Introduction
Subclavian artery thrombosis is a condition characterized by the formation of a blood clot within the subclavian artery, a large blood vessel located in the shoulder region. Thrombosis can significantly reduce blood supply to the vessel's distribution area, often the ipsilateral upper extremity. Rarely, the condition can affect the brain and heart. Complete stenosis from subclavian artery thrombosis may be considered a medical emergency, potentially causing limb loss and stroke if not treated promptly.
Symptoms of subclavian artery thrombosis may include pain, numbness, weakness, or coolness in the affected limb, particularly during physical activity or with certain arm positions. In severe cases, individuals may experience ischemia symptoms, such as skin color changes or even gangrene. Subclavian artery thrombosis can occur due to various factors, including atherosclerosis, hypercoagulable states, trauma, or certain medical procedures.[1]
A combination of thorough clinical evaluation and imaging studies, particularly Doppler ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA), is critical to diagnosis. Treatment aims to restore circulation in the affected artery and prevent complications. Nonsurgical and surgical interventions are recommended, depending on the extent of thrombosis and the patient's risk factors. These interventions include anticoagulant therapy and thrombolytic therapy, thrombectomy, and angioplasty with stent placement. Notably, the treatment is graded depending on the severity and after assessing the risk of potential complications. Overall, subclavian artery thrombosis is a serious condition requiring prompt and appropriate management to prevent long-term complications and preserve limb function.
Subclavian Artery Anatomy
The subclavian artery originates from the brachiocephalic trunk on the right side and the aortic arch on the left side. This artery supplies the upper limb, neck, and brain, coursing through the chest from its origin and traversing the thoracic outlet beneath the clavicle and over the 1st rib before reaching the axilla. Along its path, the subclavian artery gives rise to several branches, each serving distinct anatomical areas and functions.
The subclavian artery consists of 3 parts. The 1st part extends from the subclavian artery's origin to the anterior scalene muscle's medial border. The 2nd part lies posterior to the anterior scalene muscle. The 3rd part courses from the anterior scalene's lateral border to the 1st rib's lateral border. The subclavian artery's branches include the vertebral artery, internal mammary artery (IMA), thyrocervical trunk, costocervical trunk, and dorsal scapular artery. On the left side, all branches except the dorsal scapular artery arise from the 1st part. On the right side, the costocervical trunk typically originates from the 2nd part.
The vertebral artery emanates from the 1st part of the subclavian artery and ascends through the cervical vertebrae's transverse foramina to supply the brain and spinal cord. When the subclavian artery is narrowed or blocked, blood from the contralateral vertebral artery or other intracranial collaterals can flow retrogradely through the vertebrobasilar system to help maintain brain perfusion. This collateral circulation can mitigate the risk of cerebral ischemia and stroke in individuals with subclavian artery stenosis, providing a vital compensatory mechanism to preserve brain function.
The IMA, also called the "internal thoracic artery," descends along the chest wall's inner surface and provides blood to the chest wall and breasts. This artery is often involved in coronary artery bypass grafting (CABG). The thyrocervical trunk divides into the inferior thyroid, transverse cervical, and suprascapular arteries, which supply blood to the thyroid gland, neck muscles, and shoulder region, respectively. The costocervical trunk distributes blood to the upper intercostal spaces, deep neck muscles, and superior spinal cord portions. The dorsal scapular artery, arising either separately or as a transverse cervical artery branch, nourishes the shoulder girdle and back muscles. The subclavian artery transitions into the axillary artery after passing the 1st rib's lateral border.
The subclavian artery supplies vast areas in the head, neck, and upper limb. Knowledge of this artery's anatomy is vital for diagnosing and treating conditions like subclavian artery thrombosis and conducting surgical procedures in the shoulder, arm, and neck regions.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The most widely recognized etiology of subclavian artery thrombosis is atherosclerosis. Uncommon etiologies include congenital deformities, fibromuscular dysplasia, neurofibromatosis, autoimmune vasculitis, radiation exposure, neurofibromatosis, inadvertent puncture, and mechanical causes, including injury or compression disorders.[2][3]
Epidemiology
The incidence of subclavian artery thrombosis in patients with peripheral vascular disease is approximately 11% to 18%.[4] Patients with subclavian artery thrombosis have a 50% likelihood of concurrent coronary artery disease (CAD), a 27% probability of lower extremity artery disease, and a 29% chance of concomitant carotid artery disease.[5]
Patients with subclavian artery thrombosis have an elevated risk of developing CAD, transient ischemic attack, and cerebrovascular ischemia or infarction because of these conditions' shared pathogenesis. This risk correlates more with left-sided lesions.[6][7][8]
Subclavian artery thrombosis is believed to be underdiagnosed. The disease is 4 times more common in the left subclavian artery than in the right.
Pathophysiology
Subclavian artery thrombosis risk factors are the same as in thrombosis in any other body part, including obesity, hypertension, diabetes mellitus, smoking, and metabolic syndrome. Like similar events in other regions, subclavian artery thrombosis involves an area subjected to increased shear stress, leading to endothelial injury, subsequent platelet aggregation, and release of platelet-derived growth factor. This sequence triggers smooth muscle cell proliferation in the arterial intima and forms the locus of the atherosclerotic plaque.
History and Physical
The presence of symptoms after subclavian artery thrombosis occurs depends on collateralization. Upper limb symptoms comprise arm claudication or muscle fatigue, rest pain, and finger necrosis from embolic debris.
Vertebrobasilar insufficiency may develop when subclavian artery thrombosis is proximal to the vertebral artery's origin. Conditions of increased flow distal to the stenosis, like exercise, result in retrograde flow in the vertebral artery, followed by decreased flow in the basilar artery. Vertebrobasilar hypoperfusion may produce neurologic symptoms, including visual abnormalities (diplopia), drop attacks, syncope, ataxia, vertigo, dysphasia, dysarthria, dizziness, nystagmus, tinnitus, hearing loss, and facial sensory deficits.
Angina pectoris is a rare complication of subclavian stenosis in a patient who has had CABG with the IMA. The IMA arises from the subclavian artery and can be affected by stenosis. Thrombosis proximal to the IMA graft impairs blood flow to the IMA. In severe stenosis, retrograde flow from the grafted coronary artery to the brachial artery may lead to angina, a phenomenon called "coronary steal syndrome."
Physical examination with a detailed cardiovascular assessment may reveal unequal blood pressure in the arms, absent or diminished upper limb pulses compared to the contralateral arm, and cervical or supraclavicular bruits. Ischemic findings such as gangrenous skin changes of the fingers or nail bed splinter hemorrhages may be present. The physical examination should also encompass cerebral circulation evaluation and include palpation of the carotid pulses and auscultation for vertebral and carotid bruits. An interarm systolic blood pressure difference of less than 10 mm Hg has a negative predictive value of 99%.
Clinical clues suggesting subclavian artery stenosis include unequal upper limb blood pressures, absent or diminished axillary, brachial, radial, or ulnar pulses, and digital ulceration or gangrene. A difference in systolic blood pressure of over 10 mm Hg between both arms has a positive predictive value of 13%. However, the positive predictive value increases from 67% to 100%, and the negative predictive value rises to 100% if the systolic cutoff increases to 15 or 20 mm Hg.[9][10]
High-grade stenosis from subclavian artery thrombosis is a vascular emergency that poses a significant threat to limb viability and neurological function. Given the potential for limb loss and catastrophic neurological sequelae, recognizing the clinical presentation and promptly initiating appropriate evaluation and treatment are paramount.
Evaluation
Duplex ultrasound with color flow is an excellent initial noninvasive imaging test for subclavian artery thrombosis. Common findings on Duplex ultrasonography include waveform dampening or monophasic changes, color aliasing suggesting turbulent flow, and increased blood flow velocity at the stenotic site. Doppler ultrasonography can also identify ipsilateral vertebral artery flow reversal, often seen in subclavian steal syndrome.
High-velocity flow on Doppler ultrasonography indicates a greater than 50% stenosis in the thrombosed area. However, differentiating high-grade subclavian artery ostial stenosis from complete obstructive lesions is challenging. Most subclavian artery ostial lesions are located proximally. Features suggestive of high-grade, greater than 70% proximal subclavian arterial stenosis include monophasic poststenotic flow and altered flow in the ipsilateral vertebral artery.
Detailed Duplex ultrasonographic evaluations are necessary to identify a severely stenotic or obstructed right brachiocephalic trunk. Reduced flow velocities in the right subclavian and common carotid arteries indicate the presence of higher-grade stenotic lesions in the right brachiocephalic trunk.[11] Further assessment of these lesions requires anatomic imaging studies, including CTA and MRA.
CTA can provide comprehensive extravascular information, vital in ruling out vascular thoracic outlet syndrome. Moreover, supra-aortic lesions may be easily distinguished via CTA.[12]
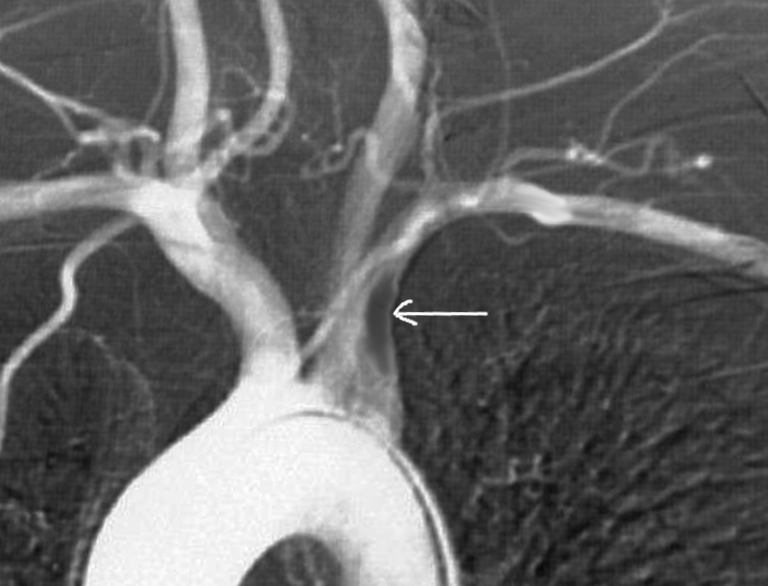
More accurate diagnostic modalities like MRA and multidetector CT (MDCT) angiography are reserved for cases wherein intervention is mandatory. MRA provides both morphological and functional characteristics, enables optimal differentiation, and measures stenotic severity (see Image. Subclavian Artery Thrombosis on Magnetic Resonance Angiography). MDCT angiography generates detailed images of pathological subclavian artery conditions. Attention must be given to specific factors to ensure the highest quality MDCT examination for evaluating subclavian artery thrombosis. These factors include proper arm positioning, optimal technique for applying contrast material, meticulous data acquisition, and appropriate reconstruction parameters.
Screening for subclavian artery stenosis is indicated in patients with possible subclavian stenosis under consideration for CABG involving the IMA. Additionally, screening is advised for individuals with a history of peripheral artery disease or a notable systolic blood pressure disparity exceeding 10 mm Hg between their upper limbs.[13] Diagnosis is confirmed after finding left vertebral artery blood flow reversal on Doppler ultrasound and angiographic confirmation of severe left subclavian artery.
Treatment / Management
Timely treatment of subclavian artery stenosis is paramount to salvage limb viability and prevent potentially life-altering sequelae such as limb loss or stroke. The management strategy may involve pharmacological, endovascular, surgical, or combined interventions tailored to the patient's presentation and underlying vascular pathology.
Treatment Indications
Treatment decisions for subclavian artery thrombosis are based on a comprehensive assessment of clinical presentation, imaging findings, risk factors, and patient-specific factors. The primary management goal is to optimize outcomes and preserve limb and vascular health. Treatment indications include the following:
- Morbid upper arm ischemia (57%)
- Upper limb claudication
- Upper extremity pain at rest
- Fingers embolization
- Vertebrobasilar insufficiency from steal syndrome (37%)
- Anginal symptoms from coronary steal via intermammary artery graft (21%)
- Leg claudication in the presence of axillofemoral graft
Medical therapy includes aspirin or clopidogrel, HMG-CoA reductase inhibitors, and angiotensin receptor blockers or angiotensin-converting enzyme inhibitors. Patients must be counseled to refrain from smoking. Individuals with diabetes should be placed on strict glycemic control, with a target HbA1c below 7.
Surgical Intervention
Operative management indications include symptomatic subclavian artery disease, critical limb ischemia, failure of medical therapy, high-risk patients, presence of contraindications to endovascular intervention, patient preference, and prevention of complications. High-risk patients include those with severe comorbidities, extensive arterial disease, or poor response to medical therapy. Surgical treatments include the axillary–axillary and carotid-subclavian bypass procedures and subclavian artery transposition.[14] The axillary–axillary bypass surgery is associated with reduced morbidity and mortality.[15]
Endovascular intervention, including percutaneous transluminal angioplasty with stenting or ballooning, is the best modality for relieving subclavian artery thrombosis. These minimally invasive modalities have demonstrated high success rates in restoring patency to the subclavian artery and improving stenosis symptoms.[16](B2)
Rheolytic pharmacomechanical thrombectomy (PMT) using the Angiojet® device is a recognized method for treating acute arterial thrombosis. This approach combines thrombolytic therapy with mechanical thrombus removal using a thrombectomy catheter or prolonged infusion, often facilitated by an indwelling catheter. Thus, the procedure is a catheter-directed thrombolysis.
A study showed that patients treated with PMT alone had improved outcomes compared to patients who underwent combined catheter-directed thrombolysis and PMT, with higher procedural success rates and 12-month amputation-free survival. These findings were reported in the Peripheral Use of AngioJet Rheolytic (PEARL) Thrombectomy registry, which included various catheter lengths. Notably, only a small percentage (3%) of patients in the PEARL registry had upper extremity acute limb ischemia.
Revascularization
Risk factor control and medical therapy for cardiovascular risk reduction are recommended in all patients with symptomatic upper extremity artery disease.[17] However, management of subclavian artery pathologies with revascularization is indicated in symptomatic patients with the following:(B2)
- Signs and symptoms indicative of a transient ischemic attack or stroke
- Signs and symptoms suggestive of coronary subclavian steal syndrome
- Ipsilateral hemodialysis access dysfunction
- Impaired quality of life [18] (B2)
Moreover, revascularization should be considered in asymptomatic patients in the following circumstances:
- Planned CABG with the IMA
- Patients with ipsilateral hemodialysis vascular access
- Significant bilateral subclavian stenosis or occlusion
Both endovascular and surgical procedures are recommended if contemplating revascularization. According to recent reviews, the results of the endovascular and open repair and significant complications, including vertebrobasilar and postprocedural stroke, were comparable. Still, no randomized clinical trials have evaluated the outcome differences between endovascular and open repair in managing subclavian artery pathologies. The risk of severe complications, including vertebrobasilar stroke, is low with both approaches.[19][20](B2)
Severe thrombotic stenosis management
The following stepwise management has been recommended in a case report to address severe thrombotic left proximal subclavian artery stenosis:
- Placing a long guiding sheath
- Placing an antiembolic filter into the left brachial artery (recommended for distal protection)
- Inflating a blood pressure cuff over the left brachial artery. The cuff should be inflated for pressures above the maximum systolic arterial blood pressure for 10 minutes.
- Inflating a coronary balloon catheter specifically along the 1st segment of the vertebral artery, at the origin of the left subclavian artery's origin.
- Placing a peripheral stent, dilated distal to the subclavian stenosis
- Deflating the jailed balloon, blood pressure cuff, and postdilation balloon sequentially
- Performing control angiography after jailed balloon catheter retrieval
Control angiography is conducted to assess the success of the intervention, confirm adequate dilation and stent placement, and detect any residual stenosis or complications that may require further intervention.
Differential Diagnosis
The differential diagnosis of subclavian artery stenosis includes the following:
- Congenital malformations, such as an aberrant subclavian artery or cervical rib, may mimic subclavian artery thrombosis symptoms.
- Fibromuscular dysplasia also presents with arterial narrowing or stenosis secondary to abnormal vessel wall structure.
- Neurofibromatosis may manifest with vascular abnormalities, potentially leading to symptoms akin to those of subclavian artery thrombosis.
- Autoimmune vasculitis like Takayasu arteritis can cause inflammation and stenosis of the subclavian artery, mimicking thrombotic occlusion.
- Radiation exposure may induce subclavian artery fibrosis and stenosis, producing thrombotic occlusion symptoms.
- Mechanical causes, such as trauma or compression syndromes like thoracic outlet syndrome, can impede blood flow through the subclavian artery, resembling thrombotic occlusion.
A combination of clinical evaluation and characteristic diagnostic findings differentiates subclavian artery stenosis from these conditions.
Prognosis
The prognosis of subclavian artery thrombosis hinges upon multiple factors, notably the severity of the blockage, timeliness of medical intervention, presence of comorbid conditions, degree of tissue damage, treatment response, and development of complications. Prolonged, complete occlusion may produce life-altering complications such as limb loss or stroke. Partial blockages may present with milder symptoms or remain asymptomatic. Swift recognition and revascularization are imperative for a favorable prognosis. Comorbid conditions can make invasive procedures contraindicated in some patients, possibly delaying revascularization and tissue healing.
The degree of tissue damage also impacts prognosis, with potential complications including limb ischemia, stroke, or mortality in severe cases. Successful and prompt revascularization significantly improves outcomes. Complications like recurrent thrombosis may negatively affect long-term prognosis.
Complications
The complications of subclavian artery thrombosis include the following:
- Morbid upper arm ischemia (57%)
- Upper limb claudication
- Upper extremity pain at rest
- Fingers embolization
- Vertebrobasilar insufficiency from steal syndrome (37%)
- Anginal symptoms from coronary steal via IMA graft (21%)
- Leg claudication in the presence of axillofemoral graft
Procedural complications are as follows:
- Stroke
- Subclavian artery dissection
- Transient ischemic attack (TIA)
- Distal emboli
- Thrombosis
- Hematoma
- Bleeding
- Access site infection or bleeding[20]
Protective measures against vertebral artery plaque shift and cerebral and distal limb embolism include using a filter and jailed balloon and noninvasive measures that induce reactive hyperemia, such as blood pressure cuff inflation and release.[21]
Deterrence and Patient Education
Preventive measures for subclavian artery thrombosis include various strategies to reduce the risk of vascular complications. Lifestyle modifications, including smoking cessation, regular exercise, and a healthy diet, help prevent atherosclerosis and vascular disease development. Effective blood pressure, cholesterol, and diabetes management help prevent arterial damage and reduce thrombotic risk. Regular medical check-ups enable early detection of vascular abnormalities and identification of thrombosis risk factors. Occupational safety measures, such as ergonomic practices and protective equipment, can mitigate vascular injury in highly physical occupations. Raising awareness about subclavian artery thrombosis' signs and symptoms promotes early recognition and timely intervention, improving outcomes and reducing the incidence of thrombotic events.
Pearls and Other Issues
Subclavian artery thrombosis occurs when a blood clot forms in the subclavian artery, resulting in reduced blood flow to the affected upper limb and potentially the brain. Patients may experience symptoms such as arm or hand pain, weakness, numbness, or coldness, which may vary depending on stenosis severity and collateral circulation development. Neurologic and cardiac symptoms may manifest in severe cases. Risk factors for subclavian artery thrombosis include atherosclerosis, smoking, hypertension, diabetes, hyperlipidemia, trauma, and certain medical conditions like vasculitis or hypercoagulable states.
Diagnosis involves clinical evaluation and imaging studies such as Doppler ultrasound, CTA, and MRA. Treatment aims to restore circulation and prevent complications through anticoagulation, thrombolysis, or surgical interventions like thrombectomy or angioplasty with stent placement. Chronic cases may develop collateral circulation, alleviating some symptoms but not fully restoring function.
Complications of untreated thrombosis include limb ischemia, digital gangrene, and stroke. Long-term follow-up is mandatory to monitor for recurrence, assess vascular health, and manage underlying risk factors. Rehabilitation may be needed to regain function and mobility in the affected arm or hand. Prevention strategies include lifestyle modifications and effective management of cardiovascular risk factors. Given the complexity of management, a multidisciplinary approach involving vascular surgeons, interventional radiologists, cardiologists, and rehabilitation specialists is often required to provide comprehensive care.
Enhancing Healthcare Team Outcomes
Subclavian artery thrombosis is a rare emergency that requires management by a team of healthcare professionals. This team should include an emergency medicine physician, cardiologist, vascular surgeon, interventional radiologist, nursing staff, pharmacists, rehabilitation specialists, and primary care physicians.
Emergency physicians can rapidly assess and stabilize patients, initiate appropriate diagnostic modalities, and provide initial treatment to relieve symptoms and prevent further complications before referring to the appropriate specialist. Emergency medicine physicians may order diagnostic imaging studies to confirm the diagnosis and determine thrombosis severity in suspected cases. These health professionals may also administer medications such as antiplatelet agents or anticoagulants to prevent thrombus propagation and manage pain.
Cardiologists are vital in managing cardiovascular risk factors and providing medical therapy, including antiplatelet agents and anticoagulants, to prevent thrombus formation and complications. Vascular surgeons are responsible for performing surgical interventions to restore blood flow. Interventional radiologists contribute expertise in minimally invasive procedures like percutaneous transluminal angioplasty with stenting, offering alternatives to traditional surgery.
Nurses assist with preoperative preparation, intraoperative support, and postoperative management while educating patients about preventive measures and self-care strategies. Pharmacists ensure appropriate medication management, monitoring for potential drug interactions and adverse effects, and providing counseling on medication adherence. Rehabilitation specialists focus on optimizing functional outcomes in patients with limb ischemia, aiding in recovery and improving quality of life. Primary care physicians coordinate overall care, facilitating communication between team members and ensuring continuity of care throughout the patient's treatment journey.
Team members can provide patients with the best possible care by interprofessional collaboration. Communication and coordination among these interprofessional team members are essential for delivering comprehensive, patient-centered care and optimizing outcomes for individuals with subclavian artery thrombosis.
Media
(Click Image to Enlarge)
References
Jones CS, Verde F, Johnson PT, Fishman EK. Nontraumatic Subclavian Artery Abnormalities: Spectrum of MDCT Findings. AJR. American journal of roentgenology. 2016 Aug:207(2):434-41. doi: 10.2214/AJR.15.15685. Epub 2016 May 17 [PubMed PMID: 27187867]
Ochoa VM, Yeghiazarians Y. Subclavian artery stenosis: a review for the vascular medicine practitioner. Vascular medicine (London, England). 2011 Feb:16(1):29-34. doi: 10.1177/1358863X10384174. Epub 2010 Nov 15 [PubMed PMID: 21078767]
Tolerico PH, Harvey JE, Benton SM, Patel MD, Nicholson WJ. Acute Catheter-Induced Subclavian Artery Thrombosis Treated with Endovascular Stent Graft Placement and Rheolytic Thrombectomy: A Case Report and Review. Cardiovascular revascularization medicine : including molecular interventions. 2019 Nov:20(11S):31-33. doi: 10.1016/j.carrev.2019.02.021. Epub 2019 Mar 1 [PubMed PMID: 30857976]
Level 3 (low-level) evidenceEnglish JA, Carell ES, Guidera SA, Tripp HF. Angiographic prevalence and clinical predictors of left subclavian stenosis in patients undergoing diagnostic cardiac catheterization. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2001 Sep:54(1):8-11 [PubMed PMID: 11553941]
Rodriguez-Lopez JA, Werner A, Martinez R, Torruella LJ, Ray LI, Diethrich EB. Stenting for atherosclerotic occlusive disease of the subclavian artery. Annals of vascular surgery. 1999 May:13(3):254-60 [PubMed PMID: 10347257]
Hennerici M, Rautenberg W, Mohr S. Stroke risk from symptomless extracranial arterial disease. Lancet (London, England). 1982 Nov 27:2(8309):1180-3 [PubMed PMID: 6128493]
Moran KT, Zide RS, Persson AV, Jewell ER. Natural history of subclavian steal syndrome. The American surgeon. 1988 Nov:54(11):643-4 [PubMed PMID: 3189998]
Williams SJ 2nd. Chronic upper extremity ischemia: current concepts in management. The Surgical clinics of North America. 1986 Apr:66(2):355-75 [PubMed PMID: 2937168]
Osborn LA, Vernon SM, Reynolds B, Timm TC, Allen K. Screening for subclavian artery stenosis in patients who are candidates for coronary bypass surgery. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2002 Jun:56(2):162-5 [PubMed PMID: 12112906]
Lobato EB, Kern KB, Bauder-Heit J, Hughes L, Sulek CA. Incidence of coronary-subclavian steal syndrome in patients undergoing noncardiac surgery. Journal of cardiothoracic and vascular anesthesia. 2001 Dec:15(6):689-92 [PubMed PMID: 11748514]
Dubey G, Gupta SK, Kothari SS. Isolated left brachiocephalic artery with the right aortic arch: A rare differential of large patent ductus arteriosus. Annals of pediatric cardiology. 2017 Jan-Apr:10(1):78-81. doi: 10.4103/0974-2069.197067. Epub [PubMed PMID: 28163435]
Tong E, Rizvi T, Hagspiel KD. Complex aortic arch anomaly: Right aortic arch with aberrant left subclavian artery, fenestrated proximal right and duplicated proximal left vertebral arteries-CT angiography findings and review of the literature. The neuroradiology journal. 2015 Aug:28(4):396-403. doi: 10.1177/1971400915598075. Epub 2015 Aug 25 [PubMed PMID: 26306929]
Costa SM, Fitzsimmons PJ, Terry E, Scott RC. Coronary-subclavian steal: case series and review of diagnostic and therapeutic strategies: three case reports. Angiology. 2007 Apr-May:58(2):242-8 [PubMed PMID: 17495276]
Level 3 (low-level) evidenceSHIMIZU K, SANO K. Pulseless disease. Journal of neuropathology and clinical neurology. 1951 Jan:1(1):37-47 [PubMed PMID: 24538949]
Chang JB, Stein TA, Liu JP, Dunn ME. Long-term results with axillo-axillary bypass grafts for symptomatic subclavian artery insufficiency. Journal of vascular surgery. 1997 Jan:25(1):173-8 [PubMed PMID: 9013922]
Angle JF, Matsumoto AH, McGraw JK, Spinosa DJ, Hagspiel KD, Leung DA, Tribble CG. Percutaneous angioplasty and stenting of left subclavian artery stenosis in patients with left internal mammary-coronary bypass grafts: clinical experience and long-term follow-up. Vascular and endovascular surgery. 2003 Mar-Apr:37(2):89-97 [PubMed PMID: 12669139]
Level 2 (mid-level) evidenceClark CE, Greaves CJ, Evans PH, Dickens A, Campbell JL. Inter-arm blood pressure difference in type 2 diabetes: a barrier to effective management? The British journal of general practice : the journal of the Royal College of General Practitioners. 2009 Jun:59(563):428-32. doi: 10.3399/bjgp09X420752. Epub [PubMed PMID: 19520026]
Level 2 (mid-level) evidenceSalman R, Hornsby J, Wright LJ, Elsaid T, Timmons G, Mudawi A, Bhattacharya V. Treatment of subclavian artery stenosis: A case series. International journal of surgery case reports. 2016:19():69-74. doi: 10.1016/j.ijscr.2015.12.011. Epub 2015 Dec 17 [PubMed PMID: 26722712]
Level 2 (mid-level) evidenceDuran M, Grotemeyer D, Danch MA, Grabitz K, Schelzig H, Sagban TA. Subclavian carotid transposition: immediate and long-term outcomes of 126 surgical reconstructions. Annals of vascular surgery. 2015 Apr:29(3):397-403. doi: 10.1016/j.avsg.2014.09.030. Epub 2014 Nov 24 [PubMed PMID: 25463327]
Level 2 (mid-level) evidenceAboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I, ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). European heart journal. 2018 Mar 1:39(9):763-816. doi: 10.1093/eurheartj/ehx095. Epub [PubMed PMID: 28886620]
Vuruşkan E, Saraçoğlu E, Polat M, Düzen İV. Case images: Treatment of thrombotic subclavian artery stenosis involving vertebral artery ostium with maximum protection. Turk Kardiyoloji Dernegi arsivi : Turk Kardiyoloji Derneginin yayin organidir. 2017 Mar:45(2):207. doi: 10.5543/tkda.2016.93727. Epub [PubMed PMID: 28424448]
Level 3 (low-level) evidence