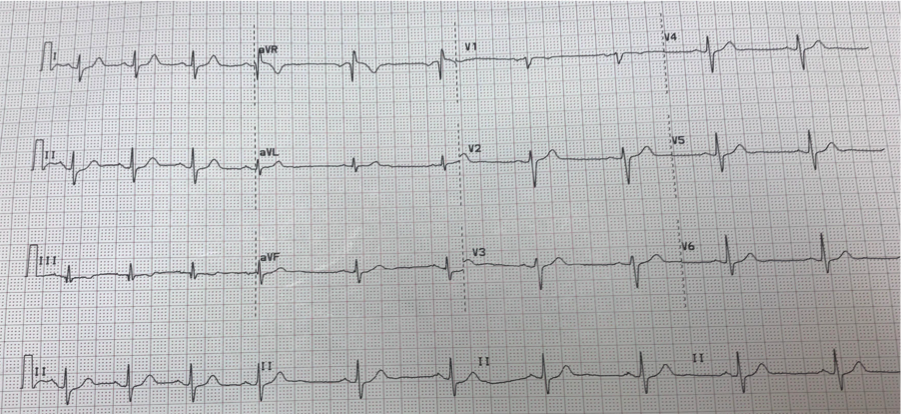
Sinus arrhythmia is a common incidental finding on presenting EKGs (see Image. 12-Lead Electrocardiogram, Sinus Arrhythmia). The finding is normal and found at a higher prevalence in younger individuals. Lack of sinus arrhythmia may indicate underlying chronic disease requiring further investigation. It is rare for symptoms to display in patients with sinus arrhythmia. If present, symptoms such as shortness of breath, lower extremity edema, dyspnea on exertion, or peripheral neuropathy are likely due to some underlying cause and not sinus arrhythmia. Care should be taken to rule out other potential causes of sinus arrhythmia while taking history. History of trauma to the head or neck via fall or another mechanism, especially in the setting of anticoagulation use, may increase suspicion of underlying intracranial hemorrhage. Additionally, care should be taken on a review of the initial EKG to rule out 3rd-degree heart block as a cause of sinus arrhythmia. No physical exam findings directly correlate to the diagnosis of sinus arrhythmia.
Evaluation
Often an asymptomatic and normal finding, the evaluation of sinus arrhythmia is limited. Care should be taken to rule out other causes of arrhythmia, including atrial fibrillation, flutter, or multifocal atrial tachycardia with an EKG. P-waves show uniform morphology. On the EKG, sinus rhythm appears as a beat-to-beat variation in the P-P interval. Typically, this variation is greater than 120 msec: the P-P interval increases and decreases with inspiration and exhalation (See Image. 12-Lead Electrocardiogram Displaying Sinus Arrhythmia).
Treatment / Management
Sinus arrhythmia is a common finding on telemetry and is considered a normal variation found in healthy young adults. Upon confirming the diagnosis of sinus arrhythmia on EKG, there are no further recommendations regarding treatment.
Differential Diagnosis
The differential diagnoses for sinus arrhythmia include the following:
- Atrial fibrillation
- Third-degree AV block
- Sick sinus syndrome
- Sinoatrial exit block
Staging
No required staging criteria exist for the evaluation of sinus arrhythmia.
Prognosis
Sinus arrhythmia indicates cardiovascular health and is often found in young, healthy patients. Sinus arrhythmia does not correlate with decreased life expectancy or other comorbidities. Its absence, however, has been associated with chronic diseases such as diabetes mellitus and heart failure.
Complications
Typically, an incidental finding, there are rarely any complications associated with sinus arrhythmia.
Consultations
Cardiology consults are not a requirement for patients with sinus arrhythmia.
Deterrence and Patient Education
Patients with sinus arrhythmia should be educated that this is a common finding in young, healthy persons. It rarely requires further evaluation upon establishment of the diagnosis.
Pearls and Other Issues
Sinus arrhythmia is a common incidental finding on routine EKG. It is most prevalent in young, healthy patients and is a prognostic indicator of good cardiac health. It decreases in prevalence in older patients and those with multiple comorbid conditions, including diabetes and heart failure. Typically asymptomatic, patients rarely require evaluation by a cardiologist or additional treatment.
Enhancing Healthcare Team Outcomes
Sinus arrhythmia is a common incidental finding that often prompts evaluation by a cardiologist. This is likely due to low provider confidence and education regarding this rhythm. Often found in young, healthy persons, sinus arrhythmia typically does not require further evaluation. There are no indications at this time for medications to treat sinus arrhythmia. Clinicians may play an essential role in evaluating sinus arrhythmia, as they are often the first health professional to detect its presence on telemetry. Comfort with the identification of this rhythm is pivotal to decreasing healthcare costs and eliminating potential exposures of patients to anticoagulants. Patients should receive counsel that this finding is normal and serves as an indicator of cardiac health.
Media
(Click Image to Enlarge)
References
Kaushal P, Taylor JA. Inter-relations among declines in arterial distensibility, baroreflex function and respiratory sinus arrhythmia. Journal of the American College of Cardiology. 2002 May 1:39(9):1524-30 [PubMed PMID: 11985918]
Coker R, Koziell A, Oliver C, Smith SE. Does the sympathetic nervous system influence sinus arrhythmia in man? Evidence from combined autonomic blockade. The Journal of physiology. 1984 Nov:356():459-64 [PubMed PMID: 6520795]
Piepoli M, Sleight P, Leuzzi S, Valle F, Spadacini G, Passino C, Johnston J, Bernardi L. Origin of respiratory sinus arrhythmia in conscious humans. An important role for arterial carotid baroreceptors. Circulation. 1997 Apr 1:95(7):1813-21 [PubMed PMID: 9107168]
Smith SA. Reduced sinus arrhythmia in diabetic autonomic neuropathy: diagnostic value of an age-related normal range. British medical journal (Clinical research ed.). 1982 Dec 4:285(6355):1599-601 [PubMed PMID: 6814668]
Barbosa Filho J, Barbosa PR, Cordovil I. Nonrespiratory sinus arrhythmia. Arquivos brasileiros de cardiologia. 2002 Apr:78(4):406-11 [PubMed PMID: 12011957]
Level 3 (low-level) evidenceDeboor SS, Pelter MM, Adams MG. Nonrespiratory sinus arrhythmia. American journal of critical care : an official publication, American Association of Critical-Care Nurses. 2005 Mar:14(2):161-2 [PubMed PMID: 15728960]
Level 3 (low-level) evidence