Introduction
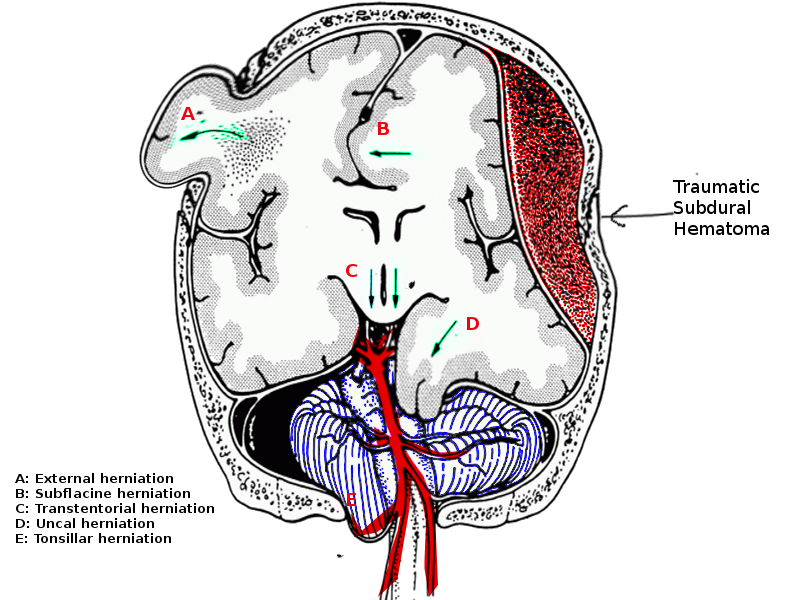
Herniation occurs when brain tissue is displaced across a structure within the cranium. Subfalcine herniation is the most common form of intracranial herniation and occurs when brain tissue is displaced under the falx cerebri. The cingulate gyrus is herniated under the falx, and if progression occurs, other areas of the frontal lobe are involved.
Once the fontanels close in infancy, the cranium becomes a closed rigid structure with a fixed volume containing three components; the brain, the cerebrospinal fluid (CSF), and intracerebral blood. The Monroe-Kellie doctrine states that intracranial volume is constant, and an increase in the volume of one component will cause a decrease in the volume of one or both of the others. This change can have significant effects, such as decreased cerebral blood flow or herniation of brain tissue. When herniation occurs, the location of the herniation determines the presenting symptoms and the clinical outcomes.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Subfalcine herniation is a secondary intracranial injury caused by several primary injuries. The list below represents a sample of lesions associated with subfalcine herniation. In each case, a change in volume in one compartment precedes herniation.[1][2]
- Increased brain volume
- Traumatic brain injury (TBI)
- Hemorrhage (epidural, subdural, intraparenchymal)
- Ischemia due to stroke
- Tumor
- Cytotoxic/vasogenic/osmotic edema
- Change in CSF volume
- Increase
- Choroid plexus tumor
- Obstructive hydrocephalus
- Non-obstructive hydrocephalus
- Pseudotumor cerebri
- Meningeal inflammation or granulomas
- Change in intracranial blood volume
- Increase
- Loss of autoregulation due to TBI
- Increased cerebral blood flow (hypercapnia, hypoxia)
- Venous sinus thrombosis
- Elevated right atrial pressure (heart failure)
- Acidosis
- Decrease
- Rapid decompression of a hematoma[7]
Epidemiology
Many sources affirm that subfalcine herniations are the most common type of brain herniation; however, not all agree. It is difficult to assess this because the prevalence and incidence of subfalcine herniation are not well documented. This is likely to occur because many patients have symptoms too subtle to require neuroimaging, or the patient's condition progressed too rapidly. The neuroimaging in the latter would not identify a subfalcine herniation but only the more catastrophic uncal, transtentorial, and the tonsillar herniations.
Although the epidemiology of subfalcine herniation is lacking, it is likely reflected in the epidemiology of those conditions noted to cause subfalcine herniation and ischemic events that might result from subfalcine herniation. TBI, brain tumors, and strokes are the leading causes. According to the Centers for Disease Control (CDC) and Prevention, TBI is a leading cause of death and disability in the United States among all races, ethnicities, social, economic levels, and age groups.[8]
Between 2002 and 2006, about 1.7 million US civilians sustained a TBI annually. Of these, approximately 1.4 million were treated and released from emergency departments, 275,000 were hospitalized and discharged alive, and 52,000 died. TBI-related deaths represent approximately one-third of injury-related deaths. These data are exclusive of members of the United States military who sustained a TBI while serving abroad and those patients who did not seek medical care. An estimated 25% of patients who sustain TBI do not seek medical care. As a result, the reported incidence is likely less than the true occurrence. Similarly, one might speculate that the true incidence of subfalcine herniation is less than reports of clinical data would suggest.[9]
The CDC reports suggest that children younger than five years of age have the highest rates of TBI, as evidenced by emergency department visits, hospital visits, and death secondary to TBI.[9] The next most frequently affected group is the adolescents aged 15 to 19 years, followed by adults 75 years of age or older. Older adults have the highest rates of TBI hospitalizations and deaths in all three age groups.
The incidences of ischemic strokes in infants, children, and adults younger than 45 years of age range from 0.62 to 7.9 per 100,000 children per year and 3.4 to 11.3 per 100,000 people per year for adults younger than 45 years old. The reported incidence rates were mostly in white populations. Studies report the incidence of ischemic stroke in young black adults to be as high as 22.8 per 100,000 people per year.[10]
If one accepts that the incidence rates of TBI and ischemic strokes reflect the incidence rate of a subfalcine herniation, healthcare personnel treating patients with TBI or stroke should maintain a high index of suspicion of the occurrence of subfalcine herniation in these patients.
Pathophysiology
Brain herniation occurs when a pressure difference is created on either side of a fixed intracranial structure; the pressure differential results from increases in brain volume as seen with tumors, localized hemorrhage, changes in CSF volume, or increases in blood volume. Compensatory mechanisms or autoregulation (CSF shift and blood volume shift) allow for the constant maintenance of intracranial pressure (ICP). When intracranial lesions exceed the capacity of native compensatory mechanisms, pressure increases, and herniation occurs. CSF opening pressures are used as surrogates for ICP though patient variables (position, sedation, level of activity) likely affect the accuracy of the measurement. As reflected by opening pressures, intracranial pressure in children normally ranges from 8 to 28 cm H20 pressure.[11][12]
The probability of herniation occurs when intracranial pressures exceed 28 cm H2O for more than 5 minutes.[13] When a lesion is causing a mass effect on the brain, the CSF volume and blood volume within the brain are decreased to maintain a normal ICP. As the lesion's volume increases and overwhelms the compensatory mechanism to maintain a normal ICP, the ICP increases, and the probability of herniation increases.
The falx cerebri is the sickle-shaped dura mater that spans the length of the cerebral hemispheres and extends downward into the longitudinal fissure, separating the cerebral hemispheres and leaving a free edge inferiorly. When there is a mass effect that could not be compensated for, brain tissue herniates under the falx cerebri causing subfalcine herniation.
History and Physical
A subfalcine herniation may not cause severe clinical symptoms initially. The initial presentation can be as benign as a headache. It is common to have headaches, nausea, vomiting, or altered mental status. When a patient develops a subfalcine herniation, the cingulate gyrus is forced under the falx cerebri and can compress the ipsilateral anterior cerebral artery resulting in contralateral leg weakness.[5] If the herniation affects the dominant hemisphere and involves the contralateral arcuate fasciculus, patients present with conduction aphasia, receptive/sensory aphasia, or expressive/motor aphasia.[14]
If the primary lesion becomes large enough, uncal or central herniation may develop. As the lesion grows and herniation becomes prominent, patients may develop anisocoria, a decreased level of consciousness, changes in respiratory pattern, changes in muscle tone, and abnormal motor posturing. Hypertension, bradycardia, and irregularly decreased respiration, comprising the classical Cushing triad, may be present, indicating imminent tonsillar herniation.[5]
Evaluation
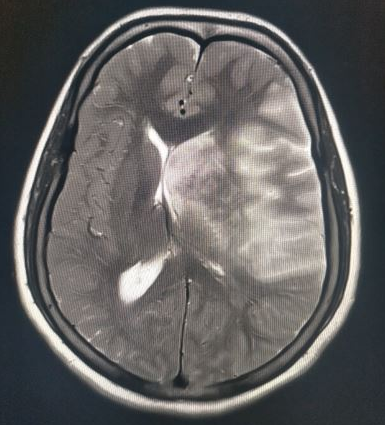
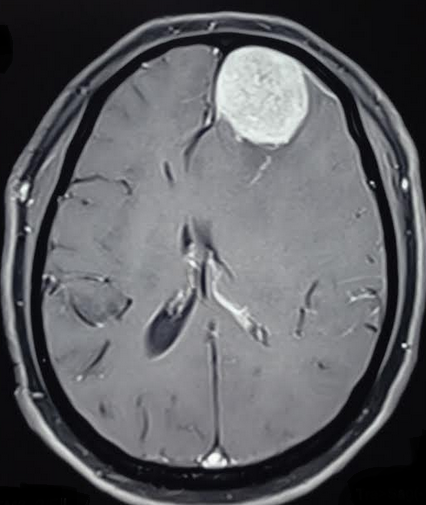
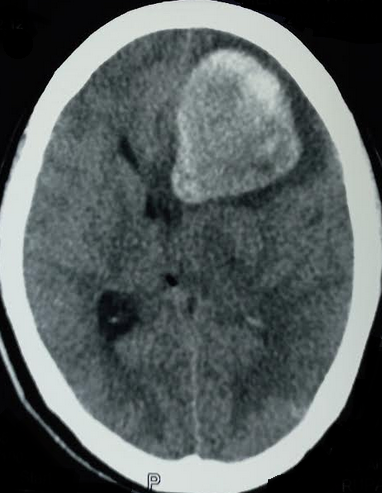
Patients presenting with signs or symptoms of neurologic deterioration require a thorough history taking and physical examination. The history may raise suspicion of intracranial lesions that might lead to neurological deficits. A head computed tomography (CT) scan is the preferred imaging study in TBI. If there is a suspicion of a brain tumor, magnetic resonance imaging (MRI) with and without contrast enhancement is preferred as it shows the lesion with better anatomic and spatial details and can also exclude other non-tumoral etiologies. All patients with neurological deficits require frequent re-evaluation. If any significant findings raise the suspicion of intracranial herniation, a non-contrast CT brain scan should be ordered immediately. The CT scan detects acute hemorrhagic lesions and subtle concurrent midline shifts. It is readily available in most trauma centers and provides rapid results which help improve patient prognosis and clinical outcome.[15][16]
MRI is not always available, and imagings take significantly longer than CT scans. While CT scans are the gold standard for immediate neuroimaging and evaluation for herniation syndromes, other assessment methods such as non-invasive ICP monitoring and transcranial Doppler ultrasonography have the advantage of bedside evaluation of probable herniation, exposing patients to fewer risks of radiation hazards.[17]
Treatment / Management
Management of herniation syndromes depends on etiology, but the prime intention focuses on supporting the patient's respiratory and cardiovascular systems while attempting to decrease the intracranial pressure. Patients presenting with evidence of herniation are treated using a tiered emergency neurological life support (ENLS) management protocol.[5] If one tier does not arrest or reverse the herniation, progression to the next tiers is done sequentially. During such strategies, it is crucial to identify and treat the primary cause. Neurologic resuscitation often requires patience. If resuscitation is successful, clinical and radiological improvement will be noted. When resuscitation is less successful, more invasive and multimodal therapies are available, including ventriculostomy, removing space-occupying lesions (hemorrhages, tumors, abscesses), and decompressive craniectomy. Guidelines for managing severe TBI were published in 2017 by the brain trauma foundation to address treatment interventions, monitoring, and treatment thresholds.[18]
Medical Management
- The head of the bed should be elevated to more than 30 degrees
- Corticosteroid therapy only for tumors
- Hyperosmolar therapy with hypertonic saline or mannitol - Hypertonic saline is available in concentrations from 2 to 23.4% and can be administered as a bolus with set serum sodium goals; serum sodium level is checked every 4 to 6 hours. Mannitol is administered as a 0.5 to 1 g/kg intravenous bolus and may be repeated every 4 to 6 hours with concurrent monitoring of the serum osmolality.
- Sedation with propofol
- Hypothermia
- Pentobarbital for electroencephalographic burst suppression
- Hyperventilation in the early acute phase before a definite treatment is performed
- Seizure prophylaxis
Surgical Management
- ICP monitoring
- External ventricular drain to measure ICP and to drain CSF
- Craniotomy to remove a hematoma or brain mass
- Decompressive craniectomy
Differential Diagnosis
Subfalcine herniation does not have a differential diagnosis, but the primary lesion causing the herniation needs to be differentiated. In the absence of trauma, the following etiologies should be excluded:
- Tumor
- Stroke
- Infection
- Edema
- Radiation necrosis
- Hydrocephalus
Prognosis
Prognosis depends on the cause of the herniation, the level of elevation in the intracranial pressure, the presence and duration of resultant cerebral ischemia, and the intracranial structures affected. While some patients make a full recovery, many are left with temporary as well as permanent neurological deficits and disabilities. Reports suggest mortality rates as high as 33% in children with severe nonpenetrating traumatic brain injuries and 60% among patients developing transtentorial herniation.[19][20] It has been reported that 17% of TBI patients have poor clinical outcomes with moderate to severe disability or persistent coma.[21]
Overall, morbidity and mortality rates from traumatic brain injury have decreased in recent years. A 2017 CDC surveillance report noted that 73% of patients discharged following traumatic brain injury had a good functional recovery.[9]
Complications
The primary complication of subfalcine herniation is the compromise of the blood flow through the anterior cerebral artery, resulting in ischemia in the frontal and parietal lobes. This ischemia and the progressing cerebral herniation will eventually lead to decreased consciousness, hemiparesis, respiratory difficulty, coma, and death. Seizures may result from ischemic tissue.
Deterrence and Patient Education
Brain herniation can cause severe clinical disability or death. In some cases of subfalcine herniation, the patients are alert and can make their own decisions. Brain herniation is potentially reversible with appropriate and timely therapeutic interventions. The family members and the relatives should be thoroughly counseled about the patient's herniation syndrome and possible treatment protocols to help in shared decision-making. A timely diagnosis and management will ultimately benefit the patient and improve the clinical outcome.
Pearls and Other Issues
- Subfalcine herniation is noted in many conditions that cause an increase in one of the three integral compartments within the skull:
- Increased brain volume due to tumor, hemorrhage, or edema
- Increased cerebral spinal fluid volume due to hydrocephalus
- Increased blood volume due to increased cerebral blood flow
- Subfalcine herniation may present with very subtle clinical signs and symptoms.
- Subtle clinical changes in patients with subfalcine herniation must be taken seriously to prevent significant morbidity and mortality.
- Subfalcine herniation can progress to uncal or central herniation syndromes.
- Subfalcine herniation can be identified by stringent clinical monitoring and neuroimaging.
Enhancing Healthcare Team Outcomes
Patients with subfalcine herniation frequently require neurosurgical consultation and monitoring by critical care clinicians (MDs, DOs, NPs, PAs) in a medical or neurological intensive care unit. The interprofessional team should be prepared to intervene timely to prevent progressive herniation and neurological deterioration in the patient. Because initial symptoms of subfalcine herniation may be subtle before sudden clinical deterioration, the interprofessional healthcare team must maintain open and clear lines of communication. Nursing staff should thoroughly examine the patient for any clinical deterioration and immediately contact the physician responsible for the patient’s care. A thorough evaluation by the clinician must follow, and pertinent imaging studies should be ordered immediately. If subfalcine herniation is detected, the team should immediately start the treatment algorithm to stabilize the airway, maintain adequate cerebral perfusion, and halt or reverse the herniation syndrome.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001 Jun 26:56(12):1746-8 [PubMed PMID: 11425944]
Schimpf MM. Diagnosing increased intracranial pressure. Journal of trauma nursing : the official journal of the Society of Trauma Nurses. 2012 Jul-Sep:19(3):160-7. doi: 10.1097/JTN.0b013e318261cfb4. Epub [PubMed PMID: 22955712]
Myers KA, McMahon JM, Mandelstam SA, Mackay MT, Kalnins RM, Leventer RJ, Scheffer IE. Fatal Cerebral Edema With Status Epilepticus in Children With Dravet Syndrome: Report of 5 Cases. Pediatrics. 2017 Apr:139(4):. pii: e20161933. doi: 10.1542/peds.2016-1933. Epub 2017 Mar 22 [PubMed PMID: 28330972]
Level 3 (low-level) evidenceSterns RH, Silver SM. Complications and management of hyponatremia. Current opinion in nephrology and hypertension. 2016 Mar:25(2):114-9. doi: 10.1097/MNH.0000000000000200. Epub [PubMed PMID: 26735146]
Level 3 (low-level) evidenceStevens RD, Shoykhet M, Cadena R. Emergency Neurological Life Support: Intracranial Hypertension and Herniation. Neurocritical care. 2015 Dec:23 Suppl 2(Suppl 2):S76-82. doi: 10.1007/s12028-015-0168-z. Epub [PubMed PMID: 26438459]
Bjerring PN, Eefsen M, Hansen BA, Larsen FS. The brain in acute liver failure. A tortuous path from hyperammonemia to cerebral edema. Metabolic brain disease. 2009 Mar:24(1):5-14. doi: 10.1007/s11011-008-9116-3. Epub 2008 Dec 3 [PubMed PMID: 19050999]
Level 3 (low-level) evidenceShah A, Choi D. Subfalcine herniation in the absence of a high pressure collection or mass: 'brain-slump'? British journal of neurosurgery. 2004 Jun:18(3):273-4 [PubMed PMID: 15327230]
Level 3 (low-level) evidenceCoronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD, Guzman BR, Hemphill JD, Centers for Disease Control and Prevention (CDC). Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002). 2011 May 6:60(5):1-32 [PubMed PMID: 21544045]
Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002). 2017 Mar 17:66(9):1-16. doi: 10.15585/mmwr.ss6609a1. Epub 2017 Mar 17 [PubMed PMID: 28301451]
Earley CJ, Kittner SJ, Feeser BR, Gardner J, Epstein A, Wozniak MA, Wityk R, Stern BJ, Price TR, Macko RF, Johnson C, Sloan MA, Buchholz D. Stroke in children and sickle-cell disease: Baltimore-Washington Cooperative Young Stroke Study. Neurology. 1998 Jul:51(1):169-76 [PubMed PMID: 9674798]
Avery RA, Shah SS, Licht DJ, Seiden JA, Huh JW, Boswinkel J, Ruppe MD, Chew A, Mistry RD, Liu GT. Reference range for cerebrospinal fluid opening pressure in children. The New England journal of medicine. 2010 Aug 26:363(9):891-3. doi: 10.1056/NEJMc1004957. Epub [PubMed PMID: 20818852]
Level 3 (low-level) evidenceAvery RA. Interpretation of lumbar puncture opening pressure measurements in children. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2014 Sep:34(3):284-7. doi: 10.1097/WNO.0000000000000154. Epub [PubMed PMID: 25133882]
Level 3 (low-level) evidenceAndrews BT, Chiles BW 3rd, Olsen WL, Pitts LH. The effect of intracerebral hematoma location on the risk of brain-stem compression and on clinical outcome. Journal of neurosurgery. 1988 Oct:69(4):518-22 [PubMed PMID: 3418383]
Level 2 (mid-level) evidenceJang SH, Kim SH, Chang MC. Injury of the Arcuate Fasciculus in the Nondominant Hemisphere by Subfalcine Herniation in Patients with Intracerebral Hemorrhage : Two Case Reports and Literature Review. Journal of Korean Neurosurgical Society. 2016 May:59(3):306-9. doi: 10.3340/jkns.2016.59.3.306. Epub 2016 May 10 [PubMed PMID: 27226866]
Level 3 (low-level) evidenceMarshall LF, Marshall SB, Klauber MR, Van Berkum Clark M, Eisenberg H, Jane JA, Luerssen TG, Marmarou A, Foulkes MA. The diagnosis of head injury requires a classification based on computed axial tomography. Journal of neurotrauma. 1992 Mar:9 Suppl 1():S287-92 [PubMed PMID: 1588618]
Maas AI, Hukkelhoven CW, Marshall LF, Steyerberg EW. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005 Dec:57(6):1173-82; discussion 1173-82 [PubMed PMID: 16331165]
Cardim D, Robba C, Bohdanowicz M, Donnelly J, Cabella B, Liu X, Cabeleira M, Smielewski P, Schmidt B, Czosnyka M. Non-invasive Monitoring of Intracranial Pressure Using Transcranial Doppler Ultrasonography: Is It Possible? Neurocritical care. 2016 Dec:25(3):473-491 [PubMed PMID: 26940914]
Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Ghajar J. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. 2017 Jan 1:80(1):6-15. doi: 10.1227/NEU.0000000000001432. Epub [PubMed PMID: 27654000]
Michaud LJ, Rivara FP, Grady MS, Reay DT. Predictors of survival and severity of disability after severe brain injury in children. Neurosurgery. 1992 Aug:31(2):254-64 [PubMed PMID: 1513431]
Andrews BT, Pitts LH. Functional recovery after traumatic transtentorial herniation. Neurosurgery. 1991 Aug:29(2):227-31 [PubMed PMID: 1886660]
Langlois JA, Kegler SR, Butler JA, Gotsch KE, Johnson RL, Reichard AA, Webb KW, Coronado VG, Selassie AW, Thurman DJ. Traumatic brain injury-related hospital discharges. Results from a 14-state surveillance system, 1997. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002). 2003 Jun 27:52(4):1-20 [PubMed PMID: 12836629]