Introduction
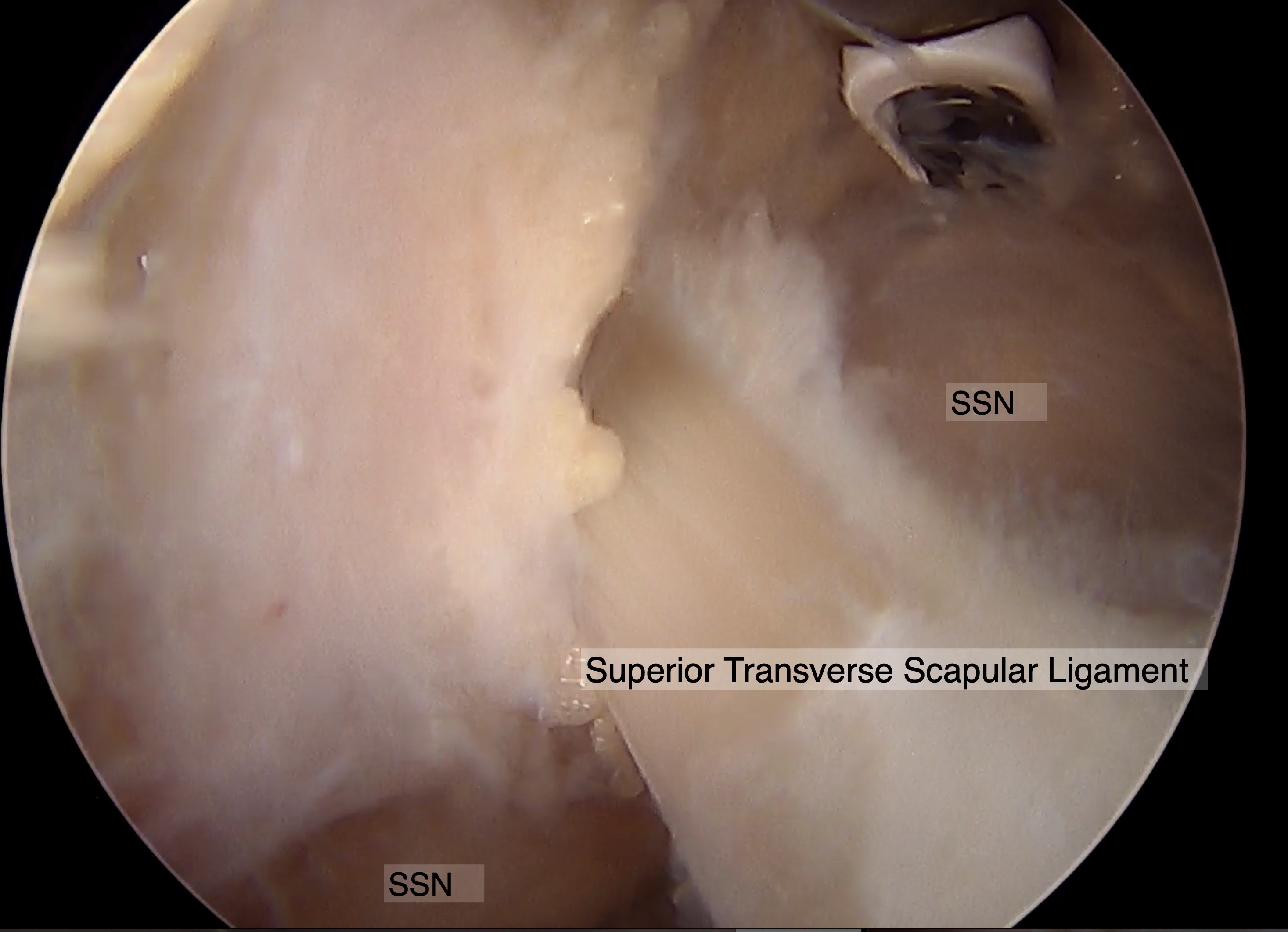
There is an increasing interest in the literature regarding the clinical presentation of suprascapular nerve (SSN) injuries. While the underlying etiology of suprascapular neuropathy remains elusive, multiple compression, traction, and inflammatory pathophysiologic cascades have been previously considered.[1][2][3] The latter are often readily grouped together with other clinical manifestations of SSN dysfunction and inevitably become labeled as idiopathic. The anatomically tortuous course of the SSN predisposes it to direct mechanical compression at the suprascapular and spinoglenoid notches (see Image. Suprascapular Nerve Course, Arthroscopic Image). Moreover, anatomic variations along the nerve's course and occupational or athletic overuse conditions, especially in overhead athletes, can predispose the SSN to varying degrees of dysfunction.[4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
First described in the French literature in 1936 and the English literature in 1959, SSN dysfunction is implicated in approximately 1% to 2% of cases of shoulder pain and up to 33% of cases of shoulder pain in overhead athletes.[6] Causes of SSN injury include primary etiologies that can be attributed to anatomical entrapment of the SSN along the nerve's course or functional impingement of the SSN with repetitive use, as in overhead athletes. Some of the most common anatomic sites of SSN entrapment include:
Other secondary etiologies of SSN dysfunction include, but are not limited to:
- Scapulothoracic dyskinesia, shoulder girdle dysfunction
- Traumatic injuries with SSN injury occurring secondary to the nerve's proximity to the primary injury and associated mechanism of action [9][10]
- Fractures of the scapula, clavicle, proximal humerus
- Glenohumeral dislocations
- Acromioclavicular joint injuries
- Iatrogenic injuries during arthroscopic or open shoulder surgeries [11]
- Space-occupying lesions [12]
- Ganglion cysts
- Paralabral cysts
- Bone cysts
- Osteosarcoma, soft tissue sarcoma, metastatic lesions
- Systemic conditions
Historically a diagnosis of exclusion, SSN dysfunction has become an increasingly recognized clinical condition with an often discrete underlying pathologic process. Moreover, while isolated SSN injuries remain relatively uncommon, this is the most frequently injured peripheral branch of the brachial plexus in athletes.[5]
Primary etiologies of SSN compression and injury include the at-risk anatomic sites along the course of the SSN, in addition to repetitive overhead activities often seen during various sports and manual labor with excessive overhead occupational demands. The former includes throwing athletes and those athletes exposed to repetitive overhead trauma and repetitive motions, such as baseball players, tennis players, weight lifters, swimmers, and volleyball players.[15][16][17][18]
Epidemiology
SSN dysfunction epidemiological data are lacking and often debated given the general heterogeneous reports in the literature, combined with the recent increases and advancements in diagnostic imaging modalities. Moreover, the clinical significance of SSN dysfunction varies from complete irrelevance in asymptomatic patients who can be diagnosed with possible SSN dysfunction incidentally to increasing degrees of shoulder pain and dysfunction related to the supraspinatus or infraspinatus atrophy and degeneration. Thus, incidence and prevalence rates remain elusive.[4]
Estimations have cited suprascapular neuropathy, mechanical irritation during repetitive traction and overhead motions, and focal entrapment to represent anywhere from 0.4% to 2% of cases of shoulder girdle pain. Consensus exists that SSN dysfunction is often seen in association with various sport-specific positions and elite performance levels.
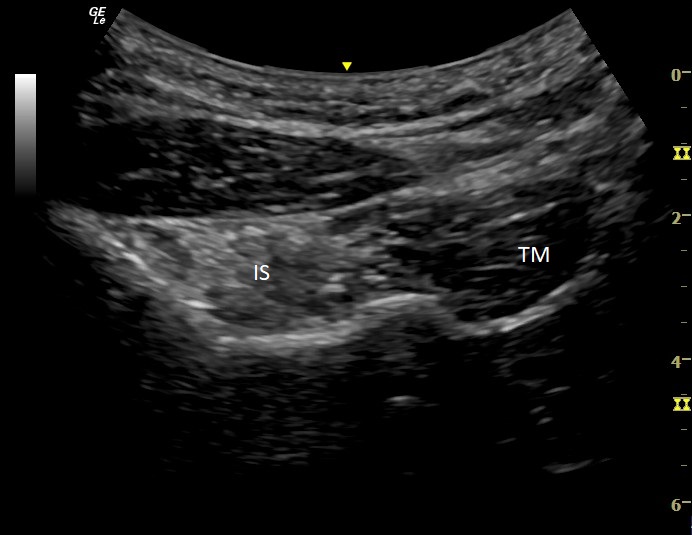
Isolated infraspinatus muscle atrophy (see Images. Infraspinatus Muscle Atrophy, Ultrasound and Supraspinatus Muscle Atrophy, Ultrasound) is often utilized as a sign as it is readily detectable on physical exam or other diagnostic modalities such as ultrasound, electromyographic studies, or magnetic resonance imaging (MRI). While the clinical relevance of isolated infraspinatus atrophy remains unclear, with most patients reporting normal shoulder function and no pain, the associated incidence rates seen in the dominant shoulder of overhead athletes range from 4% to 52%, with the highest rates recently reported in a 2015 study that investigated the incidence seen in elite professional female tennis players.[19] Interestingly, the authors noted that clinically relevant infraspinatus atrophy, as detected on physical examination alone, was associated with a higher performance ranking, and no functional deficits or associations with concurrent shoulder disorders were appreciated.[20][21][22] Even studies from the early 1990s cited a 34% to 45% incidence rate of infraspinatus muscle impairment in baseball pitchers and elite volleyball players.[23][24][25]
Pathophysiology
Muscle wasting, atrophy, and degeneration are thought to occur secondary to either direct mechanical compression from an underlying anatomic variation, space-occupying lesion, or secondary to repetitive traction and irritation of the nerve at one of the anatomically predisposed sites of SSN focal entrapment as described below.
Anatomic Sites of Entrapment
The SSN is derived from the upper trunk of the brachial plexus, consisting of fibers from the C5 and C6 nerve roots.[26] A mixed motor and sensory nerve, the SSN supplies motor innervation to the supraspinatus and infraspinatus muscles in addition to sensory innervation to the coracohumeral and coracoacromial ligaments, subacromial bursa, and the acromioclavicular and glenohumeral joint capsules.[27]
The SSN traverses through the supraclavicular fossa, passing through the posterior triangle of the neck before coursing deep to the trapezius muscle and the clavicle. Continuing laterally toward the suprascapular notch, the SSN is accompanied by its artery and vein. Aiello et al first identified the suprascapular and spinoglenoid notches as 2 potential sites of SSN entrapment secondary to direct mechanical compression.[28] The SSN passes inferior to the superior transverse scapular ligament, a fibrous, banded structure that traverses the superior aspect of the scapula and serves as the superior boundary of the suprascapular notch. Direct compression at the suprascapular notch remains the most common site for SSN entrapment. After traversing the suprascapular notch, the SSN enters the suprascapular fossa before dividing into the supraspinatus and infraspinatus nerve branches.[29] While the nerve exhibits increased mobility within the suprascapular fossa, its range is constrained due to adherence to the periosteum and motor branches directed towards the supraspinatus muscle.[30] Furthermore, space-occupying lesions (eg, ganglion or paralabral cysts) and fracture sequelae (ie, malunion/nonunion) can cause compression and resultant nerve injury. Distally, the SSN turns medially at the spinoglenoid notch and can be at risk of localized compression secondary to paralabral cysts, prominent hardware, and enlarged veins.[31][32] Although overall less common compared to its suprascapular notch counterpart for a focal site of SSN entrapment, the spinoglenoid notch is becoming an increasingly appreciated site of mechanical compression.[33][34][35]
Anatomic Variants
Multiple anatomic variations have been gaining increasing attention in the literature as additional elements predisposing to SSN dysfunction. Much of the attention has focused on variations in the morphology of the suprascapular notch itself, given that it remains the most common site of SSN focal entrapment. Suprascapular neuropathy has been reported in the setting of an ossified STSL, with varying degrees—including the presence of a double suprascapular foramen created by multiple, discrete osseous bridges.[36] The morphological risk factors of the suprascapular notch also include osseous prominences at the margins of the bony incisura, a bifid STSL, and a narrowed “V” shape configuration of the notch itself.[37] The anterior coracoscapular ligament,[38] spinoglenoid ligament (inferior transverse scapular ligament, ITSL), and a hypertrophied subscapularis muscle are other less common anatomic variations reported in the literature.[39][40][41][42]
The ITSL has continued to gain literature support and documented evidence of its physiological existence in most of the population. While historical studies reported the presence of the ITSL in about half of the population, more recent cadaveric specimen dissections identify a discrete, complex ITSL structure in 100% of the dissected specimens. In 2005, Plancher et al identified the spinoglenoid ligament in all cadaveric specimens, with the ligament reproducibly demonstrating an irregular quadrangular shape, thinnest in its midportion and fanning out to its insertions superomedially and inferolaterally. The inferolateral portion of the ligament shows distinct superficial and deep layers inserting into the posterior aspects of both the shoulder capsule and the glenoid neck.[43]
History and Physical
SSN injury is typically related to repetitive overhead activities in athletes (baseball players, tennis players, weight lifters, swimmers, and volleyball players) or laborers. Patients usually present with dull, aching pain in the superior or posterolateral shoulder (or both) that can radiate down the arm or into the neck. Patients may not complain of pain if the injury is distal to the spinoglenoid notch. Additional symptoms include a sense of instability if there is associated shoulder pathology, such as a labral or rotator cuff tear.[30] Symptoms typically develop gradually and intermittently and may worsen over time to the point of being constant. However, results from some studies have reported a traumatic injury as the initial cause in 40% of patients.[44]
Given that the symptoms can overlap with other shoulder pathologies and sometimes present without pain, it is often difficult to diagnose an SSN injury on history alone. A comprehensive physical exam must include a detailed shoulder and cervical spine exam to rule out alternative or comorbid etiologies. One of the most common findings on physical exam is atrophy of either or both of the infraspinatus or supraspinatus muscles, with a meta-analysis finding atrophy in 1 or both muscle groups in nearly 80% of patients with confirmed suprascapular neuropathy.[13]
Patients may endorse tenderness to palpation posterior to the acromioclavicular joint, the posterosuperior joint line, or both. The patient’s pain may be exacerbated by cross-body adduction and internal rotation.[45] Weakness may be noted with either or both shoulder external rotation and abduction. However, if the nerve injury is at or distal to the spinoglenoid notch, and only the infraspinatus is affected, weakness may not be as pronounced given that the patient’s deltoid, supraspinatus, and teres minor can compensate in both functional and strength. A specific physical exam maneuver that has been described to help with the diagnosis is the “SSN stretch test.” This test consists of laterally rotating the patient’s head away from the painful shoulder and retracting the neck and shoulder on the affected side. A test is “positive” when the maneuver provokes pain at the posterior shoulder.[46]
Evaluation
Suprascapular neuropathy is very difficult to diagnose from history and physical examination alone. Further evaluation with imaging and diagnostic testing, including electrodiagnostic testing and nerve blocks, is warranted. Initially, plain radiographs should be obtained to evaluate for possible osseous abnormalities impinging on the nerve or other comorbid shoulder conditions, such as arthritis or evidence of dislocation or subluxation.[30] Radiographs are essential in patients with an acute injury causing pain and weakness, as the clinician will need to rule out a scapular fracture, first rib fracture, acromioclavicular joint disruption, or shoulder dislocation.[47] Shoulder radiographs must include the specialized Stryker notch view to help visualize the suprascapular notch and any associated osseous abnormalities at the foramen.[1] If osseous abnormalities are thought to be the primary cause of injury, a computed tomography scan may help further localize the area of nerve compression.[48]
MRI can be helpful in the evaluation of suprascapular neuropathy, given its ability to assess for indirect signs of SSN injury, such as areas of soft tissue compression, as well as the quality of the rotator cuff musculature revealing areas of muscle atrophy and fatty infiltration.[49] MRI can also help rule out other causes of shoulder pain considered in the differential, such as labral or rotator cuff tears.
Musculoskeletal ultrasound can be particularly useful in diagnosis for visualizing the nerve course and performing a dynamic muscle and nerve exam but also for guidance for an SSN block. The SSN is best visualized with ultrasound during its supraclavicular course when the nerve is most superficial. While the optimal visualization of the nerve is suggested in the coronal plane over the suprascapular fossa between the spinoglenoid and scapular notch, studies demonstrate its accurate tracking along the entire course. This journey spans from its origin at the interscalene triangle, navigating through anatomical landmarks such as the first rib, the lateral supraclavicular fossa beneath the omohyoid muscle, the supraspinatus fossa, and the spinoglenoid notch, concluding in the infraspinatus fossa.[50] Furthermore, ultrasound is superior to MRI for its dynamic visualization of the SSN. A dynamic exam allows the clinician to visualize the nerve traveling through or near the impingement sites. This portion of the exam can show how overhead movements can impact the course of the nerve or how potential pathologic sites can cause nerve compression (eg, paralabral cyst compressing the SSN. And like MRI, ultrasound can evaluate the quality of the rotator cuff musculature again, looking for indirect signs of SSN injury such as muscle atrophy and fatty infiltration. Increased intramuscular fat causes an increase in muscular echogenicity on ultrasound, with further increases depending on muscle diameter and the amount of subcutaneous fat.[51]
Injection of an anesthetic to the suprascapular or spinoglenoid notch with resultant pain relief helps support the diagnosis of suprascapular neuropathy. Using ultrasound to guide the procedure allows for accurate localization and medication delivery, with one study using cadavers showing correct placement achieved 95% of the time (see Video. Suprascapular Nerve Block, Video). Visualization of the needle during the procedure helps to avoid possible complications such as pneumothorax or injury to neighboring vascular structures. Gorthi et al. found that compared to a blind SSN block, ultrasound guidance improved localization and provided significantly longer-lasting relief for patients in one month.[52] In patients with symptoms only present during overhead sport or occupational-specific activities, the authors recommend an ultrasound-guided nerve block with a trial of light sport or occupational-specific activities in a controlled practice environment while in the therapeutic window of the local anesthetic used.
Electrodiagnostic evaluation, including nerve conduction studies and electromyography, is the gold standard for diagnosing and confirming suprascapular neuropathy. This test can specifically focus on the SSN and its innervations. Findings on electrodiagnostic evaluation that suggest compression and denervation of the SSN include prolonged latency, decreased amplitude, fibrillation potentials, and positive sharp waves.[30] Electrodiagnostic evaluation can also ensure the clinician rules out additional etiologies that may mimic suprascapular neuropathy (eg, a cervical (C5-6) radiculopathy or Parsonage-Turner syndrome).
Treatment / Management
Given the difficulty diagnosing suprascapular neuropathy, patients may present after months of dealing with persistent pain and weakness without an identified cause or, alternately, after failing to improve with treatment of comorbid findings on exam or imaging (eg, rotator cuff strains, osteoarthritis, and labral pathology). However, once a diagnosis of SSN injury is confirmed, effective treatment can start.
Nonoperative management can be effective for patients who have isolated suprascapular neuropathy without comorbid pathology such as intra-articular shoulder or rotator cuff pathology.[44] Results from most studies show that patients benefit in 6 to 12 months with conservative management.[53] The conservative treatment approach entails non-steroidal anti-inflammatory medications, activity modification, physical therapy, and ultrasound-guided injections. Specifically for overhead athletes, given the suspected cause being repetitive microtrauma, sport-specific activity modification is key to the initial management of the nerve injury. Physical therapy exercises should emphasize maintaining a full range of motion to prevent the development of adhesive capsulitis. Exercises should focus on stretching the posterior shoulder capsule and strengthening the rotator cuff and surrounding shoulder musculature. Stretching the posterior capsule is especially important in athletes, as this is hypothesized to reduce tension on the spinoglenoid ligament--which can minimize repetitive microtrauma during sports activities. Although physical therapy is beneficial for patients with SSN injury, there is no definitive treatment protocol. An ultrasound-guided injection at the site of suspected entrapment (the superior boundary of the suprascapular notch where the SSN passes inferior to the STSL can help with diagnostic confirmation as well as therapeutic relief. (B2)
There has been growing evidence for using peripheral nerve stimulation devices primarily for patients with shoulder pain but no known compression at a specific anatomical site. These temporarily percutaneously implanted devices target the SSN as it travels through the suprascapular notch. Studies showed significant relief in shoulder pain after removal of the leads, with results from one study finding 85% of patients reporting substantial pain relief or significant improvement in quality of life, or both.[54](B2)
Surgical intervention is warranted if there is an identified pathology causing compression of the nerve or symptoms have not improved despite 6 to 12 months of conservative management. Some surgeons contend that surgical intervention should be performed immediately upon diagnosis because patients likely have had the symptoms for at least 6 months before the presentation.[55][56] Surgical management options depend on the cause and suspected location of the nerve injury. However, the exact surgical option varies, with some authors reporting improvement with the isolated repair of the shoulder pathology without decompression. In contrast, others state decompression of the nerve should occur simultaneously.[57][58][59] If the nerve injury is due to a paralabral cyst, a percutaneous cyst decompression under imaging guidance can be an effective treatment. However, failure rates have been reported up to 50%, given the inability to correct the contributing intra-articular lesions using this technique.[60][61] Postoperatively, most patients had a resolution of pain and improved muscle strength.[62](B2)
Differential Diagnosis
The diagnosis of SSN injury can be challenging given the overlap in presentation with other pathologies of the shoulder and cervical spine region. The differential diagnosis includes, but is not limited to:
- Cervical radiculopathy (C5-6)
- Parsonage-Turner syndrome
- Brachial plexopathy (upper trunk)
- Rotator cuff pathology (eg, tendinitis, bursitis, partial or complete strain or tear)
- Subacromial impingement syndrome
- Scapular dyskinesia
- Labral pathology (eg, superior labral tear from anterior to posterior [SLAP tear])
- Adhesive capsulitis
- Glenohumeral arthritis
- Facet mediated pain [30]
Prognosis
The prognosis for isolated suprascapular neuropathy is generally favorable, with one study’s results reporting 80% of patients having good or excellent improvement in pain and function. Even though most patients with suprascapular neuropathy will experience an improvement in pain and function, whether treated surgically or conservatively, once significant atrophy has occurred, it is unlikely that muscle bulk or strength will return to post-injury levels.[55] However, even with persistent atrophy, most patients will see improvement in supraspinatus and infraspinatus strength, with supraspinatus strength showing greater improvement.[62]
Complications
Pain and weakness have been shown to improve with both conservative management as well as surgical decompression of the nerve as clinically indicated. However, depending on the chronicity of symptoms, the patient may have persistent atrophy and weakness of the supraspinatus and infraspinatus muscles, which the SSN innervates. However, as mentioned previously, the deltoid, supraspinatus, and teres minor can compensate for the loss of infraspinatus strength.[63]
Consultations
Given the difficulty and typical delay in diagnosis, a referral to a physical medicine and rehabilitation physician, sports medicine physician, or orthopedic surgeon is warranted for continued workup and management.
Deterrence and Patient Education
The most important aspect of this condition is initial recognition or diagnosis. Educating patients to seek clinical evaluation without delay is imperative. When discussing treatment options, clinicians should address the patient’s understanding and set realistic expectations for improvement of muscle strength and function, as well as the expected timeline, and be prepared to answer questions regarding prognosis.
Pearls and Other Issues
Other important facets surrounding suprascapular joint nerve injury include:
- The 2 main sites of SSN compression are the suprascapular notch and the spinoglenoid notch.
- The compression of the SSN at the spinoglenoid notch likely will result in isolated infraspinatus atrophy and is painless.
- Diagnosis of suprascapular neuropathy may be delayed due to comorbid but asymptomatic findings of the rotator cuff and labral pathology on examination, imaging, or both.
- The authors recommend electrodiagnostic testing to confirm suprascapular neuropathy and avoid the pitfall of misdiagnosis as Parsonage-Turner Syndrome or cervical radiculopathy.
- In patients with symptoms only present during overhead sport or occupational-specific activities, the authors recommend an ultrasound-guided nerve block with a trial of light sport or occupational-specific activities in a controlled practice environment while still in the therapeutic window of the local anesthetic.
- Prompt diagnosis and treatment are keys to symptom improvement and the potential return to a prior level of function. Once significant atrophy has occurred, it is less likely for the patient to return to pre-morbid muscle bulk and strength in the affected muscles.
Enhancing Healthcare Team Outcomes
SSN injury is a diagnosis that requires a keen diagnostic acumen and an effective multidisciplinary team to manage successfully. Early identification and initiation of treatment are key to symptom improvement and return to the prior level of function. Efficient consultation with specialty providers, such as physical medicine and rehabilitation, sports medicine, or orthopedic surgery, provides the best prognosis and outcome for the patient. Once diagnosed, prompt referral to physical therapy to begin focused rehabilitation is also beneficial for patients to increase their range of motion and strengthen the rotator cuff and surrounding musculature—whether it is the definitive treatment or, ultimately, part of a presurgical and postoperative rehabilitation protocol.
Referrals should include a summary of the history of present illness, physical exam findings, a detailed social history (with close attention to occupations, hobbies, and sports with repetitive overhead motions), the patient’s goals of treatment, and interventions already trialed. This information sharing allows for a more complete view of the patient’s condition and enables all team members access to important information necessary to treat and meet their goals effectively.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Video to Play)
Suprascapular Nerve Block, Video. Ultrasound-guided suprascapular nerve block at the level of the suprascapular notch.
Contributed by Eric Helm, MD
(Click Image to Enlarge)
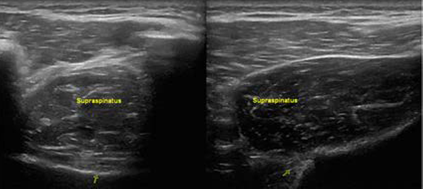
Supraspinatus Muscle Atrophy, Ultrasound. Images of the supraspinatus muscle in short axis. The left image shows evidence of atrophy compared to the right image, which shows normal supraspinatus muscle.
Peck E, Strakowski JA. Ultrasound evaluation of focal neuropathies in athletes: a clinically focused review. Br J Sports Med. 2015;49(3):166-175. doi: 10.1136/bjsports-2014-094268.
References
Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. The Journal of bone and joint surgery. American volume. 2010 Oct 6:92(13):2348-64. doi: 10.2106/JBJS.I.01743. Epub [PubMed PMID: 20926731]
Le Hanneur M, Maldonado AA, Howe BM, Mauermann ML, Spinner RJ. "Isolated" Suprascapular Neuropathy: Compression, Traction, or Inflammation? Neurosurgery. 2019 Feb 1:84(2):404-412. doi: 10.1093/neuros/nyy050. Epub [PubMed PMID: 29529303]
Albritton MJ, Graham RD, Richards RS 2nd, Basamania CJ. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. Journal of shoulder and elbow surgery. 2003 Sep-Oct:12(5):497-500 [PubMed PMID: 14564276]
Kostretzis L, Theodoroudis I, Boutsiadis A, Papadakis N, Papadopoulos P. Suprascapular Nerve Pathology: A Review of the Literature. The open orthopaedics journal. 2017:11():140-153. doi: 10.2174/1874325001711010140. Epub 2017 Feb 28 [PubMed PMID: 28400882]
Safran MR. Nerve injury about the shoulder in athletes, part 1: suprascapular nerve and axillary nerve. The American journal of sports medicine. 2004 Apr-May:32(3):803-19 [PubMed PMID: 15090401]
THOMPSON WA, KOPELL HP. Peripheral entrapment neuropathies of the upper extremity. The New England journal of medicine. 1959 Jun 18:260(25):1261-5 [PubMed PMID: 13666948]
Clavert P, Thomazeau H. Peri-articular suprascapular neuropathy. Orthopaedics & traumatology, surgery & research : OTSR. 2014 Dec:100(8 Suppl):S409-11. doi: 10.1016/j.otsr.2014.10.002. Epub 2014 Oct 25 [PubMed PMID: 25454727]
Gosk J, Urban M, Rutowski R. Entrapment of the suprascapular nerve: anatomy, etiology, diagnosis, treatment. Ortopedia, traumatologia, rehabilitacja. 2007 Jan-Feb:9(1):68-74 [PubMed PMID: 17514177]
Zoltan JD. Injury to the suprascapular nerve associated with anterior dislocation of the shoulder: case report and review of the literature. The Journal of trauma. 1979 Mar:19(3):203-6 [PubMed PMID: 458888]
Level 3 (low-level) evidenceSolheim LF, Roaas A. Compression of the suprascapular nerve after fracture of the scapular notch. Acta orthopaedica Scandinavica. 1978 Aug:49(4):338-40 [PubMed PMID: 696273]
Level 3 (low-level) evidenceMallon WJ, Bronec PR, Spinner RJ, Levin LS. Suprascapular neuropathy after distal clavicle excision. Clinical orthopaedics and related research. 1996 Aug:(329):207-11 [PubMed PMID: 8769453]
Level 3 (low-level) evidenceSjödén GO, Movin T, Güntner P, Ingelman-Sundberg H. Spinoglenoid bone cyst causing suprascapular nerve compression. Journal of shoulder and elbow surgery. 1996 Mar-Apr:5(2 Pt 1):147-9 [PubMed PMID: 8742879]
Level 3 (low-level) evidenceZehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. International orthopaedics. 2002:26(6):339-43 [PubMed PMID: 12466865]
Level 1 (high-level) evidenceJustiz Vaillant AA, Goyal A, Varacallo M. Systemic Lupus Erythematosus. StatPearls. 2024 Jan:(): [PubMed PMID: 30571026]
Agre JC, Ash N, Cameron MC, House J. Suprascapular neuropathy after intensive progressive resistive exercise: case report. Archives of physical medicine and rehabilitation. 1987 Apr:68(4):236-8 [PubMed PMID: 3566518]
Level 3 (low-level) evidenceHoyt WA Jr. Etiology of shoulder injuries in athletes. The Journal of bone and joint surgery. American volume. 1967 Jun:49(4):755-66 [PubMed PMID: 6026009]
Yoon TN, Grabois M, Guillen M. Suprascapular nerve injury following trauma to the shoulder. The Journal of trauma. 1981 Aug:21(8):652-5 [PubMed PMID: 7265337]
Level 3 (low-level) evidenceSandow MJ, Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. Journal of shoulder and elbow surgery. 1998 Sep-Oct:7(5):516-21 [PubMed PMID: 9814933]
Cummins CA, Messer TM, Schafer MF. Infraspinatus muscle atrophy in professional baseball players. The American journal of sports medicine. 2004 Jan-Feb:32(1):116-20 [PubMed PMID: 14754733]
Level 2 (mid-level) evidenceYoung SW, Dakic J, Stroia K, Nguyen ML, Harris AH, Safran MR. High Incidence of Infraspinatus Muscle Atrophy in Elite Professional Female Tennis Players. The American journal of sports medicine. 2015 Aug:43(8):1989-93. doi: 10.1177/0363546515588177. Epub 2015 Jun 15 [PubMed PMID: 26078449]
Lajtai G, Wieser K, Ofner M, Raimann G, Aitzetmüller G, Jost B. Electromyography and nerve conduction velocity for the evaluation of the infraspinatus muscle and the suprascapular nerve in professional beach volleyball players. The American journal of sports medicine. 2012 Oct:40(10):2303-8 [PubMed PMID: 22875791]
Level 2 (mid-level) evidenceLajtai G, Pfirrmann CW, Aitzetmüller G, Pirkl C, Gerber C, Jost B. The shoulders of professional beach volleyball players: high prevalence of infraspinatus muscle atrophy. The American journal of sports medicine. 2009 Jul:37(7):1375-83. doi: 10.1177/0363546509333850. Epub 2009 Apr 9 [PubMed PMID: 19359418]
Level 2 (mid-level) evidenceEggert S, Holzgraefe M. [Compression neuropathy of the suprascapular nerve in high performance volleyball players]. Sportverletzung Sportschaden : Organ der Gesellschaft fur Orthopadisch-Traumatologische Sportmedizin. 1993 Sep:7(3):136-42 [PubMed PMID: 8273015]
Holzgraefe M, Kukowski B, Eggert S. Prevalence of latent and manifest suprascapular neuropathy in high-performance volleyball players. British journal of sports medicine. 1994 Sep:28(3):177-9 [PubMed PMID: 8000816]
Ringel SP, Treihaft M, Carry M, Fisher R, Jacobs P. Suprascapular neuropathy in pitchers. The American journal of sports medicine. 1990 Jan-Feb:18(1):80-6 [PubMed PMID: 2154138]
Level 3 (low-level) evidencePester JM, Hendrix JM, Varacallo M. Brachial Plexus Block Techniques. StatPearls. 2024 Jan:(): [PubMed PMID: 29262036]
Cummins CA, Schneider DS. Peripheral nerve injuries in baseball players. Physical medicine and rehabilitation clinics of North America. 2009 Feb:20(1):175-93, x. doi: 10.1016/j.pmr.2008.10.007. Epub [PubMed PMID: 19084770]
Aiello I, Serra G, Traina GC, Tugnoli V. Entrapment of the suprascapular nerve at the spinoglenoid notch. Annals of neurology. 1982 Sep:12(3):314-6 [PubMed PMID: 7137969]
Level 3 (low-level) evidenceBencardino JT, Rosenberg ZS. Entrapment neuropathies of the shoulder and elbow in the athlete. Clinics in sports medicine. 2006 Jul:25(3):465-87, vi-vii [PubMed PMID: 16798138]
Piasecki DP, Romeo AA, Bach BR Jr, Nicholson GP. Suprascapular neuropathy. The Journal of the American Academy of Orthopaedic Surgeons. 2009 Nov:17(11):665-76 [PubMed PMID: 19880677]
Maquieira GJ, Gerber C, Schneeberger AG. Suprascapular nerve palsy after the Latarjet procedure. Journal of shoulder and elbow surgery. 2007 Mar-Apr:16(2):e13-5 [PubMed PMID: 17399619]
Level 3 (low-level) evidenceCarroll KW, Helms CA, Otte MT, Moellken SM, Fritz R. Enlarged spinoglenoid notch veins causing suprascapular nerve compression. Skeletal radiology. 2003 Feb:32(2):72-7 [PubMed PMID: 12589484]
Level 3 (low-level) evidenceVastamäki M, Göransson H. Suprascapular nerve entrapment. Clinical orthopaedics and related research. 1993 Dec:(297):135-43 [PubMed PMID: 8242921]
Level 3 (low-level) evidenceTirman PF, Feller JF, Janzen DL, Peterfy CG, Bergman AG. Association of glenoid labral cysts with labral tears and glenohumeral instability: radiologic findings and clinical significance. Radiology. 1994 Mar:190(3):653-8 [PubMed PMID: 8115605]
Level 2 (mid-level) evidenceMoore TP, Fritts HM, Quick DC, Buss DD. Suprascapular nerve entrapment caused by supraglenoid cyst compression. Journal of shoulder and elbow surgery. 1997 Sep-Oct:6(5):455-62 [PubMed PMID: 9356935]
Level 2 (mid-level) evidencePolguj M, Podgórski M, Jędrzejewski K, Topol M. The double suprascapular foramen: unique anatomical variation and the new hypothesis of its formation. Skeletal radiology. 2012 Dec:41(12):1631-6. doi: 10.1007/s00256-012-1460-z. Epub 2012 Jun 22 [PubMed PMID: 22722309]
Level 3 (low-level) evidenceRengachary SS, Burr D, Lucas S, Hassanein KM, Mohn MP, Matzke H. Suprascapular entrapment neuropathy: a clinical, anatomical, and comparative study. Part 2: anatomical study. Neurosurgery. 1979 Oct:5(4):447-51 [PubMed PMID: 534048]
Level 2 (mid-level) evidenceAvery BW, Pilon FM, Barclay JK. Anterior coracoscapular ligament and suprascapular nerve entrapment. Clinical anatomy (New York, N.Y.). 2002 Nov:15(6):383-6 [PubMed PMID: 12373728]
Polguj M, Jędrzejewski KS, Podgórski M, Topol M. Correlation between morphometry of the suprascapular notch and anthropometric measurements of the scapula. Folia morphologica. 2011 May:70(2):109-15 [PubMed PMID: 21630232]
Polguj M, Majos A, Waszczykowski M, Fabiś J, Stefańczyk L, Podgórski M, Topol M. A computed tomography study on the correlation between the morphometry of the suprascapular notch and anthropometric measurements of the scapula. Folia morphologica. 2016:75(1):87-92. doi: 10.5603/FM.a2015.0072. Epub 2015 Sep 14 [PubMed PMID: 26365856]
Demirhan M, Imhoff AB, Debski RE, Patel PR, Fu FH, Woo SL. The spinoglenoid ligament and its relationship to the suprascapular nerve. Journal of shoulder and elbow surgery. 1998 May-Jun:7(3):238-43 [PubMed PMID: 9658348]
Duparc F, Coquerel D, Ozeel J, Noyon M, Gerometta A, Michot C. Anatomical basis of the suprascapular nerve entrapment, and clinical relevance of the supraspinatus fascia. Surgical and radiologic anatomy : SRA. 2010 Mar:32(3):277-84. doi: 10.1007/s00276-010-0631-7. Epub 2010 Feb 21 [PubMed PMID: 20309668]
Plancher KD, Peterson RK, Johnston JC, Luke TA. The spinoglenoid ligament. Anatomy, morphology, and histological findings. The Journal of bone and joint surgery. American volume. 2005 Feb:87(2):361-5 [PubMed PMID: 15687160]
Martin SD, Warren RF, Martin TL, Kennedy K, O'Brien SJ, Wickiewicz TL. Suprascapular neuropathy. Results of non-operative treatment. The Journal of bone and joint surgery. American volume. 1997 Aug:79(8):1159-65 [PubMed PMID: 9278075]
Level 2 (mid-level) evidencePlancher KD, Luke TA, Peterson RK, Yacoubian SV. Posterior shoulder pain: a dynamic study of the spinoglenoid ligament and treatment with arthroscopic release of the scapular tunnel. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007 Sep:23(9):991-8 [PubMed PMID: 17868839]
Lafosse L, Piper K, Lanz U. Arthroscopic suprascapular nerve release: indications and technique. Journal of shoulder and elbow surgery. 2011 Mar:20(2 Suppl):S9-13. doi: 10.1016/j.jse.2010.12.003. Epub [PubMed PMID: 21281924]
Bateman JE. Nerve injuries about the shoulder in sports. The Journal of bone and joint surgery. American volume. 1967 Jun:49(4):785-92 [PubMed PMID: 6026011]
Dididze M, Jimsheleishvili S, Ward WB, Ramos-Vargas KE. Spinal Accessory and Suprascapular Nerve Injury After Human Bite. American journal of physical medicine & rehabilitation. 2021 Jan 1:100(1):e1-e3. doi: 10.1097/PHM.0000000000001472. Epub [PubMed PMID: 32452882]
Gereli A, Uslu S, Okur B, Ulku TK, Kocaoğlu B, Yoo YS. Effect of suprascapular nerve injury on rotator cuff enthesis. Journal of shoulder and elbow surgery. 2020 Aug:29(8):1584-1589. doi: 10.1016/j.jse.2019.12.028. Epub 2020 Mar 18 [PubMed PMID: 32199756]
Faruch Bilfeld M, Lapègue F, Sans N, Chiavassa Gandois H, Laumonerie P, Larbi A. Ultrasonography study of the suprascapular nerve. Diagnostic and interventional imaging. 2017 Dec:98(12):873-879. doi: 10.1016/j.diii.2017.09.003. Epub 2017 Nov 6 [PubMed PMID: 29102312]
Reimers K, Reimers CD, Wagner S, Paetzke I, Pongratz DE. Skeletal muscle sonography: a correlative study of echogenicity and morphology. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 1993 Feb:12(2):73-7 [PubMed PMID: 8468739]
Gorthi V, Moon YL, Kang JH. The effectiveness of ultrasonography-guided suprascapular nerve block for perishoulder pain. Orthopedics. 2010 Apr:33(4):. doi: 10.3928/01477447-20100225-11. Epub 2010 Apr 16 [PubMed PMID: 20415302]
Level 1 (high-level) evidenceDrez D Jr. Suprascapular neuropathy in the differential diagnosis of rotator cuff injuries. The American journal of sports medicine. 1976 Mar-Apr:4(2):43-5 [PubMed PMID: 961967]
Level 3 (low-level) evidencePingree MJ, Hurdle MF, Spinner DA, Valimahomed A, Crosby ND, Boggs JW. Real-world evidence of sustained improvement following 60-day peripheral nerve stimulation treatment for pain: a cross-sectional follow-up survey. Pain management. 2022 Jul:12(5):611-621. doi: 10.2217/pmt-2022-0005. Epub 2022 May 5 [PubMed PMID: 35510333]
Level 2 (mid-level) evidencePost M. Diagnosis and treatment of suprascapular nerve entrapment. Clinical orthopaedics and related research. 1999 Nov:(368):92-100 [PubMed PMID: 10613156]
Level 2 (mid-level) evidencePost M, Grinblat E. Suprascapular nerve entrapment: Diagnosis and results of treatment. Journal of shoulder and elbow surgery. 1993 Jul:2(4):190-7. doi: 10.1016/1058-2746(93)90062-L. Epub 2009 Feb 25 [PubMed PMID: 22971734]
Lafosse L, Tomasi A, Corbett S, Baier G, Willems K, Gobezie R. Arthroscopic release of suprascapular nerve entrapment at the suprascapular notch: technique and preliminary results. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007 Jan:23(1):34-42 [PubMed PMID: 17210425]
Schroder CP, Skare O, Stiris M, Gjengedal E, Uppheim G, Brox JI. Treatment of labral tears with associated spinoglenoid cysts without cyst decompression. The Journal of bone and joint surgery. American volume. 2008 Mar:90(3):523-30. doi: 10.2106/JBJS.F.01534. Epub [PubMed PMID: 18310702]
Costouros JG, Porramatikul M, Lie DT, Warner JJ. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007 Nov:23(11):1152-61 [PubMed PMID: 17986401]
Level 2 (mid-level) evidencePiatt BE, Hawkins RJ, Fritz RC, Ho CP, Wolf E, Schickendantz M. Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. Journal of shoulder and elbow surgery. 2002 Nov-Dec:11(6):600-4 [PubMed PMID: 12469086]
Tuckman GA, Devlin TC. Axillary nerve injury after anterior glenohumeral dislocation: MR findings in three patients. AJR. American journal of roentgenology. 1996 Sep:167(3):695-7 [PubMed PMID: 8751683]
Kim DH, Murovic JA, Tiel RL, Kline DG. Management and outcomes of 42 surgical suprascapular nerve injuries and entrapments. Neurosurgery. 2005 Jul:57(1):120-7; discussion 120-7 [PubMed PMID: 15987547]
Level 2 (mid-level) evidenceTakeda S, Tatebe M, Morita A, Saka N, Iwatsuki K, Hirata H. Transfer of the Lower Trapezius as a Surgical Treatment for Combined Injuries to the Suprascapular and Axillary Nerves: A Case Report. Journal of orthopaedic case reports. 2019:9(2):56-59. doi: 10.13107/jocr.2250-0685.1370. Epub [PubMed PMID: 31534936]
Level 3 (low-level) evidence