Introduction
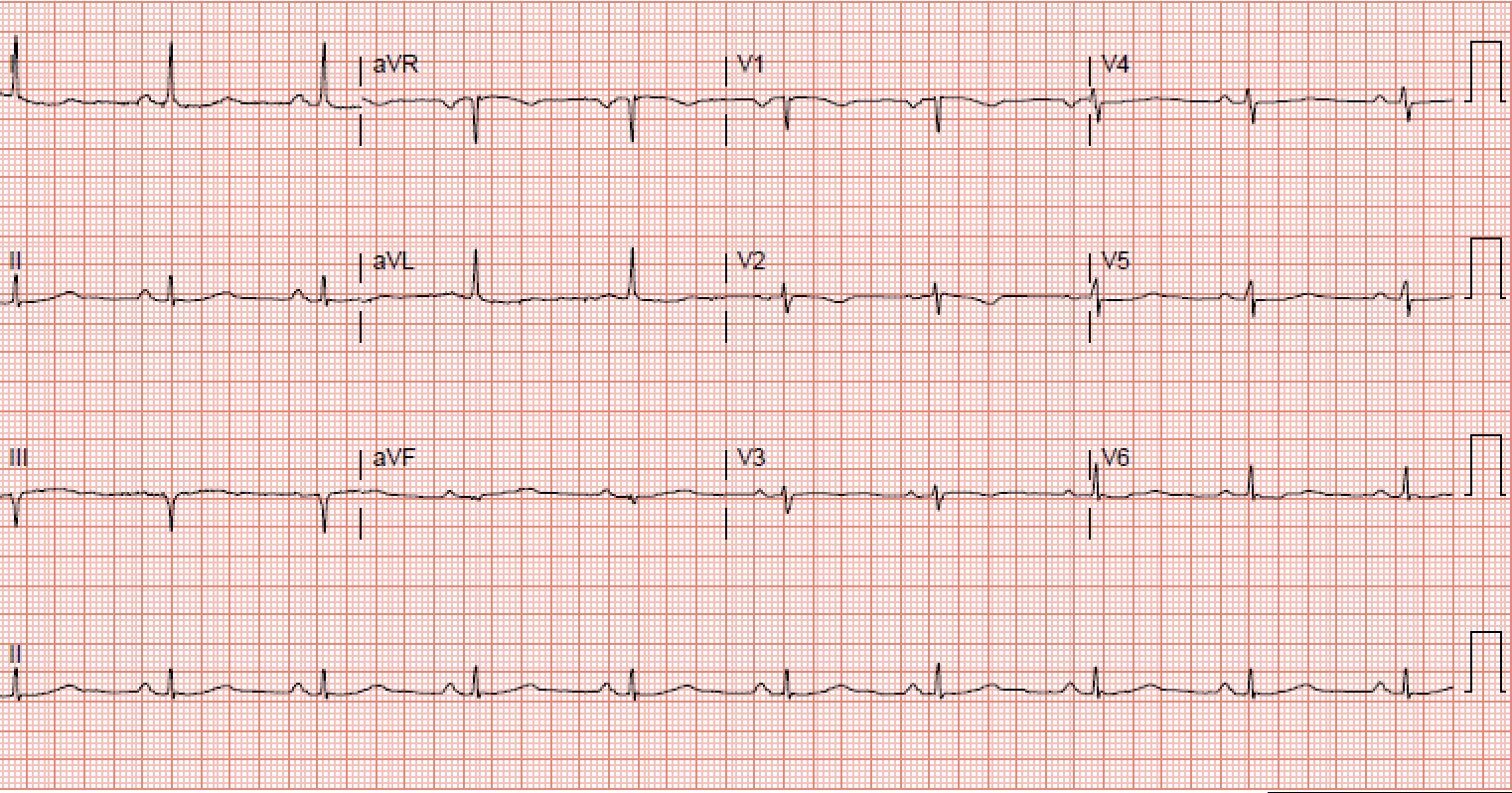
The sinoatrial node (SA) is the default pacemaker and, therefore, a crucial component of the heart's conduction system. It is located subepicardial and is crescent in shape. In an average adult, a sinoatrial node is 13.5 millimeters in length and is innervated by the vagus and sympathetic nerves. The sinoatrial nodal artery supplies blood to the sinoatrial node, it branches off the right coronary artery in 60% of cases, whereas in 40% of cases, it comes off the left circumflex coronary artery.[1][2] Sinus bradycardia is a cardiac rhythm with appropriate cardiac muscular depolarization initiating from the sinus node generating less than 60 beats per minute (bpm). The diagnosis of sinus bradycardia requires visualization of an electrocardiogram showing a normal sinus rhythm at a rate lower than 60 bpm. Where a normal sinus rhythm has the following criteria[3][4]:
- Regular rhythm, with a P wave before every QRS.
- The p wave is upright in leads 1 and 2; the P wave is biphasic in V1.
- The maximum height of a P wave is less than or equal to 2.5 mm in leads 2 and 3.
- The rate of the rhythm is between 60 bpm and 100 bpm.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Sinus bradycardia has many intrinsic and extrinsic etiologies.[5]][6][7][8][9][10]
Inherent Etiologies
- Chest trauma
- Ischemic heart disease
- Acute myocardial infarction
- Acute and chronic coronary artery disease
- Repair of congenital heart disease
- Sick sinus syndrome
- Radiation therapy
- Amyloidosis
- Pericarditis
- Lyme disease
- Rheumatic fever
- Collagen vascular disease
- Myocarditis
- Neuromuscular disorder
- X-linked muscular dystrophy
- Familial disorder
- Inherited channelopathy
Extrinsic Etiologies
- Vasovagal simulation (endotracheal suctioning)
- Carotid sinus hypersensitivity
- Beta-blockers
- Calcium channel blockers
- Digoxin
- Ivabradine
- Clonidine
- Reserpine
- Adenosine
- Cimetidine
- Antiarrhythmic class I to IV
- Lithium
- Amitriptyline
- Narcotics
- Cannabinoids
- Hypothyroidism
- Sleep apnea
- Hypoxia
- Intracranial hypertension
- Hyperkalemia
- Anorexia nervosa
Epidemiology
In clinical practice, adults over the age of 65 and young athletes of both sexes are commonly known to present with sinus bradycardia. One in 600 adults over 65 has sinus node dysfunction, but more research needs to be done to collect epidemiologic data within the United States and globally for patients with sinus bradycardia.[11]
Pathophysiology
Sinus bradycardia, as any of the other bradyarrhythmias, is caused by a multitude of intrinsic and extrinsic factors which may compromise the integrity of the sinus node. These factors can cause failure of the impulse formation at the sinus node, impulse conduction at the atrioventricular node, or bundle of His-Purkinje fibers.[9]
Sinus bradycardia is an incidental finding in many healthy adults. This is common in athletes and during sleep.
Physiological causes that increase vagal tone are more common in athletes. Pathological causes are stated in the etiology.
Sinus bradycardia is a common occurrence in sick sinus syndrome. In this disorder, there is dysfunction of the SA node. The condition is most common in elderly patients with concomitant heart disease.
Histopathology
A specific group of patients with sinus bradycardia may show no nodal histopathology, yet associated findings are as follows[9][12]:
- Nodal cell reduction and fibrosis
- Nodal region amyloidosis
- Sinus node hypoplasia or atrophy
History and Physical
The majority of patients with sinus bradycardia do not have symptoms. Healthy young adults and athletes tend to have an increased vagal tone which keeps them in sinus bradycardia at rest. Also, patients above the age of 65 tend to have sinus bradycardia during sleep secondary to the aging of the sino-atrial node. Using history to relate to the symptoms of a patient with sinus bradycardia on an electrocardiogram is essential to come to the correct diagnosis. Those who present with symptoms may present with fatigue, exercise intolerance, lightheadedness, dizziness, syncope or presyncope, worsening of anginal symptoms, worsening of heart failure, or cognitive slowing. When taking a history, a health care provider must include relevant questions that help narrow down the differential, such as any recent medication changes, medication overdoses, chest pain, shortness of breath, history of prior myocardial infarction, symptoms of intermittent palpitations, history of chest trauma, rash or recent tick bite, current or past diagnosis of streptococcus pharyngitis, family history of sinus bradycardia, family history of muscular dystrophy. Moreover, physical exam findings should be correlated with the history given by the patient to help narrow the differential diagnosis, such as any murmur heard during the physical exam or any skin exam findings of a developing rash.[13][14]
The physical exam may reveal the following:
- Cyanosis
- Peripheral edema
- An altered state of consciousness
- Dyspnea
- Rales and crackles
Evaluation
The most significant component of evaluation for a patient who presents with signs and symptoms of sinus bradycardia is history and physical exam. These should include vital signs (respiratory rate, blood pressure, temperature, and heart rate) and an electrocardiogram. During the evaluation, it should be established whether the patient is hemodynamically unstable; evaluation for this includes high blood pressure, altered mental status, or difficulty breathing. If the patient is healthy, athletic, and has no symptoms, then no further medical intervention is required. On the contrary, in older individuals, sinus bradycardia may point towards an unhealthy sinus node. Patients with congestive heart failure often have sinus bradycardia. These patients may have compromised blood supply from the right coronary artery or left circumflex artery to the sinus node secondary to some underlying ischemic heart disease.[15]
Laboratory studies that should be ordered include:
- Glucose level
- Electrolytes
- Calcium, magnesium
- Thyroid function
- Troponin
- Toxicological drug screen
A 12-lead ECG is necessary to make the diagnosis.
If there are no signs or symptoms of acute myocardial infarction in a hemodynamically stable patient, then workup should be initiated for an infectious etiology (including chest x-ray, blood cultures, urinary analysis, viral panel) together with thyroid function tests. If a patient is found to have an infectious etiology or a thyroid abnormality, the patient should be appropriately treated for these underlying etiologies and re-evaluated. Upon re-evaluation, if this patient is no longer symptomatic and his heart rate returns to within normal limits patient could be evaluated for a possible sick sinus syndrome or a long-term implantable loop recorder.
Treatment / Management
A patient with sinus bradycardia should be evaluated for hemodynamic instability. If found to be hemodynamically unstable, the patient can be treated with intravenous (IV) atropine 0.5 mg push every 3 to 5 minutes up to 3 mg total. If the patient's symptoms and heart rate do not improve, the patient is a candidate for a temporary pacemaker. If the patient on arrival is hemodynamically stable but has signs and symptoms of acute myocardial infarction, they should be treated for an acute myocardial infarction appropriately.
Hypothermic patients should be warmed to normothermia before making definitive decisions on treatment.
While management decisions are being made for a patient with sinus bradycardia, the patient's medication list should also be reviewed for possible causes of bradycardia, and those medications should be withdrawn if possible. If a patient has comorbid conditions that require him to be on certain medications, which may be causing the sinus bradycardia, then in that case-patient may be a candidate for a permanent pacemaker. In cases where medication can be withdrawn, withdrawal is made, and if symptoms and heart rate still do not improve, then the patient may be evaluated for a permanent pacemaker.[16]
Differential Diagnosis
Differentiation of sinus bradycardia from other bradyarrhythmias is done by establishing a relationship between P waves and QRS complexes on an electrocardiogram. Nondiscernible P waves are associated with junctional or ventricular escape rhythms. Whereas second or third-degree AV blocks will have more than a 1-to-1 relationship between P waves and QRS complexes[11][12].
Rhythms on the differentials are:
- Sick sinus rhythm
- Wandering atrial pacemaker
- Junctional escape rhythm
- Ventricular escape rhythm
Prognosis
Prognosis is good when the rhythm is promptly identified by a healthcare provider. However, patients with sick sinus syndrome who have bradycardia tend to have a poor prognosis with 5-year survival rates between 45 to 70%.
With the number of bariatric procedures increasing each year, it has been observed that many of these patients also develop sinus bradycardia. Whether this is linked to the sudden loss of weight is not yet known.
Complications
If not identified promptly symptomatic complications such as syncope, fatigue or dizziness can occur.
Deterrence and Patient Education
Multiple resources are available for providers to help educate patients about this rhythm and its potential symptomatic complications. A patient who comes to the hospital or a clinic and has this rhythm identified should be provided with educational pamphlets if they are available at the facility.
Pearls and Other Issues
There is a growing clinical consensus to lower the diagnosis threshold of sinus bradycardia to less than 50 bpm as there is a significant population size with a resting heart rate between 50 to 60 bpm. At present, the diagnostic consensus remains at a rate lower than 60 bpm with only the American College of Cardiology/American Heart Association/American College of Physicians–American Society of Internal Medicine (ACC/AHA/ACP–ASIM) Task Force recommending that it be diagnosed at 50 bpm.[4]
Enhancing Healthcare Team Outcomes
Because there are many causes of sinus bradycardia, an interprofessional team approach is necessary for making an early diagnosis. Nurses on the floor and in the emergency department should understand bradycardia and its treatment. The pharmacist should ensure that the cause is not potentially related to any patient medications; if there is a risk, the clinical team should be contacted. The primary care provider should refer all symptomatic patients to the cardiologist for further workup. If a pacemaker is inserted, then the patient should be closely followed by a pacemaker nurse.
Educating patients at risk for this rhythm and making a closed-loop communication between them and their providers can help further improve the management of these rhythms.
Media
(Click Image to Enlarge)
References
Thery C, Gosselin B, Lekieffre J, Warembourg H. Pathology of sinoatrial node. Correlations with electrocardiographic findings in 111 patients. American heart journal. 1977 Jun:93(6):735-40 [PubMed PMID: 871100]
Truex RC, Smythe MQ, Taylor MJ. Reconstruction of the human sinoatrial node. The Anatomical record. 1967 Dec:159(4):371-8 [PubMed PMID: 5586287]
Spodick DH. Normal sinus heart rate: sinus tachycardia and sinus bradycardia redefined. American heart journal. 1992 Oct:124(4):1119-21 [PubMed PMID: 1529897]
Kadish AH, Buxton AE, Kennedy HL, Knight BP, Mason JW, Schuger CD, Tracy CM, Boone AW, Elnicki M, Hirshfeld JW Jr, Lorell BH, Rodgers GP, Tracy CM, Weitz HH. ACC/AHA clinical competence statement on electrocardiography and ambulatory electrocardiography. A report of the ACC/AHA/ACP-ASIM Task Force on Clinical Competence (ACC/AHA Committee to Develop a Clinical Competence Statement on Electrocardiography and Ambulatory Electrocardiography). Journal of the American College of Cardiology. 2001 Dec:38(7):2091-100 [PubMed PMID: 11738321]
Silvestri NJ, Ismail H, Zimetbaum P, Raynor EM. Cardiac involvement in the muscular dystrophies. Muscle & nerve. 2018 May:57(5):707-715. doi: 10.1002/mus.26014. Epub 2017 Nov 28 [PubMed PMID: 29130502]
Gucev Z, Tasic V, Jancevska A, Jordanova NP, Koceva S, Kuturec M, Sabolic V. Friedreich's ataxia (FA) associated with diabetes mellitus type 1 and hypertrophic cardiomyopathy: analysis of a FA family. Medicinski arhiv. 2009:63(2):110-1 [PubMed PMID: 19537671]
Level 3 (low-level) evidenceMilanesi R, Baruscotti M, Gnecchi-Ruscone T, DiFrancesco D. Familial sinus bradycardia associated with a mutation in the cardiac pacemaker channel. The New England journal of medicine. 2006 Jan 12:354(2):151-7 [PubMed PMID: 16407510]
Heckle MR, Nayyar M, Sinclair SE, Weber KT. Cannabinoids and Symptomatic Bradycardia. The American journal of the medical sciences. 2018 Jan:355(1):3-5. doi: 10.1016/j.amjms.2017.03.027. Epub 2017 Mar 22 [PubMed PMID: 29289259]
Nof E, Luria D, Brass D, Marek D, Lahat H, Reznik-Wolf H, Pras E, Dascal N, Eldar M, Glikson M. Point mutation in the HCN4 cardiac ion channel pore affecting synthesis, trafficking, and functional expression is associated with familial asymptomatic sinus bradycardia. Circulation. 2007 Jul 31:116(5):463-70 [PubMed PMID: 17646576]
Level 3 (low-level) evidenceValaperta R, De Siena C, Cardani R, Lombardia F, Cenko E, Rampoldi B, Fossati B, Brigonzi E, Rigolini R, Gaia P, Meola G, Costa E, Bugiardini R. Cardiac involvement in myotonic dystrophy: The role of troponins and N-terminal pro B-type natriuretic peptide. Atherosclerosis. 2017 Dec:267():110-115. doi: 10.1016/j.atherosclerosis.2017.10.020. Epub 2017 Oct 21 [PubMed PMID: 29121498]
Brodsky M, Wu D, Denes P, Kanakis C, Rosen KM. Arrhythmias documented by 24 hour continuous electrocardiographic monitoring in 50 male medical students without apparent heart disease. The American journal of cardiology. 1977 Mar:39(3):390-5 [PubMed PMID: 65912]
Sanders P, Kistler PM, Morton JB, Spence SJ, Kalman JM. Remodeling of sinus node function in patients with congestive heart failure: reduction in sinus node reserve. Circulation. 2004 Aug 24:110(8):897-903 [PubMed PMID: 15302799]
Dobrzynski H, Boyett MR, Anderson RH. New insights into pacemaker activity: promoting understanding of sick sinus syndrome. Circulation. 2007 Apr 10:115(14):1921-32 [PubMed PMID: 17420362]
Level 3 (low-level) evidenceDobrzynski H, Anderson RH, Atkinson A, Borbas Z, D'Souza A, Fraser JF, Inada S, Logantha SJ, Monfredi O, Morris GM, Moorman AF, Nikolaidou T, Schneider H, Szuts V, Temple IP, Yanni J, Boyett MR. Structure, function and clinical relevance of the cardiac conduction system, including the atrioventricular ring and outflow tract tissues. Pharmacology & therapeutics. 2013 Aug:139(2):260-88. doi: 10.1016/j.pharmthera.2013.04.010. Epub 2013 Apr 20 [PubMed PMID: 23612425]
Level 3 (low-level) evidenceBernstein AD, Parsonnet V. Survey of cardiac pacing in the United States in 1989. The American journal of cardiology. 1992 Feb 1:69(4):331-8 [PubMed PMID: 1734644]
Level 3 (low-level) evidenceNeumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010 Nov 2:122(18 Suppl 3):S729-67. doi: 10.1161/CIRCULATIONAHA.110.970988. Epub [PubMed PMID: 20956224]