Introduction
Slipped capital femoral epiphysis (SCFE), also called slipped upper femoral epiphysis (SUFE), is the most common hip pathology in pre-adolescents and adolescents.[1] However, this diagnosis is often delayed or missed due to either atypical presentation, such as thigh or knee pain, or the chronic nature of the presentation. The differential diagnosis for pre-adolescents and adolescents presenting with leg pain is broad; thus, the medical provider must always consider the diagnosis of SCFE. A delay in the diagnosis of SCFE is associated with higher rates of complications, including femoral head osteonecrosis.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Most cases of SCFE are idiopathic. Often, there is no history of trauma or injury before the onset of symptoms. Additionally, an association has been reported between the development of SCFE and patients with endocrine disorders (including hypothyroidism, hyperthyroidism, panhypopituitarism, and growth hormone deficiency), renal disorders, and Down syndrome.[3] Hypothyroidism is the most common etiology of nonidiopathic SCF. Hence, SCFE presentation in a child younger than ten years old or weighing less than the 50th percentile is an indication of endocrine workup.
Epidemiology
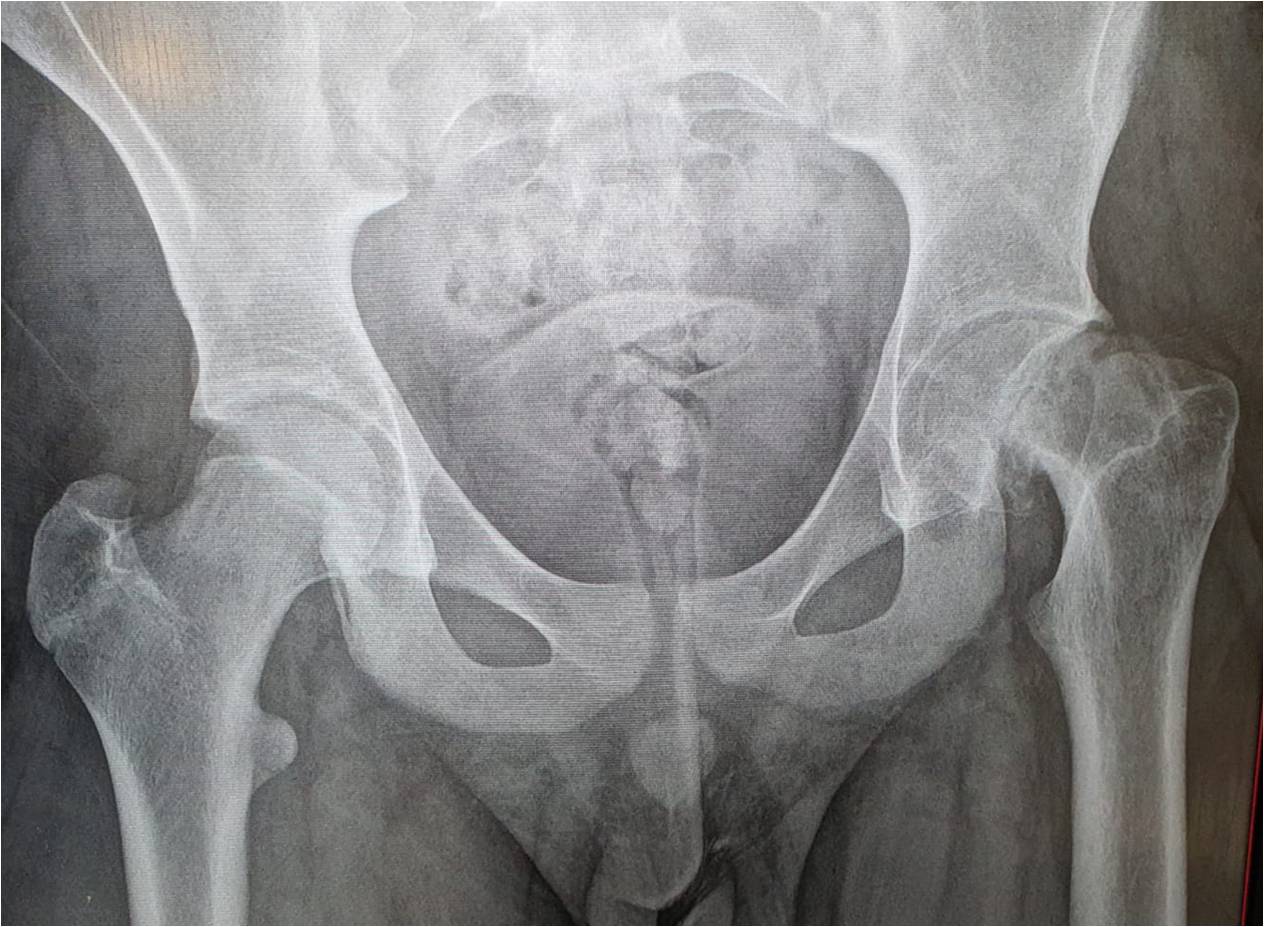
SCFE is one of the most common hip pathologies affecting pre-adolescent and adolescent patients, occurring in approximately 10.8/100,000 (Range: 0.33/100,000 to 24.8/100,000). The single most significant risk factor for SCFE is obesity.[4] Other risk factors include male sex, periods of rapid growth, prior radiation therapy to the hip, and retroversion of the acetabulum or femoral head, both of which increase mechanical shear forces across the physis. The average age of onset is 11.2 years in females and 12.0 years in males. The left hip is more commonly affected, but approximately 25% (Range: 8 to 50%) of cases are bilateral.[2] Recent literature has shown increased incidence at a younger age and more bilateral cases being reported as a possible reflection of increased rates of childhood obesity.
Pathophysiology
The exact mechanism remains uncertain. It is hypothesized that displacement occurs due to a high physiologic axial load transmitted across a relatively weak physis. Conditions such as obesity increase the mechanical weight and force transmitted, whereas certain endocrine or renal disorders may contribute to the weakening of the physis.[5]
The epiphysis stays in the acetabulum, and the metaphysis externally rotates with anterior translation. This slippage occurs at the level of the hypertrophic zone of the physis. In adolescence, a combination of factors puts the physis at high risk of slippage. That includes the physis being in a vertical position more susceptible to shear forces, thinning and weakening of the perichondrial ring of la Croix, along with unlocking of the mamillary processes of the physis, further destabilizing it. SCFE is a Salter-Harris type I fracture that can be differentiated with preceding epiphysiolysis, more steady displacement, and intact periosteum in chronic cases or partially torn in acute cases.
History and Physical
The clinician should always consider SCFE in a pre-adolescent, adolescent, or young adult patient with a complaint of atraumatic hip, thigh, or knee pain, particularly if associated with limping or inability to bear weight. Pain is most often reported in the hip (52%); however, pain associated with SCFE may also be reported in the groin (13.9%), thigh (35%), or knee (26%).[6] Knee pain is usually due to pain activation of the medial obturator nerve. Patients with SCFE, on average, have 4 to 5 months of symptoms prior to diagnosis; however, patients with SCFE may also present with less than three weeks of symptoms. While most patients will not report any history of trauma or injury before the onset of symptoms, a history of injury or trauma does not exclude the possibility of SCFE.[2][7] The patient may prefer to sit with the affected leg crossed over the other.
On examination, a limited internal rotation of the affected extremity can be present, and passive internal rotation may elicit pain. There would be a loss of hip flexion, abduction, and internal rotation. The patient may demonstrate the Drehmann sign, which is obligatory external rotation with passive hip flexion to 90 degrees.[8] Additionally, the patient may have a shuffling, Trendelenburg, antalgic gait, or a complete inability to bear weight. Thigh atrophy may or may not be present.[7]
Evaluation
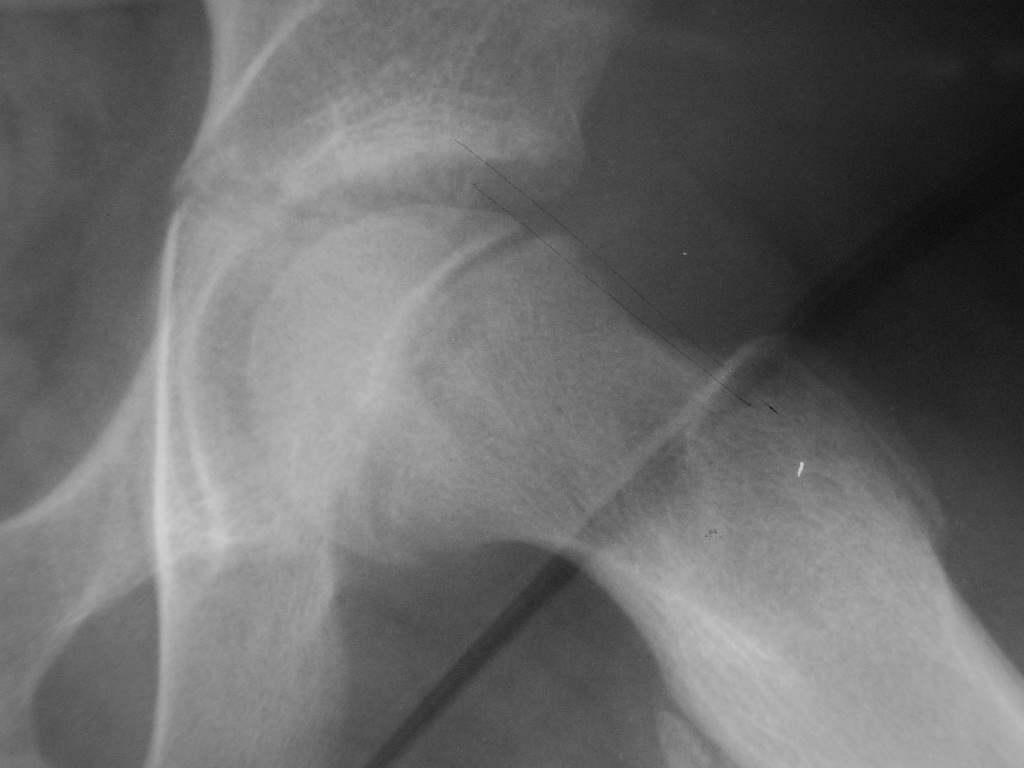
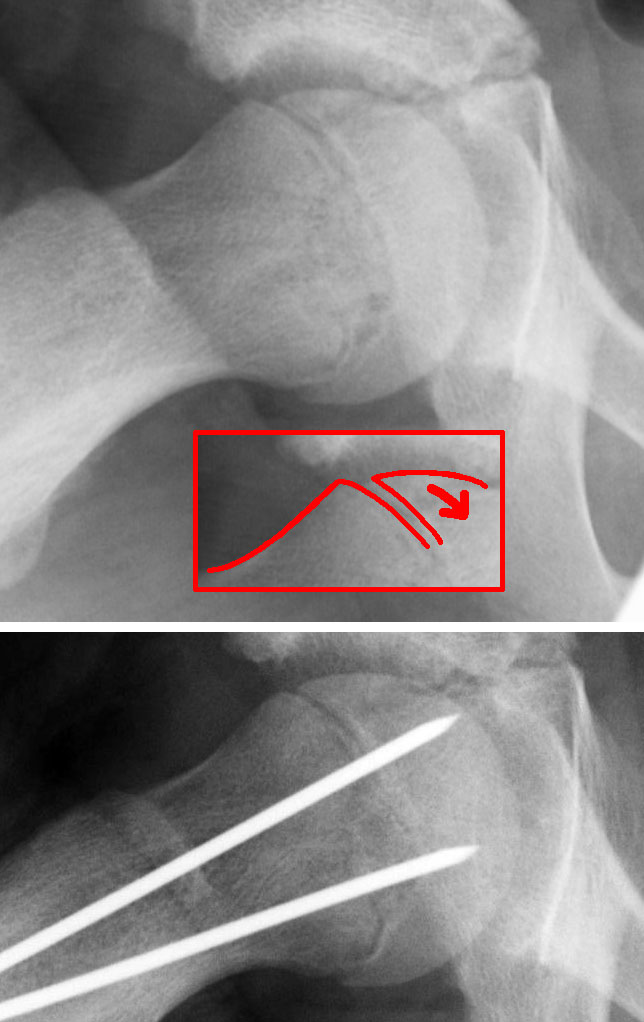
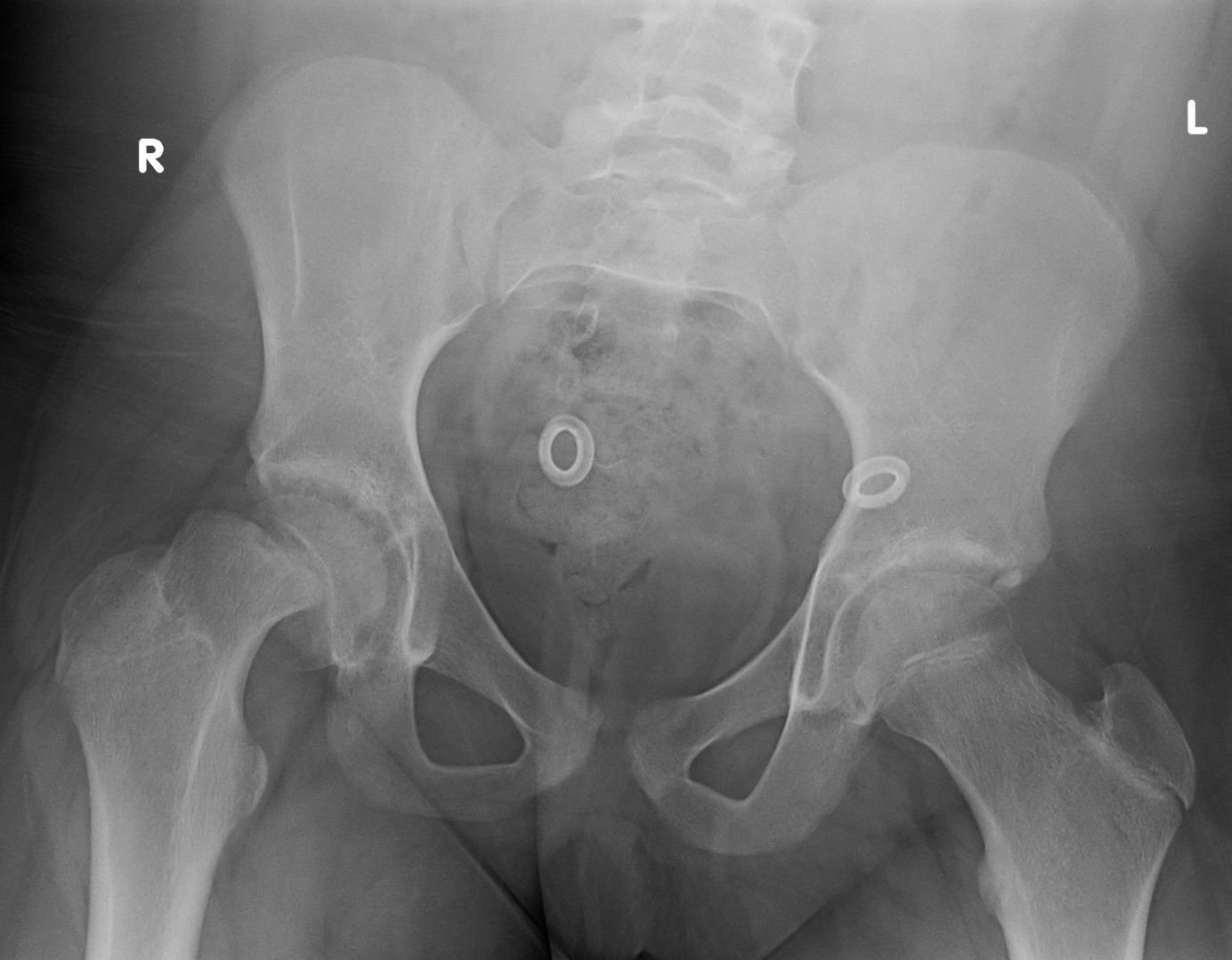
The evaluation of patients with suspected SCFE should begin with bilateral hip radiographs with anteroposterior (AP) and frog-leg lateral views.[9] Radiographs should be bilateral to allow for comparison. Klien's line is a radiographic finding used to detect SCFE on plain radiographs. On the AP view, a line is drawn along the superior border of the femoral neck. In a normal hip, the line intersects the lateral part of the superior femoral epiphysis. If Klein's line fails to intersect the epiphysis, SCFE is likely present (known as the Trethowan sign); however, this method has relatively low sensitivity for diagnosing SCFE.[7]
Other plain radiography methods of detecting SCFE include the Southwick slip angle and the "S" sign. The Southwick slip angle measures the degrees of epiphyseal displacement in relation to the diaphysis; this method is considered more sensitive in detecting SCFE. The "S" sign consists of a line drawn along the inferior cortical outline of the femur in the frog-leg lateral view that extends from the proximal femoral head-neck junction to the proximal femoral physis; normally, the cortical outlines are symmetrical, without sharp turns, or broken continuity. SCFE is likely to present if the cortical outlines are asymmetrical, have a sharp turn, or have broken continuity. The use of the "S" sign in conjunction with Klein's line was found to increase both sensitivity and specificity in the detection of SCFE.[10]
Ephyisiolysis, which is the widening or lucency of the growth plate, could be an early radiographic sign. In addition, another sign can be detected on the anteroposterior radiographs, the metaphyseal blanch sign of steel, which is the blurring of the proximal femoral metaphysis due to its overlapping on the displaced epiphysis.
If radiographs do not demonstrate findings consistent with SCFE, but clinical suspicion is high, the clinician can consider obtaining magnetic resonance imaging (MRI) to evaluate further.[7] MRI can be helpful in the diagnosis of pre-slip cases, which demonstrates metaphyseal edema and growth plate widening. Several recent small studies suggest that ultrasound may be a more sensitive modality compared to radiographs in diagnosing SCFE; however, further investigation of ultrasound application is needed.[11]
The clinician should consider laboratory testing to evaluate for possible underlying medical conditions such as endocrine or renal disorders if the patient is less than ten years of age or pre-pubertal, has short stature (more than two standard deviations below mean for age), or weight below the 50th percentile for age. Initial laboratory testing can include thyroid-stimulating hormone (TSH) level, thyroxine level (free T4), blood urea nitrogen (BUN), and serum creatinine.[3] Further testing can be performed in consultation with appropriate pediatric specialists, such as pediatric endocrinology.
Treatment / Management
Management is mainly operative for both stable and unstable SCFE.[12][13] This includes:
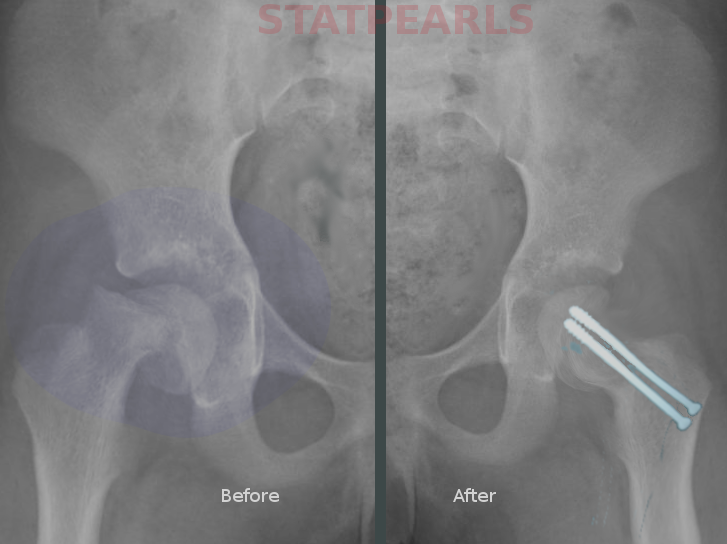
In situ fixation with Percutaneous Screws
The aim is to prevent further slippage of the epiphysis. The epiphysis is fixed in situ. If a reduction is indicated, a serendipitous reduction is performed rather than forceful to reduce the risk of osteonecrosis.[8][14]
Controversy exists about whether to use one or two screws. A single screw is sufficient; however, the advantage of two screws is being more biomechanically stable but at the expense of a higher complication rate, including articular surface violation.
The screw should be perpendicular to the physis and central in the head, both in the anteroposterior and lateral views. To achieve that, the entry point should be anterior in the proximal femur; however, care should be taken not to be medial to the intertrochanteric line to avoid impingement in flexion between the acetabulum and the screw head. Screws should be advanced until 5 mm from the subchondral bone in all views, with at least five threads engaging the epiphysis to prevent slip progression.
The procedure is performed under fluoroscopy guidance. The screw tip should not violate the articular surface in any view. The approach-withdraw technique has been performed to confirm the correct position of the screw. This is accomplished by maximally internally and externally rotating the hip under live fluoroscopy. The screw tip is viewed as approaching and then withdrawing from the subchondral bone. The point of the change is the appropriate position of the screw.
Postoperatively, patients are allowed to bear weight after fixation in case of stable slips and partially weight-bearing for six weeks in unstable slips.
Capsulotomy has been shown to reduce intracapsular pressure in unstable SCFE. However, there is no clear evidence that it reduces the avascular necrosis rate.
Prophylactic fixation of the contralateral hip is another controversial modality. It is indicated when there are high-risk factors for a contralateral slip. Such as obesity, male gender, initial slip in a younger than ten years old, endocrine disorders
Open Reduction and Internal Fixation of the Slipped Epiphysis (Modified Dunn Procedure)
The aim is to correct the deformity of the proximal femur and stabilize the epiphysis, meanwhile protecting the femoral head blood supply.[15]
The procedure involves the surgical dislocation of the hip through the Gibson approach. The patient is positioned in lateral decubitus. The incision is straight lateral over the greater trochanter. The approach utilizes the plane between the gluteus maximus and medius. A trochanteric flip osteotomy is performed—Z-shaped anterior capsulotomy to expose the metaphysis. The slipped epiphysis is initially primarily stabilized by k wire prior to dislocation; then, the hip is dislocated using a hook around the femoral neck for traction. Once the hip is dislocated, an incision of the periosteum is performed over the anterior neck and proximal femur to the lesser trochanter. Periosteal flaps are developed bluntly anteriorly and posteriorly. The epiphysis is freed completely from the metaphysis using a chisel; then, the metaphysis is debrided. The epiphysis is reduced and fixed to the metaphysis using two or three K wires, both antegrade and retrograde. Postoperatively, patients are instructed to only partially weight bear for six weeks.
This is another controversial management modality indicated in unstable and severe slips. It is performed through a modified Dunn procedure, which is capital realignment.
After initial management, patients may develop consequences that can be symptomatic, and these can also be addressed by operative management such as femoroacetabular impingement as a result of a cam lesion from a metaphyseal bump or cases of SCFE deformity with a slip angle < 30 degrees. Both can be managed by osteochondroplasty.
However, severe SCFE deformity with a slip of more than 30 to 45 degrees, which is painful or limiting function in the absence of hip osteoarthritis or osteonecrosis, can be managed by proximal femoral osteotomy. Several proximal femoral osteotomies have been described in the literature, with the most commonly used one being intertrochanteric (Imhauser) osteotomy. The greatest deformity correction is achievable by femoral neck cuneiform osteotomy. Also, subtrochanteric (Southwick) osteotomy has been described.
Osteochondroplasty is indicated in mild and moderate chronic SCFE deformity cases where a prominent metaphyseal bump results in pain and a restricted range of motion. Osteochondroplasty can be performed arthroscopically with a burr or through a limited anterior arthrotomy via a modified Smith-Peterson approach.[16] Also, it can be performed through surgical dislocation of the hip and using a curved osteotome to remove the bump along with a burr to reshape the contour of the head-neck junction.[17]
Differential Diagnosis
The differential diagnosis of SCFE should include infectious etiologies such as septic arthritis and osteomyelitis, particularly if the patient is febrile or ill-appearing. If the onset of pain is reported in the context of a sports injury or other traumatic injury, etiologies such as avulsion fracture of the anterior iliac spine(s), adductor muscle strain, ligamentous knee injury, and femur or pelvic fractures should be considered. Inflammatory processes such as transient synovitis, Legg-Calve-Perthes disease, and Osgood-Schlatter disease can also be considered in the appropriate clinical context. However, if the patient has a clinical exam consistent with possible SCFE, even if other clinical features are atypical, the clinician should strongly consider obtaining plain radiographs of the hips.
Staging
There are three classification systems for SCFE: Loder Classification, Southwick Slip Angle Classification, and Temporal Classification.
The Loder Classification was introduced in 1993 based on the ability to bear weight and helps to predict osteonecrosis. Cases can be classified as stable if the patient is able to bear weight with or without crutches. And those cases would have less than a 10% risk of osteonecrosis. Or unstable if the patient is unable to bear weight. And these cases carry a higher risk of osteonecrosis (24 to 47%).
The Southwick Slip Angle Classification grades the severity of SCFE based on the difference in the epiphyseal diaphyseal angle between the affected hip and the unaffected/contralateral hip, both in anteroposterior and lateral radiographs of the hip. Mild cases < 30 degrees, moderate cases 30-50 degrees, and severe cases with more than 50 degrees of difference. In bilateral cases, a set reference is used for comparison: 145 degrees on the anteroposterior radiographs and 10 degrees on the lateral radiographs.
Temporal Classification is based on the duration of symptoms. It is seldom used as it has no bearing on prognosis. SCFE is considered acute if symptoms are present for less than three weeks, chronic if symptoms have persisted for more than three weeks, or acute on chronic if a patient has worsening symptoms for more than three weeks.
SCFE can also be graded based on the percentage of slippage. Grade I up to 33%, Grade II 34 to 50 %, and Grade III over 50%.
Prognosis
The Loder classification is essential in prognosis. The original study in 1993 found that a patient with SCFE classified as stable did not develop osteonecrosis, whereas 47% of the patients with SCFE who were considered unstable went on to develop osteonecrosis. More recent studies, including a systematic review, have confirmed these findings.[18][19]
Complications
Complications of SCFE include femoral growth arrest due to premature closure of the physis, femoral head osteonecrosis, chondrolysis, femoroacetabular impingement, labral tears, infection, chronic pain, and development of SCFE in the contralateral hip. Later complications of SCFE include early-onset osteoarthritis of the hip.[18][20]
Femoral head osteonecrosis could result from the initial injury, with a higher risk in unstable SCFE cases.[21][22] Also, it can develop as a postoperative complication due to metalwork placement in the posterosuperior aspect of the femoral neck, where it poses a risk of disrupting the blood supply of the femoral neck.
Chondrolysis could be a consequence of articular surface penetration.[21] Patients will usually present with pain and a reduced range of motion. Radiographs will show reduced joint space, and a CT scan would be the best modality to assess metalwork penetration.
Femoroacetabular impingement is due to failure of proximal femoral remodeling (pistol grip deformity). This can be addressed, as mentioned earlier, by proximal femoral osteotomy.[23]
Slip progression: This has been reported in 1 to 2% of cases with single screw fixation.
Postoperative and Rehabilitation Care
Postoperative rehabilitation protocols for SCFE are poorly described in the literature. However, it follows the same pattern for postoperative rehabilitation following hip preserving procedures, e.g., hip arthroscopies.[24] Most recommended protocols in the literature involve a five-phase regime with predictable recovery times.[8]
Phase 1
It involves using appropriate walking aids and performing gait analysis to assess the patient’s heel-to-toe pattern. The main focus of the phase is the reduction of joint inflammation, protection of soft tissue repair, synergistic muscle activation, and range of motion.
Phase 2
Weaning off crutches once the patient has a normal pain-free gait pattern and can perform pain-free straight leg raises and abduction.
Phases 3 and 4
Increasing range of motion and aerobic conditioning. In addition to strengthening functional movement patterns.
Phase 5
Ensuring adequate functional power is crucial for returning to daily activities or playing. The time frame for a return to play is variable and set by the treating surgeon based on the case.
Deterrence and Patient Education
Patients and their families require instructions on strict non-weight-bearing status. They will also require counseling on adequate pain control. If, after pediatric orthopedic consultation, urgent operative management is not performed, patients and families should be given anticipatory guidance regarding SCFE and the need for urgent orthopedic follow-up. If there is any concern that the family may be unable or unwilling to follow up with an orthopedic surgeon, admission with pediatric orthopedic consultation should be strongly considered.
Enhancing Healthcare Team Outcomes
Slipped capital femoral epiphysis (SCFE), also called slipped upper femoral epiphysis (SUFE), is the most common hip pathology in pre-adolescent and adolescent patients; however, the diagnosis can be delayed or missed. Primary care (family medicine, internal medicine, or pediatrics) and emergency medicine clinicians, including clinicians and advanced practice providers, should always consider SCFE in the differential diagnosis of pre-adolescent and adolescent patients with leg pain.
Patients with a suspected or confirmed diagnosis of SCFE must be immediately placed on strict non-weight bearing precautions and provided adequate analgesia; thus, effective interprofessional communication among clinicians (including specialists from orthopedics and radiology), nursing, pharmacists, physical therapists, and patient care technicians is paramount to ensure optimal care delivery. Urgent pediatric orthopedic consultation for definitive management should be prioritized. Clinicians should additionally consider clinical features of possible underlying endocrine or renal disorders and further evaluate patients as indicated in consultation with appropriate subspecialists. Interprofessional teamwork and open communication are crucial to optimal patient results. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mathew SE, Larson AN. Natural History of Slipped Capital Femoral Epiphysis. Journal of pediatric orthopedics. 2019 Jul:39(Issue 6, Supplement 1 Suppl 1):S23-S27. doi: 10.1097/BPO.0000000000001369. Epub [PubMed PMID: 31169643]
Loder RT, Skopelja EN. The epidemiology and demographics of slipped capital femoral epiphysis. ISRN orthopedics. 2011:2011():486512. doi: 10.5402/2011/486512. Epub 2011 Sep 21 [PubMed PMID: 24977061]
Wells D, King JD, Roe TF, Kaufman FR. Review of slipped capital femoral epiphysis associated with endocrine disease. Journal of pediatric orthopedics. 1993 Sep-Oct:13(5):610-4 [PubMed PMID: 8376562]
Perry DC, Metcalfe D, Lane S, Turner S. Childhood Obesity and Slipped Capital Femoral Epiphysis. Pediatrics. 2018 Nov:142(5):. pii: e20181067. doi: 10.1542/peds.2018-1067. Epub 2018 Oct 22 [PubMed PMID: 30348751]
Witbreuk M, van Kemenade FJ, van der Sluijs JA, Jansma EP, Rotteveel J, van Royen BJ. Slipped capital femoral epiphysis and its association with endocrine, metabolic and chronic diseases: a systematic review of the literature. Journal of children's orthopaedics. 2013 Jun:7(3):213-23. doi: 10.1007/s11832-013-0493-8. Epub 2013 Mar 30 [PubMed PMID: 24432080]
Level 1 (high-level) evidenceUvodich M, Schwend R, Stevanovic O, Wurster W, Leamon J, Hermanson A. Patterns of Pain in Adolescents with Slipped Capital Femoral Epiphysis. The Journal of pediatrics. 2019 Mar:206():184-189.e1. doi: 10.1016/j.jpeds.2018.10.050. Epub 2018 Nov 16 [PubMed PMID: 30454962]
Georgiadis AG, Zaltz I. Slipped capital femoral epiphysis: how to evaluate with a review and update of treatment. Pediatric clinics of North America. 2014 Dec:61(6):1119-35. doi: 10.1016/j.pcl.2014.08.001. Epub 2014 Sep 26 [PubMed PMID: 25439015]
Peck DM, Voss LM, Voss TT. Slipped Capital Femoral Epiphysis: Diagnosis and Management. American family physician. 2017 Jun 15:95(12):779-784 [PubMed PMID: 28671425]
Hesper T, Zilkens C, Bittersohl B, Krauspe R. Imaging modalities in patients with slipped capital femoral epiphysis. Journal of children's orthopaedics. 2017 Apr:11(2):99-106. doi: 10.1302/1863-2548-11-160276. Epub [PubMed PMID: 28529656]
Rebich EJ, Lee SS, Schlechter JA. The S Sign: A New Radiographic Tool to Aid in the Diagnosis of Slipped Capital Femoral Epiphysis. The Journal of emergency medicine. 2018 Jun:54(6):835-843. doi: 10.1016/j.jemermed.2018.01.023. Epub 2018 Mar 15 [PubMed PMID: 29550284]
Mc Cabe A, McArdle S. Towards evidence-based emergency medicine: Best BETs from the Manchester Royal Infirmary. BET 2: Is ultrasound or plain film radiography a more sensitive diagnostic modality for diagnosing slipped capital femoral epiphysis? Emergency medicine journal : EMJ. 2014 Jan:31(1):80. doi: 10.1136/emermed-2013-203411.2. Epub [PubMed PMID: 24367014]
Otani T, Kawaguchi Y, Marumo K. Diagnosis and treatment of slipped capital femoral epiphysis: Recent trends to note. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2018 Mar:23(2):220-228. doi: 10.1016/j.jos.2017.12.009. Epub 2018 Feb 1 [PubMed PMID: 29361376]
Aprato A, Conti A, Bertolo F, Massè A. Slipped capital femoral epiphysis: current management strategies. Orthopedic research and reviews. 2019:11():47-54. doi: 10.2147/ORR.S166735. Epub 2019 Mar 29 [PubMed PMID: 31040725]
Thawrani DP, Feldman DS, Sala DA. Current Practice in the Management of Slipped Capital Femoral Epiphysis. Journal of pediatric orthopedics. 2016 Apr-May:36(3):e27-37. doi: 10.1097/BPO.0000000000000496. Epub [PubMed PMID: 25929770]
Davis RL 2nd, Samora WP 3rd, Persinger F, Klingele KE. Treatment of Unstable Versus Stable Slipped Capital Femoral Epiphysis Using the Modified Dunn Procedure. Journal of pediatric orthopedics. 2019 Sep:39(8):411-415. doi: 10.1097/BPO.0000000000000975. Epub [PubMed PMID: 31393301]
Accadbled F, May O, Thévenin-Lemoine C, de Gauzy JS. Slipped capital femoral epiphysis management and the arthroscope. Journal of children's orthopaedics. 2017 Apr:11(2):128-130. doi: 10.1302/1863-2548-11-160281. Epub [PubMed PMID: 28529661]
Kuzyk PR, Kim YJ, Millis MB. Surgical management of healed slipped capital femoral epiphysis. The Journal of the American Academy of Orthopaedic Surgeons. 2011 Nov:19(11):667-77 [PubMed PMID: 22052643]
Roaten J, Spence DD. Complications Related to the Treatment of Slipped Capital Femoral Epiphysis. The Orthopedic clinics of North America. 2016 Apr:47(2):405-13. doi: 10.1016/j.ocl.2015.09.013. Epub [PubMed PMID: 26772949]
Ganz R. Alshryda S et al. Evidence based treatment for unstable slipped upper femoral epiphysis: Systematic review and exploratory patient level analysis. The Surgeon. 2018; 16: 46-54. The surgeon : journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2019 Feb:17(1):61. doi: 10.1016/j.surge.2018.10.003. Epub 2018 Dec 2 [PubMed PMID: 30514665]
Level 1 (high-level) evidenceFernandez FF, Eberhardt O, Wirth T. [Early and late complications and their management in slipped capital femoral epiphysis]. Der Orthopade. 2019 Aug:48(8):677-684. doi: 10.1007/s00132-019-03729-2. Epub [PubMed PMID: 31025044]
Lubicky JP. Chondrolysis and avascular necrosis: complications of slipped capital femoral epiphysis. Journal of pediatric orthopedics. Part B. 1996 Summer:5(3):162-7 [PubMed PMID: 8866280]
Level 3 (low-level) evidenceMullins MM, Sood M, Hashemi-Nejad A, Catterall A. The management of avascular necrosis after slipped capital femoral epiphysis. The Journal of bone and joint surgery. British volume. 2005 Dec:87(12):1669-74 [PubMed PMID: 16326884]
Soni JF, Valenza WR, Uliana CS. Surgical treatment of femoroacetabular impingement after slipped capital femoral epiphysis. Current opinion in pediatrics. 2018 Feb:30(1):93-99. doi: 10.1097/MOP.0000000000000565. Epub [PubMed PMID: 29206650]
Level 3 (low-level) evidenceSpencer-Gardner L, Eischen JJ, Levy BA, Sierra RJ, Engasser WM, Krych AJ. A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2014 Apr:22(4):848-59 [PubMed PMID: 24077689]