Introduction
Community-acquired pneumonia (CAP) is the seventh leading cause of death in the United States, and the cost of these hospitalizations is estimated to cost up to $9 billion in the United States (US) dollars each year. Thirty-day hospital mortality associated with CAP has been estimated to be as high as 22% and is the leading cause of death amongst all infectious diseases.
Streptococcus pneumoniae is the bacterium that has historically been the most common pathogen to cause CAP worldwide. In the era before antibiotics, S. pneumoniae was estimated to be the cause of 95% of all cases of pneumonia. Currently, however, S. pneumoniae accounts for up to 15% of pneumonia cases in the United States and 27% of cases worldwide today. Blood cultures are positive in only 20% to 25% of all pneumonia cases that are caused by S. pneumonia making it a challenging diagnosis for the clinician.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
S. pneumonia was first isolated from the saliva of a patient with rabies in 1881 by Louis Pasteur and the association between lobar pneumonia, and Friedlander and Talamon first reported the bacteria in 1883. Although vaccination efforts were underway as early as 1911, the first pneumococcal vaccine was not produced in the United States until 1977 and the first conjugate vaccine in 2000.[4][5]
S. pneumonia is a lancet-shaped, gram-positive, facultative anaerobic organism that typically occurs in pairs or short chains. Encapsulated S. pneumonia is pathogenic for humans, and the capsular polysaccharide is the basis for which the organism is classified. As of 2011, a total of 92 separate serotypes have been isolated.
Epidemiology
Pneumococcal infections are present throughout the world and are most common during the winter and early spring months. IS. pneumoniae is prevalent in large part due to its colonizing ability in the nasopharynx. Almost 40%-50% healthy children and 20%-30% of healthy adults are carriers.[6] With childhood conjugate vaccination for Streptococcus pneumoniae, the colonization frequency has decreased.
Although S. pneumoniae pneumonia can occur in all populations, it is more common in patients older than 65 years, younger than 2 years, those who smoke, abuse alcohol, have asthma or COPD, or are asplenic. The overall rate of confirmed S. pneumoniae infection in the United States is 5.16 to 6.11 cases/100,000 in adults with the rate for those older than 65 years being 36.4/100,000 and infants younger than 1 year being 34.2/100,000.[7][8][9] World Health Organization estimated that 1.6 million deaths in 2005 including 1 million children less than 5 years of age, occurred due to streptococcus pneumoniae. It is a common co-infection in influenza patients and affects the morbidity and mortality in such patients.
Pathophysiology
Infection typically occurs after the colonization of the oropharynx and nasopharynx of healthy individuals. Inhalation of these colonies causes the infection of the lower airways. Infection, typically will not result unless a patient has predisposed risk factors, a bolus of infectious cells or due to a particularly virulent strain of S. pneumoniae.
The capsule plays a major role in the pathogenesis of Streptococcus pneumoniae. It is made up of polysaccharides and surrounds the cell wall. It helps in escaping phagocytosis by preventing the access of granulocytes to the underlying cell wall. These polysaccharides of the capsule help in the identification and serotyping of the bacteria. Many serotypes have been detected, 6, 14, 18, 19 and 23 are the most common ones causing the infection. On culture media, the virulence of these strains can be identified by their appearance, opaque and transparent types. Transparent type usually colonizes in nasopharynx while the opaque type is present in the lung, brain and bloodstream infection.
The second important characteristic of the pathogenicity of Streptococcus pneumoniae is its ability to adhere to the respiratory epithelium and invasion.
The severity of the pneumococcal disease is due to significant inflammatory response induced by the activation of complement pathways and cytokine release by cell wall proteins, autolysin, the capsular polysaccharides and DNA released by bacterial end products.
Toxicokinetics
S. pneumonia has several virulence factors that allow it to cause infections in humans. A polysaccharide capsule interferes with phagocytosis by inhibiting the binding of complement C3b to the cell’s surface. Pneumococcal proteins also play a large role in the virulence of the bacteria. IgA1 protease interferes with host defense at mucosal surfaces, and neuraminidase prevents the attachment to epithelial cells. Other proteins that act in the virulence of S. pneumonia include pneumolysin, pneumococcal surface protein A, and autolysin. Lastly, pili allow for the adherence of the organism to cellular surfaces and play a role in host inflammation.
Over the last several years, drug-resistant S. pneumonia (DRSP) and penicillin-resistant S. pneumonia have become more common. Penicillin resistance is the result of alterations in the penicillin-binding protein (PBP) and affects the binding penicillin but not that of all the beta-lactams. DRSP is the result of genetic mutations that can either cause an active efflux of the drug out of the cell or block it from binding. Those at risk of DRSP include the extremes of age, recent antimicrobial therapy, either attending daycare or having a family member who attends daycare, having multiple co-morbid conditions, or being recently hospitalized.
History and Physical
Those with pneumonia may present with a wide array of symptoms, but the most common include dyspnea, cough, pleuritic pain, sputum production, and fever. However, in many studies, these symptoms have been found to neither are sensitive or specific for the diagnosis of pneumonia. In the elderly, the clinical presentation may not follow typical patterns, leading to delay in diagnosis and increased mortality. In the elderly symptoms such as generalized weakness, altered mental status and malaise could be the first signs of the illness.
A patient’s vital signs may be the most useful physical exam finding in diagnosing those with pneumonia. When tachypnea, hypoxia, or hyperthermia is present in a patient whose pneumonia is suspected, further diagnostic evaluation should be undertaken. Classical signs of consolidation such as egophony, rales, whispered pectoriloquy, dullness to percussion or bronchial breath sounds might be heard. However, multiple studies have shown that physical exam findings lack both sensitivity and inter-observer reliability in regards to diagnosing pneumonia.
Evaluation
Routine laboratory evaluation does not aid in diagnosing the organism causing pneumonia but may allow for better risk stratification of patients.[10][11]
Chest radiography has been considered to be the mainstay in diagnosing pneumonia. Classically lobar pneumonia has been taught to be caused by S. pneumonia. However new literature has shown that a radiograph is not reliable in determining the causative organism in pneumonia patients. Unfortunately, radiographs are not 100% sensitive in diagnosing pneumonia. Computed tomography (CT) has shown to have better sensitivity and accuracy as compared to plain chest radiography to diagnose CAP but is used limitedly because of a relatively high cost and radiation exposure.
The diagnosis of the causative organism for pneumonia can be obtained through a variety of means including blood cultures, sputum analysis, and urinary antigens. The routine collection of blood cultures has been controversial in the literature. Recently the Centers for Medicaid and Medicare Services and the Joint Commission on Accreditation of Healthcare Organizations have noted that routine collection of blood cultures is no longer a core measure that is being tracked. Also, the American College of Emergency Physicians (ACEP) made a grade B recommendation against the routine collection of blood cultures in patients admitted with CAP. Further sources note that blood cultures should be obtained in those admitted to the intensive care unit, those with leukopenia, cavitary lesion, severe liver disease, alcohol abuse, asplenia or pleural effusions. When blood cultures are positive, the majority show S. pneumonia but rarely change clinical management.
Sputum cultures typically have had low sensitivity and specificity in detecting the causative organism for pneumonia. However, in those patients suspected of having a drug-resistant organism, sputum cultures should be obtained.
A urinary antigen does exist to aid the clinician in diagnosing cases of S. pneumonia and carries a sensitivity of 80% and a specificity of 97%. However, the usefulness in children is debatable due to many children being carriers of S. pneumonia.
Treatment / Management
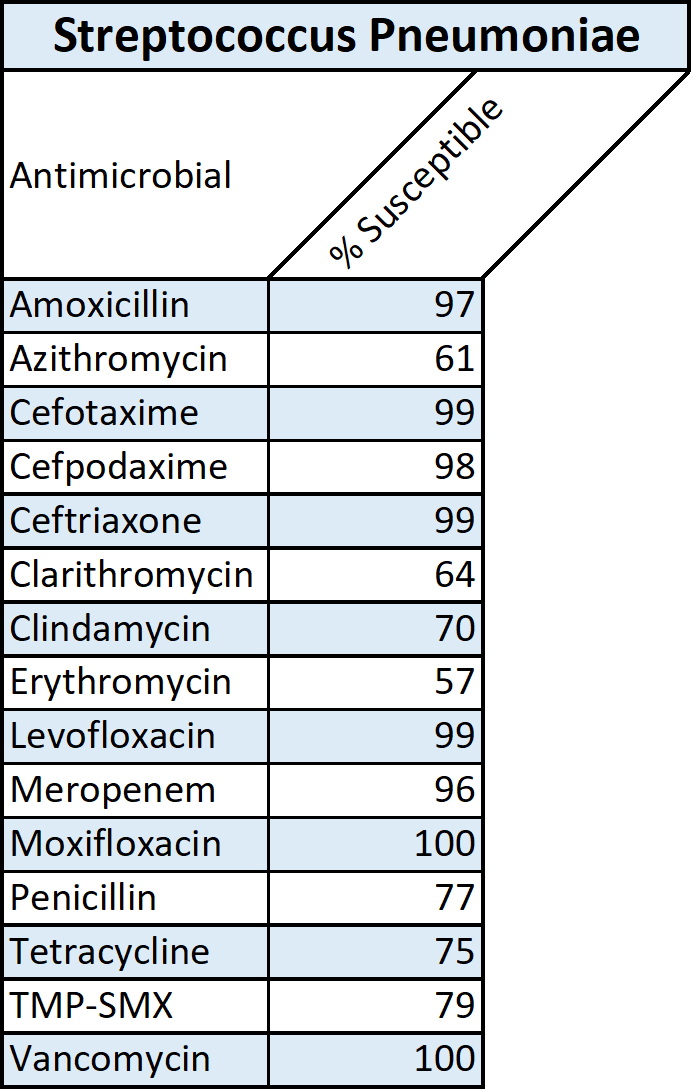
The mainstay of treatment for patients with S. pneumonia is antibiotic therapy and supportive care including mechanical ventilation if necessary. Treatment of CAP varies based on the area of practice and severity of the disease. Patients with low-risk CAP are typically treated as an outpatient with macrolide monotherapy. Respiratory fluoroquinolones are used in outpatient patients at higher risk. Non-ICU inpatients are treated with a dual therapy of a b-lactam plus a macrolide or respiratory fluoroquinolone monotherapy. Patients admitted to the ICU should be treated with a dual therapy of either a b-lactam plus a macrolide or a b-lactam plus respiratory fluoroquinolone. A recent Cochrane review shows the non-superiority of any outpatient antibiotic regimen for CAP concerning the other drug classes.[12][13][14](B3)
The first dose of antibiotics should be given as quickly as possible after the definitive diagnosis. The ACEP policy statement gives a level B recommendation that there is not enough evidence to establish a benefit in mortality or morbidity from starting the antibiotics in less than 4, 6, or 8 hours. The ACEP clinical policy also notes that there is not enough evidence to determine if there is a benefit in morbidity or mortality from antibiotics being administered within any specific time course but recommends to begin antibiotics as soon as the diagnosis is made. Patients with complicated pneumonia having parapneumonic effusion may need a tube thoracostomy and if it further progresses to empyema and is resistant to drainage by tube thoracostomy then decortication is required with video-assisted thoracoscopic surgery (VATS).
Differential Diagnosis
There are no specific signs and symptoms for pneumococcal pneumonia so whenever the diagnosis of pneumococcal pneumonia is considered following differentials should be kept in mind.
- Viral pneumonia
- PCP
- Influenza
- Klebsiella pneumonia
- Legionella pneumonia
- Pleural effusion
- Upper respiratory tract infection
Complications
Pneumococcal pneumonia, if not treated by appropriate antibiotics at an appropriate time or caused by a more virulent/resistant strains, can lead to the following complications.
- Necrotizing pneumonia
- Lung abscess
- Parapneumonic effusion
- Empyema
- Septicemia, Septic shock
Consultations
- Pulmonary Physician
- Infectious disease consultant
- Microbiologist
- May need an Intensive care physician in severe cases
Deterrence and Patient Education
Universal childhood immunization with a conjugate pneumococcal vaccine should be done. All individuals who are at increased risk of acquiring pneumococcal infection like old age people more than 65 years old, patients with underlying lung disease, alcoholics, with chronic kidney and liver diseases, who are undergoing splenectomy or have functional asplenia should be vaccinated.
Cigarette smoking has been found to increase the risk of pneumococcal infection in otherwise healthy people. Therefore smoking cessation should be encouraged. Good nutrition, healthy environment and avoidance of daycare attendance decrease the frequency of acquiring the infection.
Pearls and Other Issues
There are two vaccines commonly used for S. pneumoniae. The pneumococcal polysaccharide vaccine, PPSV23, and the pneumococcal conjugate vaccine, PCV13. In immunocompetent individuals, five doses of PCV13 are recommended during infancy and childhood. A repeat dose of PCV13 at age 65 is recommended followed by a dose of PSV23 one year later. In randomized control trials, PCV13 was shown to prevent the first episode of vaccine-serotype pneumococcal pneumonia. Although these vaccines have made great strides in decreasing S. pneumoniae pneumonia, there a number of serotypes not included in these vaccines. Although between the two vaccines the most prevalent serotypes are covered, there are approximately 90 serotypes in total and the vaccine will not foster immunity in all serotypes. Finally, it has been shown that influenza vaccination has a strong association with better outcomes and a decreased rate of pneumonia.
Enhancing Healthcare Team Outcomes
Streptococcal pneumonia is best managed with an interprofessional team that includes a pulmonologist, an infectious disease expert, an ICU nurse, a pharmacist, a respiratory therapist, and a dietitian. Patients need to be educated on the importance of vaccination and its benefits. In addition, patients should be advised to stop smoking and remain compliant with antibiotics. Since many patients with pneumonia are frail, a dietary consult should be sought to help improve the calorie intake. Others may need rehabilitation to restore muscle mass and increase exercise endurance. [15][16](Level V)
Outcomes
The prognosis for patients with streptococcal pneumonia depends on the underlying risk factors, comorbidity, age, the extent of lung involvement, the need for mechanical ventilation and the type of antibiotic. Overall, the pneumonia is associated with high morbidity and mortality. Even those who survive tend to have residual deficits in lung mechanics and recovery is prolonged. Patients in the ICU tend to have the highest mortality approaching 3-20%. [1][17](level V)
Media
(Click Image to Enlarge)
References
Luna CM, Pulido L, Niederman MS, Casey A, Burgos D, Leiva Agüero SD, Grosso A, Membriani E, Entrocassi AC, Rodríquez Fermepin M, Vay CA, Garcia S, Famiglietti A. Decreased relative risk of pneumococcal pneumonia during the last decade, a nested case-control study. Pneumonia (Nathan Qld.). 2018:10():9. doi: 10.1186/s41479-018-0053-6. Epub 2018 Sep 25 [PubMed PMID: 30263884]
Level 2 (mid-level) evidenceCillóniz C, Dominedò C, Garcia-Vidal C, Torres A. Community-acquired pneumonia as an emergency condition. Current opinion in critical care. 2018 Dec:24(6):531-539. doi: 10.1097/MCC.0000000000000550. Epub [PubMed PMID: 30239410]
Level 3 (low-level) evidenceShoji H, Vázquez-Sánchez DA, Gonzalez-Diaz A, Cubero M, Tubau F, Santos S, García-Somoza D, Liñares J, Yuste J, Martí S, Ardanuy C. Overview of pneumococcal serotypes and genotypes causing diseases in patients with chronic obstructive pulmonary disease in a Spanish hospital between 2013 and 2016. Infection and drug resistance. 2018:11():1387-1400. doi: 10.2147/IDR.S165093. Epub 2018 Sep 4 [PubMed PMID: 30214260]
Level 3 (low-level) evidenceRegev-Yochay G,Chowers M,Chazan B,Gonzalez E,Gray S,Zhang Z,Pride M, Distribution of 13-Valent pneumococcal conjugate vaccine serotype streptococcus pneumoniae in adults 50 Years and Older presenting with community-acquired pneumonia in Israel. Human vaccines [PubMed PMID: 30188760]
Quah J, Jiang B, Tan PC, Siau C, Tan TY. Impact of microbial Aetiology on mortality in severe community-acquired pneumonia. BMC infectious diseases. 2018 Sep 4:18(1):451. doi: 10.1186/s12879-018-3366-4. Epub 2018 Sep 4 [PubMed PMID: 30180811]
Ghaffar F, Friedland IR, McCracken GH Jr. Dynamics of nasopharyngeal colonization by Streptococcus pneumoniae. The Pediatric infectious disease journal. 1999 Jul:18(7):638-46 [PubMed PMID: 10440444]
Alqahtani AS, Tashani M, Ridda I, Gamil A, Booy R, Rashid H. Burden of clinical infections due to S. pneumoniae during Hajj: A systematic review. Vaccine. 2018 Jul 16:36(30):4440-4446. doi: 10.1016/j.vaccine.2018.04.031. Epub 2018 Jun 20 [PubMed PMID: 29935859]
Level 1 (high-level) evidenceWahl B, O'Brien KL, Greenbaum A, Majumder A, Liu L, Chu Y, Lukšić I, Nair H, McAllister DA, Campbell H, Rudan I, Black R, Knoll MD. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000-15. The Lancet. Global health. 2018 Jul:6(7):e744-e757. doi: 10.1016/S2214-109X(18)30247-X. Epub [PubMed PMID: 29903376]
Boeddha NP, Schlapbach LJ, Driessen GJ, Herberg JA, Rivero-Calle I, Cebey-López M, Klobassa DS, Philipsen R, de Groot R, Inwald DP, Nadel S, Paulus S, Pinnock E, Secka F, Anderson ST, Agbeko RS, Berger C, Fink CG, Carrol ED, Zenz W, Levin M, van der Flier M, Martinón-Torres F, Hazelzet JA, Emonts M, EUCLIDS consortium. Mortality and morbidity in community-acquired sepsis in European pediatric intensive care units: a prospective cohort study from the European Childhood Life-threatening Infectious Disease Study (EUCLIDS). Critical care (London, England). 2018 May 31:22(1):143. doi: 10.1186/s13054-018-2052-7. Epub 2018 May 31 [PubMed PMID: 29855385]
Bellew S, Grijalva CG, Williams DJ, Anderson EJ, Wunderink RG, Zhu Y, Waterer GW, Bramley AM, Jain S, Edwards KM, Self WH. Pneumococcal and Legionella Urinary Antigen Tests in Community-acquired Pneumonia: Prospective Evaluation of Indications for Testing. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019 May 30:68(12):2026-2033. doi: 10.1093/cid/ciy826. Epub [PubMed PMID: 30265290]
Ishiguro T, Yoshii Y, Kanauchi T, Hoshi T, Takaku Y, Kagiyama N, Kurashima K, Takayanagi N. Re-evaluation of the etiology and clinical and radiological features of community-acquired lobar pneumonia in adults. Journal of infection and chemotherapy : official journal of the Japan Society of Chemotherapy. 2018 Jun:24(6):463-469. doi: 10.1016/j.jiac.2018.02.001. Epub 2018 Mar 28 [PubMed PMID: 29605556]
Osowicki J,Steer AC, International survey of paediatric infectious diseases consultants on the management of community-acquired pneumonia complicated by pleural empyema. Journal of paediatrics and child health. 2018 Jul 27 [PubMed PMID: 30051535]
Level 3 (low-level) evidenceJakhar SK, Pandey M, Shah D, Ramachandran VG, Saha R, Gupta N, Gupta P. Etiology and Risk Factors Determining Poor Outcome of Severe Pneumonia in Under-Five Children. Indian journal of pediatrics. 2018 Jan:85(1):20-24. doi: 10.1007/s12098-017-2514-y. Epub 2017 Oct 13 [PubMed PMID: 29027126]
Lewandowska K, Kuś J. [Community acquired pneumonia - treatment options according to the international recommendations]. Wiadomosci lekarskie (Warsaw, Poland : 1960). 2016:69(2 Pt 1):139-44 [PubMed PMID: 27421128]
Green C, Moore CA, Mahajan A, Bajaj K. A Simple Approach to Pneumococcal Vaccination in Adults. Journal of global infectious diseases. 2018 Jul-Sep:10(3):159-162. doi: 10.4103/jgid.jgid_88_17. Epub [PubMed PMID: 30166816]
Herbert JA, Kay EJ, Faustini SE, Richter A, Abouelhadid S, Cuccui J, Wren B, Mitchell TJ. Production and efficacy of a low-cost recombinant pneumococcal protein polysaccharide conjugate vaccine. Vaccine. 2018 Jun 18:36(26):3809-3819. doi: 10.1016/j.vaccine.2018.05.036. Epub 2018 May 25 [PubMed PMID: 29778517]
Blot M, Pauchard LA, Dunn I, Donze J, Malnuit S, Rebaud C, Croisier D, Piroth L, Pugin J, Charles PE. Mechanical ventilation and Streptococcus pneumoniae pneumonia alter mitochondrial homeostasis. Scientific reports. 2018 Aug 6:8(1):11718. doi: 10.1038/s41598-018-30226-x. Epub 2018 Aug 6 [PubMed PMID: 30082877]