Introduction
Superior vena cava (SVC) syndrome is a collection of clinical signs and symptoms resulting from partial or complete obstruction of blood flow through the SVC. This obstruction is most commonly a result of thrombus formation or tumor infiltration of the vessel wall. The SVC is formed by the junction of the left and right innominate (brachiocephalic) veins and is tasked with returning blood from the head, neck, upper extremities, and torso back to the heart (see Image. Veins and Arteries of the Neck). Today, this syndrƒome is most commonly seen secondary to malignancy, although there has been a recent rise in benign etiologies. The resulting venous congestion produces a clinical scenario of increased upper-body venous pressure. The most common signs and symptoms include face or neck swelling, upper extremity swelling, dyspnea, cough, and dilated chest vein collaterals.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
SVC syndrome saw a dramatic decrease throughout the twentieth century. Today, the majority of SVC syndromes are the result of mediastinal malignancies, primarily among which are small-cell bronchogenic carcinoma. The second most commonly associated malignancy is non-Hodgkins lymphoma, followed by metastatic tumors. In addition, benign or nonmalignant causes of SVC syndrome now comprise at least 40% of cases. Iatrogenic thrombus formation or SVC stenosis is a growing etiology due to pacemaker wires and semipermanent intravascular catheters used for hemodialysis, long-term antibiotics, or chemotherapy.[4][5]
Epidemiology
An estimated 15,000 cases of SVC syndrome occur each year in the United States, with studies pointing to increasing frequency due to the concomitant rise in the use of semipermanent intravascular catheters. The incidence of SVC syndrome reported in the literature ranges from 1 in 650 to 1 in 3100 patients.
Pathophysiology
The SVC is part of the low-pressure venous system containing thin walls susceptible to damage by various pathologic mechanisms. These mechanisms can be divided into 3 categories: compromised vessel anatomy, impaired venous flow, and diminished vessel wall integrity. These mechanisms often coexist in patients presenting with SVC syndrome. Extrinsic compression and obstruction of the SVC by a mass in the mediastinum is the most common cause of SVC syndrome. This is often associated with malignancy; however, a variety of nonmalignant masses and dilation of the overlying aorta can cause compression. A growing proportion of SVC syndromes are now associated with occlusive venous thrombus formation that compromises venous flow back to the heart. The increasing use of indwelling intravascular devices such as catheters, pacemakers, and implantable cardioverter-defibrillator (ICD) leads to this growth. Resultant venous wall inflammation, fibrosis, and eventual thrombus lead to vessel stenosis.[6][7][8]
History and Physical
SVC syndrome diagnosis is largely based on a patient’s history and physical findings, which often develop over days to weeks. This insidious onset results from a collateral vascular network that diverts blood to the lower body, where it is then returned to the heart through the inferior vena cava, azygos vein, and intercostals. The clinical findings in SVC syndrome are closely linked to venous congestion and the resultant elevation in venous pressures seen in the upper body. A careful physical examination is often sufficient to rule out a cardiogenic origin of the patient’s symptoms. The most common presenting symptoms of SVC syndrome are face/neck swelling, distended neck veins, cough, dyspnea, orthopnea, upper extremity swelling, distended chest vein collaterals, and conjunctival suffusion. Other less common symptoms of SVC syndrome include stridor, hoarseness, dysphagia, pleural effusion, head plethora, headache, nausea, lightheadedness, syncope, change in vision, altered mental status, upper body edema, cyanosis, papilledema, stupor, and coma. Some rare but serious clinical consequences reported in SVC syndrome include cerebral edema and upper respiratory compromise secondary to edema of the larynx and pharynx.
Evaluation
Patients with high clinical suspicion for SVC syndrome should undergo imaging of the upper body and vasculature. Ultrasound of the jugular, subclavian, and innominate veins can help to identify a thrombus within the vessel lumen. Radiographic imaging and MRI also play a critical role in providing additional information about the SVC obstruction's location, severity, and etiology. CT of the chest with collateral vessels is associated with a diagnostic sensitivity of 96% and a specificity of 92%. Venography is widely accepted as the gold standard for visualizing and diagnosing a venous obstruction. This modality should be used concomitantly with endovascular intervention for patients with a severe presentation of SVC syndrome.[9][10]
Treatment / Management
Following a clinical diagnosis, supportive therapy and medical management are commonly initiated. This involves elevating the patient’s head as a simple maneuver to decrease venous pressure. Further management is guided by the patient’s underlying SVC syndrome etiology. For patients with thrombus related to an indwelling intravascular device, removal should be considered along with anticoagulation therapy and catheter-directed thrombolysis. Multidisciplinary treatment planning for those with obstruction due to malignancy is important as tumor type and staging can help to guide appropriate chemotherapy or radiation therapy. Open surgical repair through bypass grafting with spiral saphenous vein, femoral vein, polytetrafluoroethylene (PTFE) graft, or Dacron graft has traditionally been considered to overcome SVC obstruction. However, this is now reserved for cases where recanalization through endovascular repair is either impossible or has previously failed. With expanding treatment options for both benign and malignant etiology, endovascular therapy is now widely considered the first-line treatment for SVC syndrome. Less invasive endovascular management can offer patients immediate relief of symptoms. Acute or subacute thrombus can be managed with catheter-based thrombolysis or thrombectomy before venoplasty and stent placement.[11][12][13](A1)
Differential Diagnosis
The differential diagnosis for superior vena cava syndrome includes the following:
- Cardiac tamponade
- Mediastinitis
- Thoracic aortic aneurysm
- Tuberculosis
Pearls and Other Issues
A widely accepted and standardized set of criteria outlining presentation severity does not exist for SVC syndrome. The Kishi Scoring System for Signs and Symptoms of SVC syndrome grades severity based on the patient’s clinical presentation. This scoring system includes the patient’s neurologic symptoms, laryngopharyngeal or thoracic symptoms, nasal and facial signs or symptoms, and the presence of venous dilatation.
Enhancing Healthcare Team Outcomes
Because there are many causes of SVCS, the condition is best managed by an interprofessional team of healthcare workers, including a vascular surgeon, interventional radiologist, radiation therapist, oncologist, pain specialist, and cardiac surgeon. The nurse plays a vital role in the monitoring of these patients. Many of them have cerebral and laryngeal edema and need close monitoring. The pharmacist should be fully aware of the drugs used to manage SVCS, which include corticosteroids and diuretics. Because many of these patients have an unpredictable course, radiation is often administered as a palliative measure to shrink the tumor and relieve the symptoms. Patients with Hodgkin lymphoma are managed with chemotherapy.[14][15]
Outcomes
The prognosis of patients with SVCS depends on the cause. For patients with a benign cause of SVCS, the life expectancy is not changed, but for malignant cases, there is a significant drop in survival. Individuals who have features of cerebral and laryngeal edema can develop life-threatening symptoms and suddenly die. Patients with SVCS as a result of lung cancer usually live less than 24 months. For those who do not respond to radiation treatment, the survival is less than a year.[16][17][18]
Media
(Click Image to Enlarge)
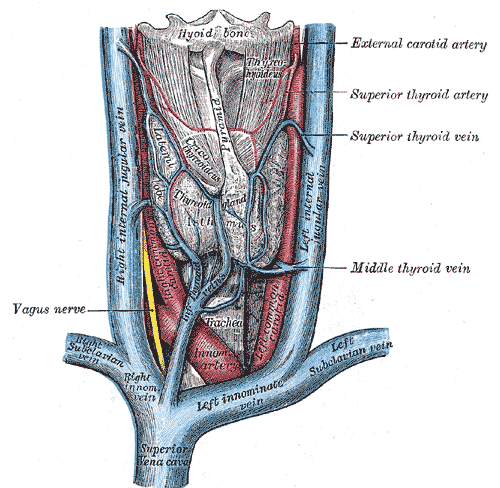
Veins and Arteries of the Neck. Superior vena cava, left and right innominate vein, left and right subclavian vein, left and right internal jugular vein, innominate arteries, hyoid bone, thyroid gland, and trachea.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Drouin L, Pistorius MA, Lafforgue A, N'Gohou C, Richard A, Connault J, Espitia O. [Upper-extremity venous thrombosis: A retrospective study about 160 cases]. La Revue de medecine interne. 2019 Jan:40(1):9-15. doi: 10.1016/j.revmed.2018.07.012. Epub 2018 Aug 16 [PubMed PMID: 30122260]
Level 2 (mid-level) evidenceZimmerman S, Davis M. Rapid Fire: Superior Vena Cava Syndrome. Emergency medicine clinics of North America. 2018 Aug:36(3):577-584. doi: 10.1016/j.emc.2018.04.011. Epub 2018 Jun 12 [PubMed PMID: 30037444]
Carmo J, Santos A. Chronic Occlusion of the Superior Vena Cava. The New England journal of medicine. 2018 Jul 5:379(1):e2. doi: 10.1056/NEJMicm1711273. Epub [PubMed PMID: 29972752]
De Potter B,Huyskens J,Hiddinga B,Spinhoven M,Janssens A,van Meerbeeck JP,Parizel PM,Snoeckx A, Imaging of urgencies and emergencies in the lung cancer patient. Insights into imaging. 2018 Aug [PubMed PMID: 29644546]
Friedman T, Quencer KB, Kishore SA, Winokur RS, Madoff DC. Malignant Venous Obstruction: Superior Vena Cava Syndrome and Beyond. Seminars in interventional radiology. 2017 Dec:34(4):398-408. doi: 10.1055/s-0037-1608863. Epub 2017 Dec 14 [PubMed PMID: 29249864]
Kalinin RE, Suchkov IA, Shitov II, Mzhavanadze ND, Povarov VO. [Venous thromboembolic complications in patients with cardiovascular implantable electronic devices]. Angiologiia i sosudistaia khirurgiia = Angiology and vascular surgery. 2017:23(4):69-74 [PubMed PMID: 29240058]
Ghorbani H, Vakili Sadeghi M, Hejazian T, Sharbatdaran M. Superior vena cava syndrome as a paraneoplastic manifestation of soft tissue sarcoma. Hematology, transfusion and cell therapy. 2018 Jan-Mar:40(1):75-78. doi: 10.1016/j.htct.2017.09.001. Epub 2018 Feb 17 [PubMed PMID: 30057975]
Labriola L, Seront B, Crott R, Borceux P, Hammer F, Jadoul M. Superior vena cava stenosis in haemodialysis patients with a tunnelled cuffed catheter: prevalence and risk factors. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2018 Dec 1:33(12):2227-2233. doi: 10.1093/ndt/gfy150. Epub [PubMed PMID: 29893920]
Mansour A, Saadeh SS, Abdel-Razeq N, Khozouz O, Abunasser M, Taqash A. Clinical Course and Complications of Catheter and Non-Catheter-Related Upper Extremity Deep Vein Thrombosis in Patients with Cancer. Clinical and applied thrombosis/hemostasis : official journal of the International Academy of Clinical and Applied Thrombosis/Hemostasis. 2018 Nov:24(8):1234-1240. doi: 10.1177/1076029618788177. Epub 2018 Jul 19 [PubMed PMID: 30025472]
Khan UA, Shanholtz CB, McCurdy MT. Oncologic Mechanical Emergencies. Hematology/oncology clinics of North America. 2017 Dec:31(6):927-940. doi: 10.1016/j.hoc.2017.08.001. Epub [PubMed PMID: 29078930]
Nossair F, Schoettler P, Starr J, Chan AKC, Kirov I, Paes B, Mahajerin A. Pediatric superior vena cava syndrome: An evidence-based systematic review of the literature. Pediatric blood & cancer. 2018 Sep:65(9):e27225. doi: 10.1002/pbc.27225. Epub 2018 May 21 [PubMed PMID: 29781569]
Level 1 (high-level) evidenceIerardi AM, Jannone ML, Petrillo M, Brambillasca PM, Fumarola EM, Angileri SA, Crippa M, Carrafiello G. Treatment of venous stenosis in oncologic patients. Future oncology (London, England). 2018 Dec:14(28):2933-2943. doi: 10.2217/fon-2017-0737. Epub 2018 Apr 6 [PubMed PMID: 29623736]
Kalra M, Sen I, Gloviczki P. Endovenous and Operative Treatment of Superior Vena Cava Syndrome. The Surgical clinics of North America. 2018 Apr:98(2):321-335. doi: 10.1016/j.suc.2017.11.013. Epub [PubMed PMID: 29502774]
Hague J, Tippett R. Endovascular techniques in palliative care. Clinical oncology (Royal College of Radiologists (Great Britain)). 2010 Nov:22(9):771-80. doi: 10.1016/j.clon.2010.08.002. Epub 2010 Sep 15 [PubMed PMID: 20833516]
Gradishar WJ, Magid D, Bitran JD. Supportive care of the lung cancer patients. Hematology/oncology clinics of North America. 1990 Dec:4(6):1183-99 [PubMed PMID: 1704881]
Lianos GD, Hasemaki N, Tzima E, Vangelis G, Tselios A, Mpailis I, Lekkas E. Superior vena cava syndrome due to central port catheter thrombosis: a real life-threatening condition. Il Giornale di chirurgia. 2018 Mar-Apr:39(2):101-106 [PubMed PMID: 29694310]
Kuo TT, Chen PL, Shih CC, Chen IM. Endovascular stenting for end-stage lung cancer patients with superior vena cava syndrome post first-line treatments - A single-center experience and literature review. Journal of the Chinese Medical Association : JCMA. 2017 Aug:80(8):482-486. doi: 10.1016/j.jcma.2017.04.005. Epub 2017 May 10 [PubMed PMID: 28501315]
Nakano T, Endo S, Kanai Y, Otani S, Tsubochi H, Yamamoto S, Tetsuka K. Surgical outcomes after superior vena cava reconstruction with expanded polytetrafluoroethylene grafts. Annals of thoracic and cardiovascular surgery : official journal of the Association of Thoracic and Cardiovascular Surgeons of Asia. 2014:20(4):310-5 [PubMed PMID: 23801179]