Introduction
The human body is capable of perceiving five traditional senses: hearing, sight, smell, touch, and taste. Also known as gustation, the sense of taste is essential in discerning the characteristics of substances that one ingests. At a basic evolutionary level, taste allows one to assess whether ingested substances are nutritious or potentially hazardous. This sensation is primarily relayed via receptors located on the tongue. However, at a higher cortical level, taste is considered a multisensory experience as smell, texture, and activation of specific receptors (eg, pain receptors from spicy food) all play a role in determining how something "tastes."[1]
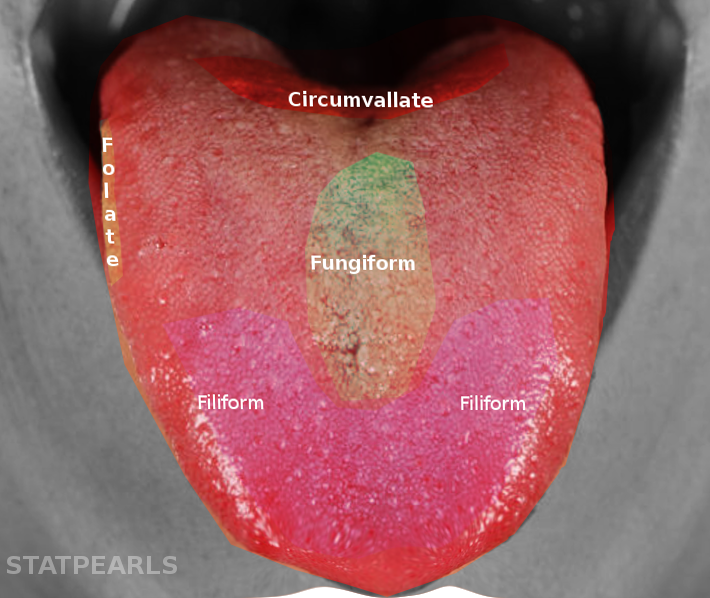
A fundamental working knowledge of the anatomy of the tongue is important in fully understanding the concept of taste. The human tongue is divided into an anterior two-thirds and a posterior one-third, separated by a v-shaped groove called the sulcus terminalis. The dorsal aspect of the tongue is covered with bumps known as papillae, of which there are four types: circumvallate, fungiform, foliate, and filiform. The circumvallate, fungiform, and foliate papillae contain taste buds known as gustatory papillae.[2] Taste buds are found on the tongue and the pharynx, larynx, soft palate, and epiglottis.
The circumvallate papillae are on the distal aspect of the anterior two-thirds of the tongue and are most sensitive to bitter tastes. The fungiform papillae are found on the tip of the tongue and are most sensitive to sweet and savory (umami) tastes. The foliate papillae are found on the sides of the tongue and are most sensitive to salty and sour tastes.[3] Filiform papillae are found throughout the entire surface of the dorsal tongue and do not contain taste buds. The rough texture of the filiform papillae aid in the gripping of food and transfer down to the esophagus, as well as in the cleaning of the mouth and spreading of saliva.[4]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
How something tastes is not a one-size-fits-all phenomenon. Previous exposure, personal experience, cultural preferences, hormones, and genetic variations can all affect the taste and consumption of food. As previously mentioned, the ability to taste something is also modulated by smell (olfaction) and oral textual perception. As individuals age, there is a reduction in the number of taste buds and papillae, and a reduced neural responsiveness to taste, which may change an individual's perception of, and preference for, certain foods.[5]
Other factors that affect taste include hunger, which increases the sensitivity to sweet, sour, and salty flavors, while satiated individuals tend to show increased sensitivity to bitter tastes.[6] Additionally, upper respiratory infections and allergies decrease sensitivity to taste.
There are five well-known basic types of taste: sweet, salty, sour, bitter, and savory (umami). However, over the past 20+ years, numerous studies have demonstrated a sixth basic taste, known as "oleogustus," or the taste of lipids (fats).[7]
Cellular Level
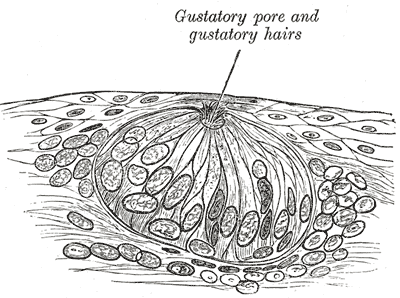
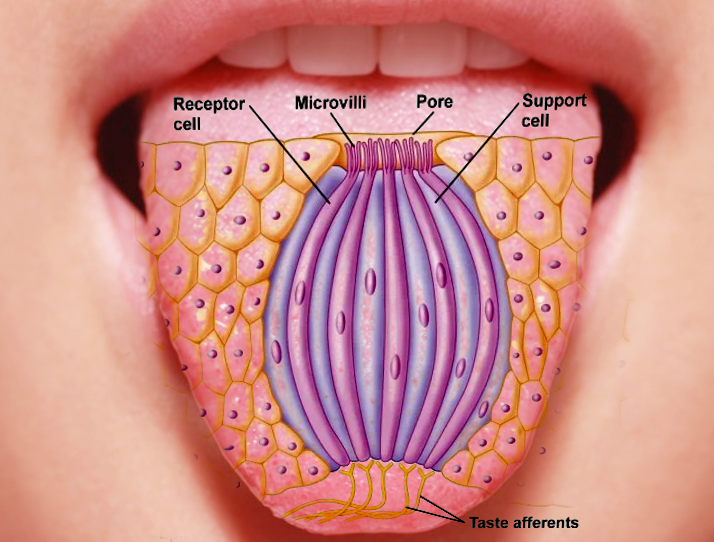
Taste is sensed by chemosensory receptors known as taste buds. Taste buds contain basal cells, which differentiate into taste receptor cells (TRCs) and perceive taste. TRCs have thin microvilli (gustatory hairs) which protrude out the top. The TRCs contain axons, which send taste signals to the brain. TRCs on the anterior two-thirds of the tongue send signals to the brain via the chorda tympani branch of the facial nerve (CN VII). TRCs on the posterior one-third and throughout the oral cavity send signals to the brain via the glossopharyngeal nerve (CN IX). TRCs found on the back of the throat and the esophagus send signals to the brain via the vagus nerve (CN X).[8]
The perception of taste begins when food substances are chewed, mixed with saliva, and travel to papillae, where they make contact with gustatory hairs located on the top of taste pores. Apical ion channels detect salty and sour tastes, while bitter, sweet, and umami tastes are detected by G protein-coupled receptors (GPCRs).[9] The perception of sweet flavors is in response to sugars and sweeteners. Sour tastes come from free H+ ions (acids), bitter tastes are due to alkaloids, salty tastes are due to Na+ ions, and umami tastes are from glutamate and other L-amino acids.[9]
Development
The human tongue consists of two parts; an anterior-two third and a posterior one-third, separated by a shallow v-shaped groove called the terminal sulcus. The development of the tongue occurs via the first four pharyngeal arches and begins at week four of gestation. The anterior two-thirds of the tongue is developed from the mesenchyme of the first pharyngeal arch, which forms a medial swelling known as the tuberculum impar.
Two lateral lingual swellings grow from the same pharyngeal arch in the fifth week of gestation. The lateral lingual swellings increase in size and eventually grow over the tuberculum impar, merging in the midline to form the median sulcus and, ultimately, the anterior two-thirds of the tongue. The second pharyngeal arch forms the initial growth of the posterior one-third of the tongue, referred to as the copula. The third and fourth pharyngeal arches form another median swelling known as the hypobranchial eminence.
Taste bud development first occurs during the eighth week of gestation and typically finishes around week 13.[10] Taste bud activation begins during the 30th week of gestation, at which time the composition of the amniotic fluid is varied based on the mother's diet and stimulates fetal taste receptors.[11]
Organ Systems Involved
Gustation is not a standalone sensation. The olfactory system, including the nose, olfactory bulb, and olfactory cortex, are major players in how an individual perceives a taste.[12] This is evident when one has a cold or other nasal obstruction and tastes seem blunted. Or, for example, when you plug your nose while chewing something that tastes bad to blunt the taste. The peripheral and central nervous systems are also involved in gustation, including the cranial nerves VII, IX, and X and the amygdala, thalamus, and hypothalamus.
Function
The function of taste, and taste buds, specifically, is to take chemical stimuli and transduce them into a nervous signal which the brain can then interpret. In this way, our brain decides whether to ingest the food or spit it out if it is deemed unpalatable or potentially toxic.[13]
Taste sensation can change according to the body’s specific nutritional needs at different times, guiding an organism to particular sources of nutrients needed. For example, salt-depleted animals in which an adrenalectomy has been performed will choose to drink water with a higher salt content to replenish their body stores.[14]
As mentioned earlier, specific fundamental characteristics of taste, such as bitterness, may denote a harmful or poisonous substance, and thus, would make one consciously aware and may prevent ingestion. Once taste signals reach the central nervous system; multiple reflex pathways are activated, leading the body to prepare for a meal, with increased salivation and elevated secretory activity in the stomach.[15]
Mechanism
The mechanism of taste signals converting from the form of a chemical stimulus to electrical impulses for transmission to the brain requires specific ion channels and second messenger systems. The type of system utilized for transduction depends upon the taste itself.[16] As previously mentioned, salty and sour tastes are detected by apical ion channels, while bitter, sweet, and umami tastes are detected by G protein-coupled receptors (GPCRs).
Salty and Sour Tastes
Na+ and H+ ions found in salty and sour foods, respectively, come into contact with the taste pores and their gustatory hairs. The ions bind to their specific receptors on a taste receptor cell (TRC) within the taste bud, triggering an intracellular cascade. The cell membrane depolarizes, and voltage-gated channels open.[17] Extracellular calcium flows inside the cell, triggering the release of neurotransmitters from the cell and into the synaptic cleft, where taste information is then taken to the brain via the associated cranial nerve.[18]
Sweet, Bitter, and Umami Tastes
The sugar, alkaloids, or L-amino acids bind to a GPCR and trigger a common signaling pathway. Once activated, these GPCRs activate a phospholipase C (PLC) pathway. Inositol triphosphate (IP3) receptors are activated through this pathway, releasing calcium from its endoplasmic reticulum stores. This calcium release causes membrane depolarization via sodium influx, releasing neurotransmitters. Taste information is then taken to the brain via the associated cranial nerve.[18]
The chorda tympani branch of the facial nerve, the glossopharyngeal nerve, and the vagus nerve all transmit their information to the nucleus tractus solitorius (NTS) of the medulla. From here, information is sent to the ventral posteromedial nucleus (VPM) of the thalamus and then to an area of the postcentral gyrus hidden by the lateral sulcus. The lateral hypothalamus and the central nucleus of the amygdala also receive gustatory information and are involved in the emotional component of taste, such as the memory of taste, and play a role in ingestive behavior.[19]
Related Testing
Taste testing involves assessing gustatory and olfactory functions. In some rare cases, imaging or electrogustometry is necessary.[20] Gustatory testing can involve spatial tests, taste sticks, and tasting tablets. Olfactory testing commonly involves using the UPSIT (University of Pennsylvania Smell Identification Test) or an odor probe.[21]
Imaging may be helpful if there is a concern for mass lesions affecting the taste pathway, and bacterial culture may be done if there is clinical suspicion of infection leading to taste dysfunction.
Pathophysiology
The sense of taste may be affected by numerous clinical conditions that affect the tongue itself, the neural pathways, or the brain. Taste dysfunction due to papillae loss or damage can occur due to nutritional deficiencies (pernicious anemia, iron-deficiency anemia), therapeutic agents (radiation/chemotherapy, anticholinergic drugs), peripheral vascular disease (lupus vasculitis, diabetic angiopathy), or by local factors (frictional irritation, long-standing xerostomia, or atrophic lichen planus).[22] Taste dysfunction can also be seen in patients with AIDS [23] and those suffering from mental disorders such as schizophrenia.[24] Impairment of smell can also negatively impact taste perception, as mentioned above.
Taste dysfunction (dysgeusia) can be categorized as hypergeusia, hypogeusia, or ageusia. Hypergeusia, while extremely rare, is an abnormally heightened taste sensitivity and can be the presenting symptom of a posterior cranial fossa lesion.[25] Hypogeusia is characterized by a decreased sense of taste; it can be caused by anything from a self-limiting upper respiratory infection to chemotherapy, Bell palsy, drug use, or numerous other neuronal dysfunctions. Ageusia is a complete loss of taste and can be due to damage to any of the three cranial nerves associated with gustation (CN VII, IX, X), dietary deficiencies, or numerous systemic conditions.[26]
As previously mentioned, genetics can play a role in our ability to taste food and how we perceive what we taste. There is a phenomenon in which some individuals are especially sensitive to bitter taste, termed supertasters, and some individuals who taste very little or no bitterness, termed non-tasters. The majority of individuals fit somewhere in the middle. The concept of supertasters originated in the 1980s in the lab of experimental psychologist Dr. Linda Bartoshuk, who specializes in genetic variations in taste perception. In her experiments on taste, Dr. Bartoshuk placed a bitter-tasting chemical called 6-n-propylthiouracil (PROP) on the tongue of individuals and found that approximately 25% were extremely sensitive to the bitter taste. In comparison, another 25% could not taste it, with the rest of the population, roughly 50%, residing somewhere in the middle and only tasting a faint bitterness.[27]
The reasoning behind this ability to perceive bitterness differently is attributed to papillae. Supertasters visibly have more papillae, meaning they have more taste cells and receptors for bitterness. Additionally, but to a lesser extent, supertasters are more sensitive to salty, sweet, and umami tastes.[28]
Another interesting concept in taste involves Synsepalum dulcificum, a plant native to Central and West Africa. This plant contains a berry that, when eaten, causes sour foods, such as lemons, to taste sweet. This phenomenon is due to a glycoprotein in the plant's fruit, miraculin, which binds to sweet taste receptors and causes acidic foods to be perceived as sweet tasting. This effect can last from 20 minutes to one hour.[29]
Clinical Significance
When patients present for evaluation of taste loss, in most cases, a loss of smell will be found, leading to a loss of taste. Distortions in taste are typically present due to another underlying cause, such as medications or infections. On its own, a presenting complaint of loss of taste has little diagnostic value and is difficult to treat unless the underlying cause is treated.[30]
Taste loss is associated with decreased appetite and food intake, especially in patients who have undergone radiotherapy for malignancy; this can increase the risk of cancer cachexia and severe weight loss and negatively impact the overall prognosis.[31] Adenoid hypertrophy in children links with olfactory disturbance, which can cause a lack of taste appreciation.[32] Nutritional zinc deficiency has been demonstrated to cause taste loss, with studies finding that zinc deficiency was associated with varying degrees of taste abnormalities and that zinc supplementation usually produced improvement in these abnormalities.[33] Taste distortion may also be a side effect of many drugs, such as the antifungals griseofulvin and terbinafine, and antihypertensive agents, such as angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers.[34] The antibiotic metronidazole is also associated with a metallic taste disturbance. Clinicians need to be aware of these side effects when prescribing medications, so they can convey accurate information to their patients and provide better care. Taste has a logical connection to overeating and obesity.[35] Obesity, being linked to diabetes, cardiovascular disease, and other causes of morbidity and mortality, has quickly become a global health concern, with about 39% of the world's population considered to be overweight or clinically obese in 2018, a number that has undoubtedly grown significantly.[36] Studies have found that abnormalities in the central response to taste can develop in individuals who suffer from obesity and can be responsible for developing unhealthy eating patterns that can exacerbate obesity and difficulty in losing weight and maintaining weight loss in previously obese individuals.[37] Taste has been an often ignored sensory modality, considered not as crucial as other senses, and patients may often decline to disclose whether they have taste disorders spontaneously. The question "Do you have a taste problem?" was only able to identify 10% of patients with taste problems. Clinicians must directly approach this topic with patients and ask specific closed-ended questions to ensure appropriate history-taking.[38] Because of the plethora of potential etiologies of loss of taste, it can be challenging to diagnose a taste disorder. However, further probing patients regarding their symptoms, such as a change in taste, can lead to further implications such as loss of appetite, weight loss, malnutrition, and ultimately a poorer quality of life. Ninety-five percent of taste disorders have been shown to be caused by an impairment of smell rather than a loss of taste, so it is of extreme importance to clinically evaluate for olfactory dysfunction.
Additionally, head trauma, cognitive impairments, and Parkinson disease should be ruled out as a cause of loss of smell or taste, and medication reconciliation should be performed to see if any medications the patient is taking could be the cause. Approximately 50% of patients with olfactory dysfunction will improve over time, with improvement inversely correlated with the severity and duration of loss of smell, a patient's age, smoking status, and male sex.[39]
Media
(Click Image to Enlarge)
References
Schiffman SS, Gatlin CA. Clinical physiology of taste and smell. Annual review of nutrition. 1993:13():405-36 [PubMed PMID: 8369152]
Jung HS, Akita K, Kim JY. Spacing patterns on tongue surface-gustatory papilla. The International journal of developmental biology. 2004:48(2-3):157-61 [PubMed PMID: 15272380]
Level 3 (low-level) evidenceSpence C. The tongue map and the spatial modulation of taste perception. Current research in food science. 2022:5():598-610. doi: 10.1016/j.crfs.2022.02.004. Epub 2022 Mar 18 [PubMed PMID: 35345819]
Wong P, Colucci-Guyon E, Takahashi K, Gu C, Babinet C, Coulombe PA. Introducing a null mutation in the mouse K6alpha and K6beta genes reveals their essential structural role in the oral mucosa. The Journal of cell biology. 2000 Aug 21:150(4):921-8 [PubMed PMID: 10953016]
Level 3 (low-level) evidenceRisso D, Drayna D, Morini G. Alteration, Reduction and Taste Loss: Main Causes and Potential Implications on Dietary Habits. Nutrients. 2020 Oct 27:12(11):. doi: 10.3390/nu12113284. Epub 2020 Oct 27 [PubMed PMID: 33120898]
Hanci D, Altun H. Hunger state affects both olfactory abilities and gustatory sensitivity. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2016 Jul:273(7):1637-41. doi: 10.1007/s00405-015-3589-6. Epub 2015 Mar 6 [PubMed PMID: 25744049]
Gaillard D, Kinnamon SC. New evidence for fat as a primary taste quality. Acta physiologica (Oxford, England). 2019 May:226(1):e13246. doi: 10.1111/apha.13246. Epub 2019 Jan 16 [PubMed PMID: 30588748]
Level 2 (mid-level) evidenceObiefuna S, Donohoe C. Neuroanatomy, Nucleus Gustatory. StatPearls. 2023 Jan:(): [PubMed PMID: 32119409]
Kinnamon SC. Taste receptor signalling - from tongues to lungs. Acta physiologica (Oxford, England). 2012 Feb:204(2):158-68. doi: 10.1111/j.1748-1716.2011.02308.x. Epub 2011 May 7 [PubMed PMID: 21481196]
Level 3 (low-level) evidenceJain P, Rathee M. Embryology, Tongue. StatPearls. 2024 Jan:(): [PubMed PMID: 31613477]
Paglia L. Taste development and prenatal prevention. European journal of paediatric dentistry. 2019 Dec:20(4):257. doi: 10.23804/ejpd.2019.20.04.01. Epub [PubMed PMID: 31850766]
Kakutani Y, Narumi T, Kobayakawa T, Kawai T, Kusakabe Y, Kunieda S, Wada Y. Taste of breath: the temporal order of taste and smell synchronized with breathing as a determinant for taste and olfactory integration. Scientific reports. 2017 Aug 21:7(1):8922. doi: 10.1038/s41598-017-07285-7. Epub 2017 Aug 21 [PubMed PMID: 28827648]
Roper SD, Chaudhari N. Taste buds: cells, signals and synapses. Nature reviews. Neuroscience. 2017 Aug:18(8):485-497. doi: 10.1038/nrn.2017.68. Epub 2017 Jun 29 [PubMed PMID: 28655883]
NACHMAN M. Taste preferences for sodium salts by adrenalectomized rats. Journal of comparative and physiological psychology. 1962 Dec:55():1124-9 [PubMed PMID: 13937025]
Level 3 (low-level) evidenceUneyama H, Kawai M, Sekine-Hayakawa Y, Torii K. Contribution of umami taste substances in human salivation during meal. The journal of medical investigation : JMI. 2009:56 Suppl():197-204 [PubMed PMID: 20224181]
Gilbertson TA. The physiology of vertebrate taste reception. Current opinion in neurobiology. 1993 Aug:3(4):532-9 [PubMed PMID: 7693091]
Level 3 (low-level) evidenceRamos Da Conceicao Neta ER, Johanningsmeier SD, McFeeters RF. The chemistry and physiology of sour taste--a review. Journal of food science. 2007 Mar:72(2):R33-8 [PubMed PMID: 17995849]
Medler KF. Calcium signaling in taste cells. Biochimica et biophysica acta. 2015 Sep:1853(9):2025-32. doi: 10.1016/j.bbamcr.2014.11.013. Epub 2014 Nov 16 [PubMed PMID: 25450977]
Level 3 (low-level) evidenceLi CS, Cho YK, Smith DV. Modulation of parabrachial taste neurons by electrical and chemical stimulation of the lateral hypothalamus and amygdala. Journal of neurophysiology. 2005 Mar:93(3):1183-96 [PubMed PMID: 15483060]
Level 3 (low-level) evidenceWrobel BB, Leopold DA. Clinical assessment of patients with smell and taste disorders. Otolaryngologic clinics of North America. 2004 Dec:37(6):1127-42 [PubMed PMID: 15563906]
Kronenbuerger M, Pilgramm M. Olfactory Testing. StatPearls. 2023 Jan:(): [PubMed PMID: 33351420]
Khan AM, Ali S, Jameela RV, Muhamood M, Haqh MF. Impact of Fungiform Papillae Count on Taste Perception and Different Methods of Taste Assessment and their Clinical Applications: A comprehensive review. Sultan Qaboos University medical journal. 2019 Aug:19(3):e184-e191. doi: 10.18295/squmj.2019.19.03.003. Epub 2019 Nov 5 [PubMed PMID: 31728215]
Henn IW, da Silva RO, Chaiben CL, Fernandes Â, Naval Machado MÂ, de Lima AA. Perception of taste in HIV-positive individuals in treatment antiretroviral: results of a case-control study. Special care in dentistry : official publication of the American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry. 2017 Jan:37(1):3-9. doi: 10.1111/scd.12186. Epub 2016 Apr 26 [PubMed PMID: 27112098]
Level 2 (mid-level) evidenceWroński M, Samochowiec J, Pełka-Wysiecka J, Liśkiewicz P, Bieńkowski P, Misiak B. Deficit Symptomatology of Schizophrenia Is Associated with Attenuated Taste Identification: Findings from a Cross-Sectional Study. Brain sciences. 2022 Nov 9:12(11):. doi: 10.3390/brainsci12111520. Epub 2022 Nov 9 [PubMed PMID: 36358446]
Level 2 (mid-level) evidenceNoda S, Hiromatsu K, Umezaki H, Yoneda S. Hypergeusia as the presenting symptom of a posterior fossa lesion. Journal of neurology, neurosurgery, and psychiatry. 1989 Jun:52(6):804-5 [PubMed PMID: 2545829]
Level 3 (low-level) evidenceRathee M, Jain P. Ageusia. StatPearls. 2024 Jan:(): [PubMed PMID: 31747182]
Bartoshuk LM. Genetic and pathological taste variation: what can we learn from animal models and human disease? Ciba Foundation symposium. 1993:179():251-62; discussion 262-7 [PubMed PMID: 8168379]
Level 3 (low-level) evidenceDiószegi J, Llanaj E, Ádány R. Genetic Background of Taste Perception, Taste Preferences, and Its Nutritional Implications: A Systematic Review. Frontiers in genetics. 2019:10():1272. doi: 10.3389/fgene.2019.01272. Epub 2019 Dec 19 [PubMed PMID: 31921309]
Level 1 (high-level) evidenceAkinmoladun AC, Adetuyi AR, Komolafe K, Oguntibeju OO. Nutritional benefits, phytochemical constituents, ethnomedicinal uses and biological properties of Miracle fruit plant (Synsepalum dulcificum Shumach. & Thonn. Daniell). Heliyon. 2020 Dec:6(12):e05837. doi: 10.1016/j.heliyon.2020.e05837. Epub 2020 Dec 29 [PubMed PMID: 33426338]
Douglas JE, Mansfield CJ, Arayata CJ, Cowart BJ, Colquitt LR, Maina IW, Blasetti MT, Cohen NA, Reed DR. Taste Exam: A Brief and Validated Test. Journal of visualized experiments : JoVE. 2018 Aug 17:(138):. doi: 10.3791/56705. Epub 2018 Aug 17 [PubMed PMID: 30176005]
Stewart GD, Skipworth RJ, Fearon KC. Cancer cachexia and fatigue. Clinical medicine (London, England). 2006 Mar-Apr:6(2):140-3 [PubMed PMID: 16688969]
Konstantinidis I, Triaridis S, Triaridis A, Petropoulos I, Karagiannidis K, Kontzoglou G. How do children with adenoid hypertrophy smell and taste? Clinical assessment of olfactory function pre- and post-adenoidectomy. International journal of pediatric otorhinolaryngology. 2005 Oct:69(10):1343-9 [PubMed PMID: 15907344]
Henkin RI. Zinc in taste function : A critical review. Biological trace element research. 1984 Jun:6(3):263-80. doi: 10.1007/BF02917511. Epub [PubMed PMID: 24264025]
Doty RL, Shah M, Bromley SM. Drug-induced taste disorders. Drug safety. 2008:31(3):199-215 [PubMed PMID: 18302445]
Drewnowski A, Kurth CL, Rahaim JE. Taste preferences in human obesity: environmental and familial factors. The American journal of clinical nutrition. 1991 Oct:54(4):635-41 [PubMed PMID: 1897470]
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism: clinical and experimental. 2019 Mar:92():6-10. doi: 10.1016/j.metabol.2018.09.005. Epub 2018 Sep 22 [PubMed PMID: 30253139]
Nasser J. Taste, food intake and obesity. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2001 Nov:2(4):213-8 [PubMed PMID: 12119992]
Gent JF, Goodspeed RB, Zagraniski RT, Catalanotto FA. Taste and smell problems: validation of questions for the clinical history. The Yale journal of biology and medicine. 1987 Jan-Feb:60(1):27-35 [PubMed PMID: 3564547]
Level 1 (high-level) evidenceMalaty J, Malaty IA. Smell and taste disorders in primary care. American family physician. 2013 Dec 15:88(12):852-9 [PubMed PMID: 24364550]